Minimally invasive surgery has revolutionized surgery for urologic disorders in pediatric patients. Laparoscopic procedures have become widely available for several different ablative and reconstructive operations in children. The success rates have paralleled those of open surgical techniques and provide the benefit of smaller incisions and less manipulation of tissue during the procedures. Robotics has enhanced these factors, coupled with increased dexterity, better visualization, and less fatigue, allowing greater precision. We must continue to evolve with the ever-changing advancements in technology and take a keen interest so that we can influence development.
Laparoscopy has its origins in the use of the cystoscope to inspect the peritoneal cavity. Within urology and pediatric surgery, the first widely accepted use of laparoscopy was for inspection of the gonads in a child with ambiguous genitalia, rather than using open abdominal exploration.
From these roots, laparoscopy has taken on a greater role in the surgical solutions for urologic disease in pediatric patients. Minimally invasive laparoscopic procedures have become widely available for several ablative and reconstructive operations in children. The small incisions used for open surgery on large organs such as the kidney in pediatric urology typically require a large amount of dissection. The organ system is then brought up to the skin or even out of the wound to perform the operation when an open approach is used. With minimally invasive surgery (MIS) the exposure to internal organs and allowing surrounding tissue to remain in situ can only be paralleled by large open incisions. There is minimal tissue manipulation with MIS when done properly.
In the past decade, technical advances such as smaller endoscopic instruments and high-resolution cameras have contributed to the widespread use of MIS in children. The introduction of robotic surgical systems represents a further step in the evolution of endoscopic instrumentation. These computer-enhanced systems offer three-dimensional visualization and significantly improved instrumentation with motion scaling and a wrist mechanism that allows surgeons to perform complex reconstructive procedures. Although these specific advantages might benefit pediatric patients, the number of reports of robotic repairs performed in children is increasing. Initially, the robot was thought to be bulky for children, but the delicate robotic movements are ideal for the reconstructive surgeries children require; hence, pediatric urology has embraced robotic technology.
The learning curve
The learning curve for MIS in children must be addressed. The skill set requires thinking regarding placement of incisions, different presentation of anatomy, and the operating room staff must learn to use new and ever-changing equipment. The technical surgical skills require mastery. The time constraints for experienced surgeons to move from the comfort of the proficient master to join the ranks of the novice surgeon make the task daunting. For those in academic training centers, training residents and fellows can present an unfamiliar challenge, particularly if their exposure is otherwise limited. Deliberate practice is a term introduced by K. Anders Ericcson to describe the methods by which expert performers in many fields (eg, sports, music, sculpture) achieve the highest levels of ability. Deliberate practice, although time consuming, is essential for obtaining proficiency in MIS and needs to be done in a mentored environment. It is erroneous to assume that experience is synonymous with expertise. Practicing the same mistakes creates an experienced, but poorly skilled surgeon. The learning curve entails a kinesiology of MIS where surgeons need to learn how their body works for and against the task at hand; for example, tendencies that are disadvantageous in surgery such as upward retraction, tunnel vision, and nondominant hand neglect. Overcoming these errors requires training them away.
Equipment
As a new field with constantly emerging new technology, an institutional commitment to the purchase and upgrading of instrumentation is required, and the surgeons must understand the equipment. MIS requires mastery of the technology of surgery to proficiently and safely use the instrument; the surgeon needs to know exactly how the tools work, the way the engineers designed them to work, and why they work. For example, surgeons should understand how electrosurgery generators actually work; what waveforms are generated; and how voltage changes with impedance, the tissue, and the patient size.
Equipment
As a new field with constantly emerging new technology, an institutional commitment to the purchase and upgrading of instrumentation is required, and the surgeons must understand the equipment. MIS requires mastery of the technology of surgery to proficiently and safely use the instrument; the surgeon needs to know exactly how the tools work, the way the engineers designed them to work, and why they work. For example, surgeons should understand how electrosurgery generators actually work; what waveforms are generated; and how voltage changes with impedance, the tissue, and the patient size.
