and Armanda Tatsas2
(1)
Department of Pathology, The Johns Hopkins University School of Medicine, Baltimore, MD, USA
(2)
Pathology Group of Louisiana, Baton Rouge, LA, USA
Introduction
Computed tomography (CT)- or ultrasound (US)-guided fine needle aspirations (FNAs) and core biopsies (CB) are increasingly used for the diagnosis of mass lesions of kidney detected by imaging techniques. Although clinical and radiological findings would be adequate to determine the benign or malignant nature of the lesion in most cases, in some, ruling out a metastatic neoplasm or a more specific diagnosis of the type of tumor may be needed to choose the appropriate therapy (e.g., total vs partial nephrectomy, cryoablation, neoadjuvant-targeted therapy).
FNAs have been used alone or in combination with core biopsies. Multiple regions of a large tumor can be sampled by FNA with lesser risk of complications, and it could also help to direct the core biopsy to the site which is best representative of the lesion if done in combination with core biopsies.
Normal Components
Varying numbers of renal tubules and glomeruli may be found in fine needle aspirations. Glomeruli appear as thick, rounded structures with dense centers (Fig. 5.1). Renal tubules are seen as small monolayer tissue fragments, groups, or tubular structures (Figs. 5.2 and 5.3). They may be mistaken for well-differentiated renal cell carcinoma in limited specimens.
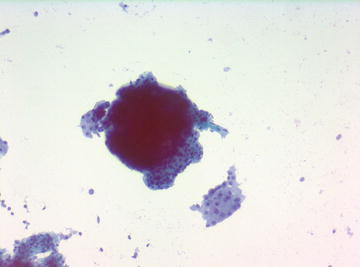
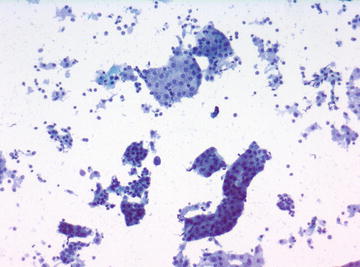
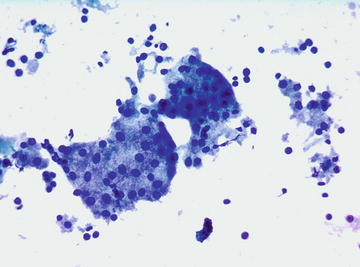
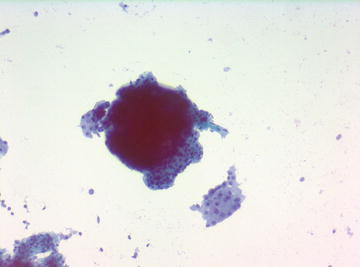
Fig. 5.1.
Glomerulus: Note fragment of proximal tubular epithelium. (Papanicolaou stain, medium power)
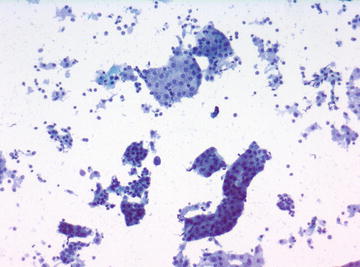
Fig. 5.2.
Renal tubular epithelium. (Papanicolaou stain, low power)
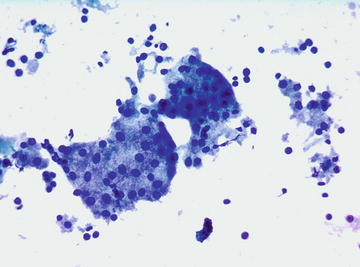
Fig. 5.3.
Fragment of proximal tubular epithelium: (Papanicolaou stain, medium power)
Nonneoplastic Masses and Cystic Lesions
Xanthogranulomatous Pyelonephritis (XGP)
Xanthogranulomatous pyelonephritis is a chronic inflammatory disease of kidney predominantly occurring in women. In 90 % of these cases, the kidney is diffusely involved. In a small percentage of cases, XGP is focal, forming a mass lesion mimicking renal cell carcinoma. Histologically it is composed of lipid-laden macrophages mixed with lymphocytes and plasma cells. Lipid-laden macrophages may mimic the clear cells of the conventional RCC.
Cytomorphology:
Misdiagnosis of XGP as renal cell carcinoma has been reported in FNAs and urine specimens. In FNA specimens, lipid-laden macrophages with vacuolated cytoplasm and vesicular nuclei with prominent nucleoli may mimic clear cell RCC. The cases showing an inflammatory background with predominantly lymphocytes, plasma cells, and occasional multinucleated cells mixed with histiocytes can be diagnosed as or suspected of being XPG in FNA specimens (Fig. 5.4a–c).
