Indications and contraindications for this surgery are the same as for any laparoscopic approach and for midline hernias. Obesity and cardiovascular diseases, as well as respiratory problems, are considered risk factors for postoperative morbidity. The hernia defect must be taken into account, since it is related directly to the conversion and recurrence rate, this last one being much higher for defects larger than 10 cm in diameter.
Common Surgical Management
Preoperative management is common for all of these hernias. Preoperative imaging (CT scan preferred) is recommended in order to correctly localize the defect, measure it, and confirm the diagnosis in some cases. Informed consent must be collected; preanesthetic evaluation and ASA classification are mandatory.
Surgical repair will start with the patient in the supine position, securely attached to the operating table, which facilitates the different movements and positions. General anesthesia is used in all patients. The placement of the nasogastric catheter is not necessary except when important distension of the stomach is observed. Prior to surgery, and with the patient in a standing position and also in a supine position, the edges of the defect as well as most significant anatomical marks (including bone reliefs and the size of the hernia sac or sacs in case of multiplicity) should be drawn on the abdominal wall with a dermographic marker. We believe that the real measurement of the defect is an important consideration during the visceral dissection and also for the choice and size of the prosthesis and the orientation of the mesh.
Pneumoperitoneum is systematically performed by the insertion of a Veress needle at the left point of Palmer except in cases of subcostal hernia on that side, in which case this will be made periumbilical. We have not had further complications regarding this maneuver. The working pressure is initially set on 14 mmHg.
Subxiphoid Hernia
It was not until the beginning of the twenty-first century (after the publication by Muysoms et al. [6]) that subxiphoid hernias were considered an independent pathology. It has different characteristics from other incisional hernias. The hernia sac is very close to bony margins, increasing the tension, and close to neurovascular structures. These hernias usually develop in patients that might have important comorbidities and surgical interventions, such as cardiac surgery (especially transplant) and bilio-pancreatic and esophagogastric surgeries, which may need bilateral subcostal incisions, high midline incisions, or a combination of them.
As this type of hernia is not very well defined and has a low report rate in scientific literature, its incidence varies from 2 to 4.2 %, especially after a sternotomy, although this incidence might be underestimated, because in up to 89 % of the cases, no incarceration is present, so the patient could have experienced the hernia much earlier with no further symptoms but cosmesis. Risk factors for the development of these hernias are left cardiac failure, male patients, obesity, immunotherapy, and wound infection.
Indications for surgery must include all symptomatic hernias (but this is uncommon as less than 2 % present pain), but also cosmetic and preventive purposes.
Conventional surgery is difficult, and high rates of recurrence have been described; this is the reason why many different approaches have been described, without a formal recommendation.
Early publications mention simple closure of the defect, with recurrence rates from 43 to 80 %. This is the main reason, together with the anatomical difficulties and proximity to bony margins, why the surgical community shifted to the use of prosthetic materials, with lower recurrence rates of 0–32 %. Some authors like Carbonell et al. [7] propose the use of a double mesh. It is accepted, with no clear evidence, that the best repair would include the implantation of a parietal prosthesis, submuscular, with a minimum 5 cm overlap surrounding the perimeter of the defect. In this anatomical region, attention to the retro-xiphoid-sternal dissection as well as perixiphoid space, mainly cranially and towards the costal insertions, must be especially paid, in order to achieve enough overlap. Some publications present the use of fixation with sutures or prosthetic loops fixed to the costal arch. This use is contraindicated nowadays, due to the high rate of postoperative chronic pain caused by the damage of this fixation to the periosteum.
During the last decade, the open approach with the insertion of a retromuscular mesh (sublay) has been used, with recurrence rates higher than 50 % in some series; this has led to controversies in the approach. Laparoscopy is the main option for treatment in referral centers. This approach does not diminish recurrence rates significantly but results in less postoperative pain, better cosmetic results, shorter postoperative stays, and faster recovery times, as the start of normal activities has been seen earlier, which proves the benefits of minimally invasive surgery for this repair.
First publications about this laparoscopic approach date from 2000 and 2001. Still, up to this point in time, few references can be found, with short and heterogeneous series and limited follow-up. Most authors recommend the laparoscopic approach with the use of laminar or bilaminar meshes, ePTFE, or polypropylene/polyester with an antiadherent side and partial fixation of the prosthesis.
In summary, in the case of a subxiphoid hernia, we recommend the laparoscopic approach with the use of a prosthetic material placed intraperitoneally (IPOM).
This approach allows for an excellent view of the hernia margin, as well as the subfascial space, and also any associated unsuspected defects, and is considered as a safe and minimally invasive alternative.