Patient physics and physiology
Children present a small working environment compared with adults. For instance, an adult pneumoperitoneum will typically provide a 5- to 6-L working space, whereas a 1-year old will present a 1-L intra-abdominal space. Also, the body surface area is smaller and the chance of port site conflicts, such as instrument crossing or trocar headpiece collisions, is greater for children.
Children are considered more sensitive to pressure in the working space than adults, and have a greater chance of developing crepitation and dissection of insufflation gas. In the author’s experience, working pressures in infants (aged 0–2 years) are 8 to 10 mm Hg; with older children and adolescents pressures of 10 to 12 mm Hg are typically sufficient. The abdominal wall of children has less resistance (or tone), so there is little change in the working space afforded by increasing the pressure beyond these levels. A benefit can be realized in increasing the pressure to 15 to 20 mm Hg for trocar insertion. Although the added pressure does not increase the working space, it does increase the resistance of the wall to deformation, easing safe trocar insertion.
Because of the more abdominal position of the bladder in infants, a Foley or straight catheter should be placed before access in all infants to reduce the possibility of bladder injury. Placement is also recommended for all children during pelvic procedures to aid visualization of pelvic structures. Because of the greater incidence of aerophagia and inflation of the stomach with air during induction of anesthesia in children, tube decompression of the stomach is an advantage.
Access in children
Open Access
The Hasson technique where an incision is made in an open fashion and carried down to expose the peritoneum, which is then opened, allows the initial port to be placed in the peritoneal cavity under direct vision. This technique has been recommended safer for children because of the decreased anterior-posterior diameter of the abdomen, and hence, closer proximity to the great vessels. Large multicenter analyses of complications associated with laparoscopy have shown a substantial reduction in the incidence of major vascular injuries with open access. The risk of major vascular injury during access is low but not zero with open techniques. The risk of bowel injury was higher with open methods in these studies. The frequency of injuries with access has decreased with time (earlier studies report higher complication rates) and decreases with operator experience.
Needle Access
The Veress technique uses a needle with a spring-loaded safety insert that is placed blindly into the abdomen. The abdomen is inflated and then the ports are placed. The risk of injury is perceived to be higher. There are numerous case reports published describing a trocar or Veress needle injury, proposing open access as the means to avoid that injury. However, large multicenter analyses document similar rates of injury with all methods.
Direct Access
Direct access implies the use of optical or special bladeless trocars. The trocar is placed directly through the abdominal wall without insufflation. For optical trocars, progress through the abdominal wall is observed directly as the port transits the wall. Anecdotally, this seems to be the least used in pediatric access techniques.
Procedures
Diagnostic Laparoscopy
Initial applications of laparoscopy were used for diagnostic purposes. For example, laparoscopy can be used for evaluation of the impalpable testis; it is currently used for laparoscopic orchiopexy rather than for diagnosis alone. The benefit of diagnostic laparoscopy is that it can be done with needle scopes typically 2 mm in diameter that fit through a Veress needle containing a sheath for the endoscope. Diagnostic laparoscopy also plays a role in the child with intersex conditions when conventional imaging is insufficient or not possible.
For hernia surgery, laparoscopic assessment of the contralateral inguinal ring at the time of inguinal hernia repair has been well described with large series demonstrating its utility, although controversy exists in its clinical relevance when a contralateral patent processus vaginalis is noted. Access is gained via the ipsilateral open hernia sac. Either a 3- to 5-mm trocar or a 16-gauge angiocatheter is placed into the abdominal cavity via the sac. Insufflation at 8 mm Hg is used and then a 70° endoscope is placed through the access. The size of the scope varies with the type of access used. The ring is easily visualized and then one can determine if the contralateral side warrants repair.