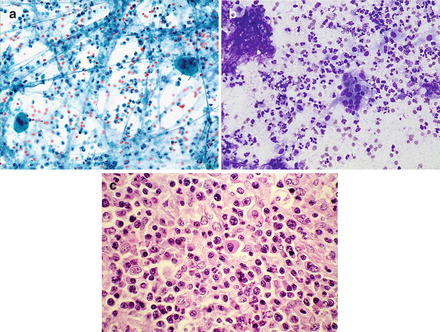
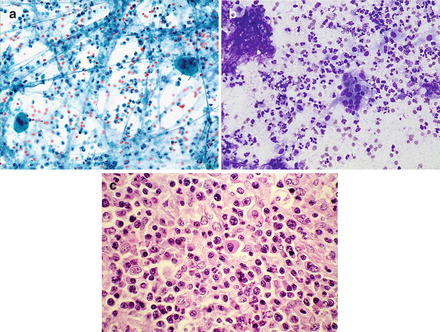
Fig. 5.4.
Xanthogranulomatous pyelonephritis: Multinucleated giant cells in a background of lymphocytes, neutrophils, and macrophages. (a) (Papanicolaou stain, low power). (b) (Diff-Quik stain, medium power). (c) Predominantly mononuclear cells, some with significant nuclear atypia (Cell block, H&E stain, medium power)
Key features:
Varying number of lipid-laden macrophages
Lymphocytic/plasmocytic background
Differential diagnosis:
Conventional (clear cell) RCC is the main tumor to be considered in the differential diagnosis. In cases with predominantly lipid-laden macrophages, CD68 stain on cell blocks or core biopsies confirm the diagnosis of XPG.
Abscess
Retroperitoneal abscesses in the kidney region are usually secondary to bacterial infection at another location. They can be confined to the kidney, occur in the perirenal region, or mixed. Abscesses confined to the renal parenchyma are rare and can be treated medically. Others usually require drainage or more invasive surgical procedures.
In aspiration specimens, neutrophils are the predominant cell component. In addition, rare degenerated renal tubular cells and macrophages may be present.
Benign Cysts
Benign renal cysts are common findings in older individuals. They are usually unilocular and are diagnosed radiologically. There are, however, some benign cysts which have atypical imaging and cytological features which make the differential diagnosis from malignant neoplasms difficult.
Aspiration specimens of benign cysts usually contain predominantly macrophages. Fragments of cyst lining epithelium and renal tubular epithelium could be present. Rarely, round lamellated structures (Liesegang rings) are present (Fig. 5.5a, b). In rare cases, histiocytes or epithelial lining cells present atypical features which are similar to those of renal cell carcinoma (Fig. 5.6a–c).
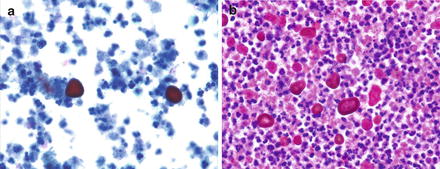
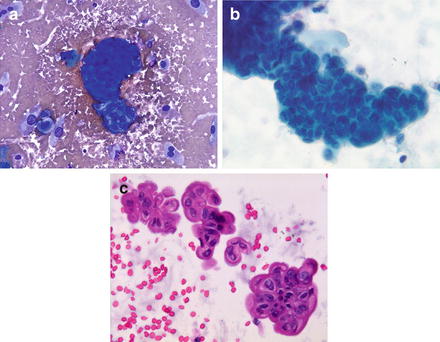
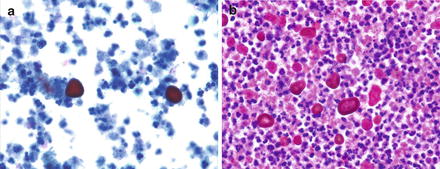
Fig. 5.5.
Renal cyst: Liesegang rings in a background of macrophages. (a) (Papanicolaou stain, medium power). (b) (Cell block, H&E stain, medium power)
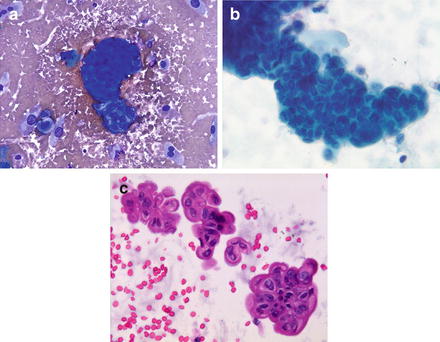
Fig. 5.6.