Surgical Technique
Trocar placement is described in Fig. 12.2. The success of the repair depends upon ensuring an overlap >5 cm of the defect margin. Fixation can be made with helical metallic or resorbable sutures, as well as a combination of both, depending on the experience of the group and availability. Transfascial nonabsorbable sutures may also be used, alternatively. The fastening of the mesh in this region is especially difficult, especially in the cephalic portion, due to the proximity of the ribs, diaphragm, and the pericardium. Diaphragmatic injuries, pericardial tamponade, and even cases of cardiac tamponade (because of the use of helical sutures) formally discourage their use. A vast majority of authors, such as Eisenberg [8], recommend no fixation of the cephalic portion of the prosthesis and fixing only the caudal portion, leaving the intra-abdominal pressure, the liver, and the stomach to help protect the upper area. The development of effective biological adhesives, in the future, to help us solve this key problem will be necessary to achieve a safe repair of these hernias.
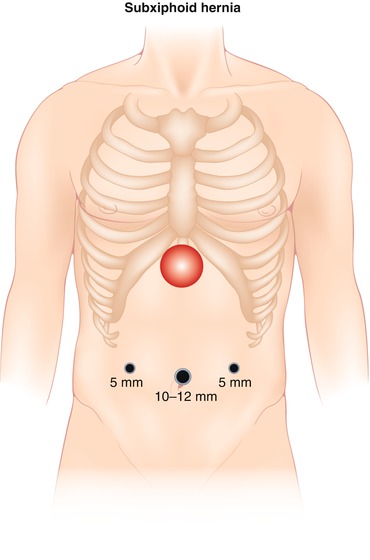
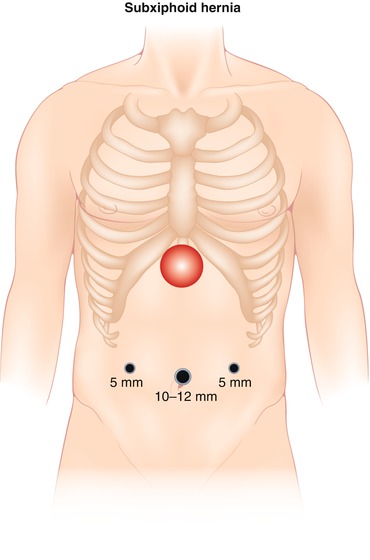
Fig. 12.2
Trocar placement in subxiphoid hernia
Our group performs the fixation following the double crown technique with metallic and absorbable tacks, in a proportion of 1:3. The limits for this are the costal arch and the diaphragm, where we use tissue adhesives (Tissucol Inmuno®, Baxter Healthcare, Deerfield, IL, USA) and absorbable sutures anchoring the mesh to the peritoneum/diaphragm with extracorporeal knotting. See Fig. 12.3.


Fig. 12.3
1 Measure of the defect. 2 Mesh with two strands for the transmural sutures
Major complications associated with this laparoscopic repair are visceral lesions during the adhesiolysis (often unknowingly), which cause high morbidity and mortality (which can be avoided following careful dissection without thermal energy), and the appearance of seroma, common to the abdominal wall prosthetic repair, which can be handled in the same manner as after hernia repair in other locations.
Subcostal Hernias
An incidence rate of 6–17 % for subcostal hernias can be found in literature, although it might be higher. Moreno-Egea and Carrillo-Alcaraz [2] describe rates as high as 25 % (including other lateral hernias such as lumbar and iliac hernias). Among their characteristics, very similar to subxiphoid defects, are having the costal arch as one of the limits on one side or the other and also presenting more diffuse hernia margins, compared to midline defects. This is the reason why published incidence rates are higher.
Standard treatment includes open repair, with mesh placement in the retromuscular space, with at least 3 cm overlap, which sometimes cannot be achieved due to the presence of the 10th or 11th rib as a limit. That is the reason why the laparoscopic approach is becoming more used lately, with intraperitoneal technique (IPOM) and transfascial or helical sutures.
A recent study published by Wassenaar et al. in 2009 [9] on 509 patients shows that the recurrence rate after laparoscopic incisional hernia repair occurs only when the principle of repairing the whole incision and prior hernia defect is omitted, regardless of the type of fixation used. This becomes of capital importance in the case of subcostal hernias since, as we have seen, subcostal defects are more diffuse and less fibrous edged. Therefore, we recommend the laparoscopic approach, which allows you to clearly identify the margins of the hernia, hidden defects, and areas of muscle weakness in the vicinity, which must necessarily be covered by the intraperitoneal prosthesis. Recurrence rates of 1.7 % as published by Wassenaar are described when applying these principles.