Orchiopexy
Laparoscopic orchiopexy is the most widely performed laparoscopic technique in pediatric urology, and is used for correction of intra-abdominal testis ( Fig. 1 ). This technique is performed either by a single stage or primary orchiopexy that leaves the spermatic vessels intact, or by a staged Fowler-Stephens orchiopexy where the vessels are ligated and transected. In the latter method, the spermatic vessels are occluded, usually with a clip, suture, or by fulguration. The testis is left in place, and at a second sitting, 4 to 6 months later, the testis is mobilized to the scrotum on a pedicle of the vas deferens and peritoneum with the spermatic vessels transected. Robotic surgery can be used in difficult cases such as high intra-abdominal testicles, and in particular for second-stage surgeries. The patient is placed supine in the Trendelenburg position with the ipsilateral side elevated 30° to 40°. The bladder is emptied to aid in access and visualization. Port placement entails the camera port in the umbilicus and 2 working ports or stab incisions made with a number 11-blade scalpel: one on the same side of the testicle above the umbilicus in the midclavicular line, and the other contralaterally below the umbilicus, also in the midclavicular line. Although available, I have not found the robot to be useful in orchiopexies because reconstruction is not a part of the procedure.
Nephrectomy
As with robotic orchiopexy, simple nephrectomy is somewhat of an overkill of robotic technology; however, robotic advantages such as the three-dimensional images, increased dexterity, and decreased learning curve can be advantageous for beginners. Nephrectomy can be performed using transperitoneal or retroperitoneal approaches, but in robotics the transperitoneal operation is the most readily accomplished because of the size of the ports and the arms, especially in the infant population. The choice of the transperitoneal or retroperitoneal approach depends on the surgeon’s experience. The choice may be influenced by the need for additional procedures such as complete nephroureterectomy and bladder access if ureteral reimplantation is required. Retroperitoneal access is distinct in port placement and patient positioning. Ports are placed posteriorly or laterally depending on the surgeon’s preference. The size of the robotic arms makes a posterior approach more difficult except in older children (ie, >12 years). Appropriate placement of the trocars is of utmost importance, and 3 to 4 laparoscopic ports are inserted at the surgeon’s discretion.
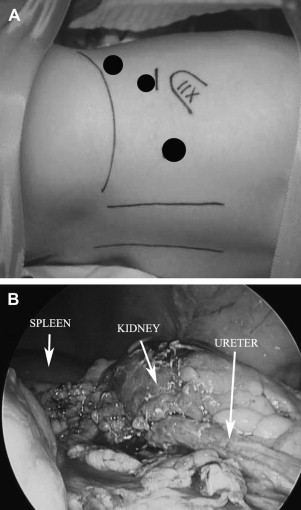
Retroperitoneal access is achieved through the first trocar incision, 15-mm long and 10-mm from the lower border of the tip of the 12th rib ( Fig. 2 A). A working space is created by gas insufflation dissection, and the first trocar is fixed with a purse-string suture applied around the deep fascia to ensure an airtight seal. Another approach to create the retroperitoneal space uses 2 index fingers of a powder-free surgical glove placed one inside the other and ligated onto the 5- or 10-mm trocar sheath. The dissection is then performed by instilling 500 mL of warm saline through the insufflation channel of the trocar. After completed dissection, the trocar is reinserted without the balloon and pneumoretroperitoneum is established (maximum pressure 12 mm Hg or age dependent). A 5- or 10-mm 0° telescope is inserted through the first trocar. A second 3-mm trocar is inserted posteriorly near the costovertebral angle; the third 3-mm trocar is inserted 10 mm above the top of the iliac crest at the anterior axillary line. To avoid transperitoneal insertion of this trocar, the working space is fully developed and the deep surface of the anterior wall muscles are identified before the trocar is inserted. The insufflation pressure is less than 12 mm Hg and the flow rate of CO 2 is progressively increased from 1 to 5 L/min The kidney is approached posteriorly, Gerota fascia is incised parallel to the psoas muscle, the perirenal fat is dissected to reveal the lower pole of the kidney in which the renal pelvis is first identified, and then mobilized (see Fig. 2 B). The ureter should be identified first and transected because it can be used as a handle and guide to reach the hilum.