Benign cyst: Atypical epithelial fragments. In this case, a neoplasm was suspected, but the resected cyst was completely benign. (a) Epithelial tissue fragment (Diff-Quik stain, low power). (b) A large atypical epithelial fragment composed of disorganized epithelial cells with enlarged nuclei slightly varying in size and shape (Papanicolaou stain, medium power). (c) Atypical tissue fragments (H&E stain, medium power)
Key features:
Predominantly macrophages
Epithelial cells from cyst lining
Rarely, round lamellated structures (Liesegang rings)
Differential diagnosis:
In most cases the diagnosis can be made with the characteristic features seen in FNA samples. In rare cases, atypical cells may mimic renal cell carcinoma or cystic renal cell neoplasms with extensive necrosis may be misdiagnosed as benign cyst in aspiration material.
Extramedullary Hematopoiesis (EMH)
EMH occurs in conditions of decreased hematopoiesis by bone marrow or increased destruction of peripheral red blood cells and commonly presents as diffuse involvement of liver and spleen. The occurrence of EMH as a solitary mass in the kidney is rare. Malignancy is usually suspected on imaging studies, and diagnosis is made by FNA or core biopsy.
In FNA specimens, the presence of erythroid and myelocytic precursor cells and megakaryocytes in correlation with clinical features, blood and bone marrow findings, establishes the diagnosis.
Benign Neoplasms
Oncocytoma
Oncocytomas comprise 3–5 % of primary renal tumors in adults. The majority occur over the age of 50 and predominantly in men. Approximately two-thirds are found incidentally by imaging studies performed for unrelated reasons. They are generally solitary lesions, but multiple, unilateral, or bilateral tumors occur in 5–6 % of cases.
Histologically, oncocytomas are usually composed of nests of oncocytic cells with eosinophilic, granular cytoplasm and typically round, uniform nuclei with evenly dispersed, finely granular chromatin (Fig. 5.7a). Occasional large, pleomorphic nuclei can be found in some cases.
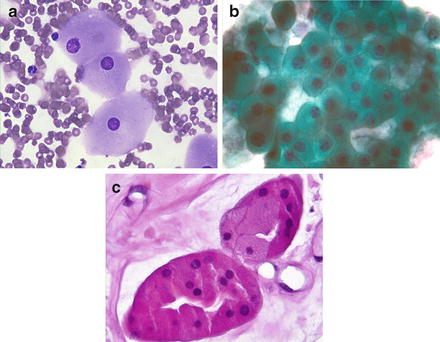
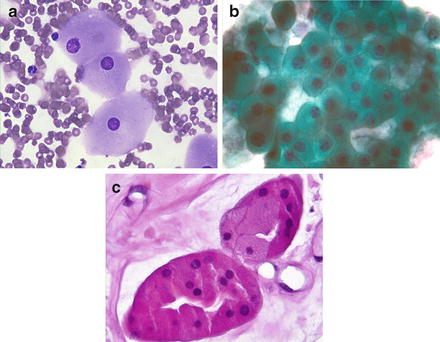
Fig. 5.7.
Oncocytoma: (a) Large cells with round, central, or eccentric nuclei with prominent nucleoli. (Diff-Quik stain, high power). (b) Large oncocytic cells with round, uniform nuclei, prominent nucleoli, and granular cytoplasm. (Papanicolaou stain, high power). (c) Oncocytic cells forming two glandular structures. (Cell block, H&E stain)
Cytomorphology:
FNA samples usually reveal varying sizes of tissue fragments and cell aggregates as well as some single cells with oncocytic features (Fig. 5.7b). Typically tumor cells have uniform, round nuclei with or without prominent nucleoli (Fig. 5.7c). Occasional large, pleomorphic nuclei may be present in some cases. Cytoplasm is usually abundant, homogeneous, and finely granular.
Immunohistochemistry:
Oncocytomas are positive for AE1/AE3, CAM5.2, CD117, Ksp-cadherin, and negative for CAIX, CK7, Ep-CAM, and RCC.
Key features:
Uniform tumor cell population with homogeneous, acidophilic, granular cytoplasm
Uniform, round nuclei with smooth outlines with or without prominent nucleoli
Differential diagnosis:
Other types of RCC with areas of oncocytic differentiation should be ruled out. Multiple biopsies (FNA and core) from different areas of the tumor minimize sampling error. In limited material, cytopathologic diagnosis should be made cautiously indicating that the findings are consistent with oncocytoma if the findings are representative of the entire tumor. Chromophobe (CR) RCC with predominantly eosinophilic cell component can be misdiagnosed as oncocytoma. CRRCC has nuclei with wrinkled borders, variation in size, and frequent binucleation.
Positive perinuclear staining with Hale’s colloidal iron stain is typical for CRRCC and helps in its differentiation from oncocytoma.
Angiomyolipoma
Angiomyolipoma is a benign mesenchymal neoplasm composed of varying proportions of epithelioid smooth muscle cells, fat, and blood vessels with thick walls. It comprises about 2 % of renal neoplasms. Although the majority of renal angiomyolipomas are sporadic, there is a strong association with tuberous sclerosis. Between 75 and 80 % of patients with tuberous sclerosis develop angiomyolipomas. Angiomyolipomas can be accurately diagnosed by imaging studies, with the exception of a small proportion with absence of or a small amount of fat tissue which do not have the characteristic imaging features. Many morphological variants have been described. One variant, epithelioid angiomyolipoma, is considered potentially malignant. Local invasion and rare cases of metastases have been reported.