It is crucial to measure the whole defect, and the prosthesis size must include a total 5 cm defect overlap in all cases. Anchoring can be made as in subxiphoid hernias through transfascial sutures, helical sutures, or both. Fixing to the proximity of the ribs or intercostal spaces, which inevitably will result in postoperative pain, is not recommended. Fixing limit is set on the lower costal edge, so the cephalic segment of the prosthesis may be fixed by tissue adhesives, or sutures from the prosthesis to the peritoneum and the diaphragm. Our group employs a combination of tissue adhesives such as Tissucol® and, sometimes, depending on the size and type of implant used, employs the use of two or three stitches of absorbable material between the prosthesis and the peritoneum, which maintain, along with the abdominal pressure and the liver, the mesh in place.
Surgical Technique
The technique is similar to that described for subxiphoid hernias. Placement of trocars is almost identical (Fig. 12.4) (mirror image in the case of a left subcostal hernia). The technique is always IPOM, and prostheses are used according to the surgeon’s preferences: PTFE (Dual Mesh™ Plus, W.L Gore & Associates, Newark, DE, USA) or Parietex™ composite (Covidien, Dublin, Ireland). Frequent complications are seromas (which can usually be treated conservatively), hematoma, and persistent postoperative pain. Visceral lesions are rare, if the technique is successful, but if they go unnoticed, they can produce high mortality and usually involve reoperation and explant of the prosthesis. In the case performing a wide adhesiolysis, we systematically leave an aspirating drainage (Blake No. 19) through one of the 5 mm trocars, in the event of visceral perforations, which will facilitate the decision for early reoperation if needed. The drainage is removed after 24 h, if discharge is less than 60 cc.
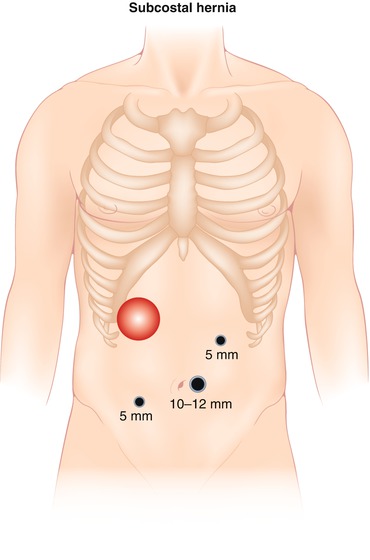
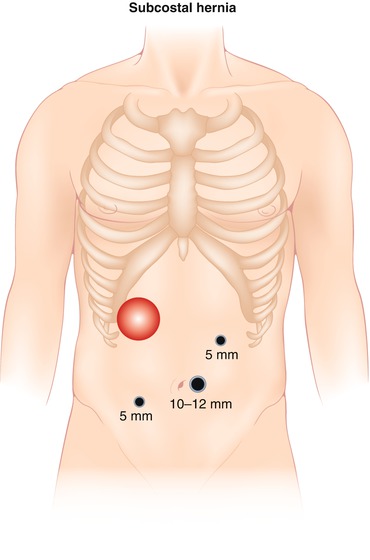
Fig. 12.4
Trocar placement in subcostal hernia
All patients leave the operating room with an elastic corset, continuously worn for 10 days. We have seen that postoperative pain and the incidence of symptomatic seromas have diminished significantly due to this. Average postoperative stay is 1–3 days. See Fig. 12.5.
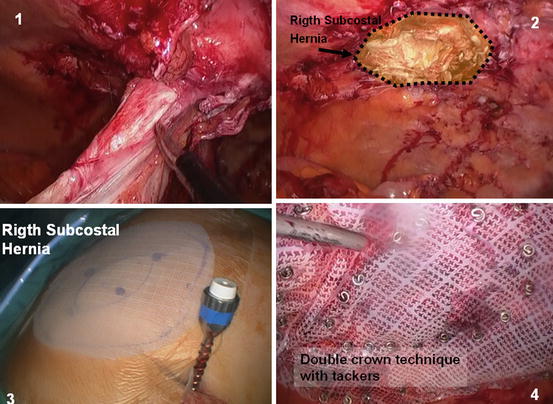
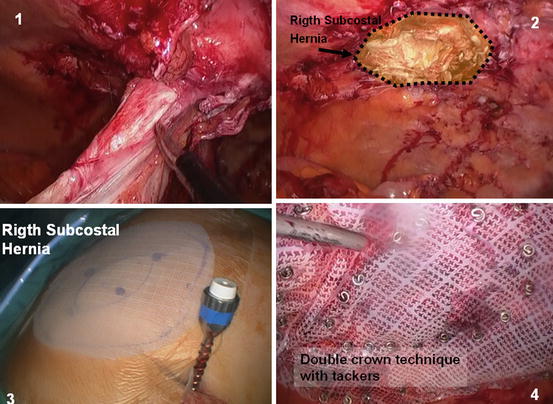
Fig. 12.5
Steps in subcostal hernia. 1 Adhesiolysis to discover the defect. 2 Subcostal hernia. 3 Measure of the limits of the hernia and the mesh (overlapping 5 cm). 4 Double crown technique with tackers
Suprapubic Hernias
Suprapubic incisional hernias are defined as parietal defects located less than 4 cm from the symphysis pubis. The concept was first introduced by El Mairy [10]. This type of hernia usually appears after lower midline laparotomies during gynecological and urological or rectal surgical interventions, and less frequently after Pfannenstiel’s or Maylard incisions.
As a result of their low and mostly unknown incidence, very little has been published about them. The key to a proper repair is perfect knowledge of the local anatomy and all the osteomuscular and neurovascular structures. Before the development of laparoscopic techniques, the standard for this type of hernia repair was popularized by Stoppa: implantation through an open approach, prosthesis in the Retzius space, anchored to Cooper’s ligament on one or both sides. Hirasa et al. in 2001 [11] published his results of laparoscopic treatment of these defects in 7 patients using a composite prosthesis anchored with metallic helical sutures. He described an initial 14.3 % recurrence rate. Other important series published to date are those of Carbonell et al. in 2005 (n = 36) [7], with laparoscopic approach and fixation with transparietal sutures and helical sutures to the Cooper’s ligament (recurrence rate of 5.5 %), and the recent series by Sharma et al. in 2011 (n = 72), the largest published to date with a recurrence rate of 0 % [12]. Essential surgical principles for the laparoscopic repair of suprapubic hernias are the same as for the rest of incisional hernia repair: proper fixation to the abdominal wall and 5 cm or more overlap. The problem in this case is that the inferior limit of the defect tends to be very close to the pubis and therefore does not allow for a proper fixation or overlap below the pubis. In order to achieve this, it is essential to carry out an opening of the supravesical peritoneum as in the TAPP technique for the laparoscopic treatment of inguinal hernia. The peritoneal flap must be pulled back to expose all the anatomical structures of the region: the symphysis pubis, Cooper’s ligaments, and epigastric vessels on both sides, retracting the bladder down and dissecting the Retzius space widely. Only by this often difficult and potentially dangerous dissection is it possible to achieve a proper overlap of the prosthesis in the caudal edge of the hernia defect. Once the prosthesis is placed in this position and at least a 5 cm overlap is guaranteed, the mesh should be fixed as described by Carbonell [7], using transfascial or helical sutures to the abdominal wall and using helical sutures to the pubis bone between both Cooper’s ligaments.
Surgical Technique
The position of the patient on the operating table is similar to other hernias, and the location of the trocar is shown in Fig. 12.6, but in the case of suprapubic hernias, a bladder catheter will be inserted for bladder filling/identification during the dissection of prevesical space. Our group has changed the position, exchanging the trocar for the optic, placing it almost at the midline, and raising the left-working trocar to an almost subcostal situation.
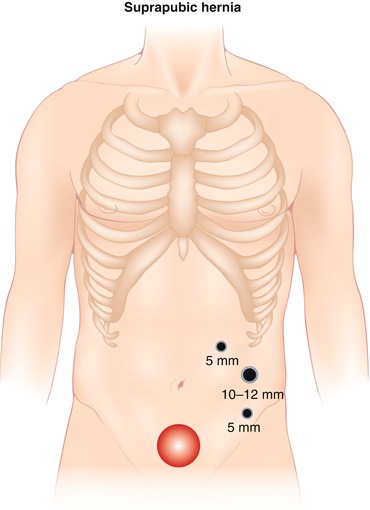
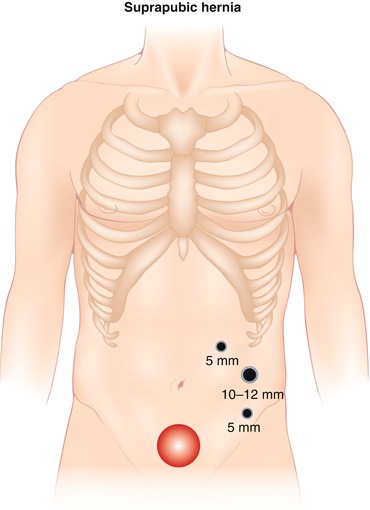
Fig. 12.6




Typical disposition of trocars in suprapubic hernia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