Cytomorphology:
Varying proportions of adipose tissue, spindle and epithelioid cells with rare intranuclear inclusions can be identified (Fig. 5.8a, b). Thick-walled blood vessels can only be seen in cell blocks and core biopsies (Fig. 5.8c).
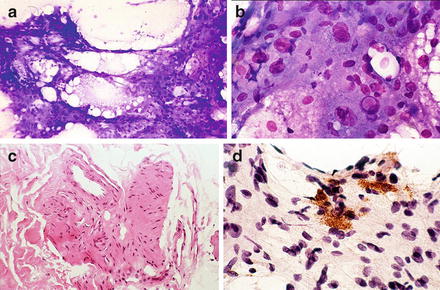
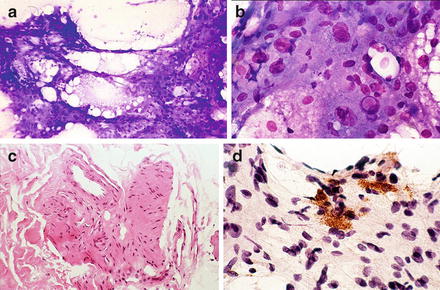
Fig. 5.8.
Angiomyolipoma: (a) Adipose tissue and epithelioid cells. (Diff-Quik stain, low power) (b) Atypical epithelial smooth muscle cells: large nuclei with prominent nucleoli, one intranuclear pseudoinclusion (Diff-Quik stain, medium power) (c) Thick walled blood vessels (Cell block, H&E stain, low power) (d) Positive staining with HMB45. (Medium power)
Immunohistochemistry:
Muscle markers (SMA, desmin), vimentin, c-kit, and HMB45 are usually positive (Fig. 5.8d).
Key features:
Mixture of adipose tissue, atypical epithelioid cells, and spindle cells
Thick-walled blood vessels (cell block or core biopsy)
Focal positive HMB45 staining
Differential diagnosis:
Cases of predominantly atypical epithelioid cells can be difficult to differentiate from high-grade, poorly differentiated primary or metastatic carcinomas. Immunostains could be helpful as could repeat FNA and/or core biopsies with extensive sampling of the tumor and correlation of clinical and radiological findings.
Metanephric Adenoma
A rare benign neoplasm of kidney, generally occurring in adults but also seen in children. Most of these tumors are discovered incidentally during investigations for other problems requiring abdominal imaging studies. Histologically the tumor is composed of small epithelial cells forming small acini and lobulated papillary formations.
Cytomorphology:
There are a few publications about FNA of this tumor reporting cellular specimens composed of oval to round cells are arranged in microfollicular and papillary pattern. The tumor cells have scant cytoplasm, uniform nuclei with evenly distributed fine chromatin and, occasionally, small nucleoli. No pleomorphism, necrosis, or mitosis is present.
Immunohistochemistry:
Tumor cells are reported to be positive for vimentin, WT1, and CD57.
Key features:
Cellular specimen
Small cells with scant cytoplasm forming small acini
Differential diagnosis:
Solid forms of papillary renal cell carcinoma, nephroblastoma, and metastatic carcinomas such as papillary carcinoma of thyroid are major tumors to be considered in the differential diagnosis. Immunostain TTF-1 is positive in thyroid carcinoma and negative in metanephric tumor.
Malignant Neoplasms
Kidney cancers usually occur in older people. They may be sporadic or hereditary. The latter comprise about 4 % of kidney tumors. The majority of these primary malignant neoplasms of kidney are carcinomas arising from renal parenchyma. Primary tumors arising from the renal pelvis are rare. They are mostly urothelial, but squamous cell and adenocarcinomas may also occur.
Renal Cell Carcinomas (RCCs)
Renal cell carcinomas make up a small percentage (~3 %) of adult malignancies. They have multiple chromosomal abnormalities which differ among the types of RCCs. Some of these are shown in Table 5.1 Three major types, conventional (clear cell), papillary, and chromophobe, comprise 85–90 % of RCCs. There is limited information about FNA findings in the remaining rare types, some of which will be covered in addition to the major types (Table 5.2).
Table 5.1.
Genetic abnormalities in primary renal carcinomas.
Type of neoplasm | Genetic abnormality |
|---|---|
Clear Cell (conventional) RCC | 3p deletions |
Mutations of VHL gene | |
Deletions of 6q, 8p, 9p, 14q | |
Papillary RCC | Trisomies of 3q, 7, 8, 12, 16, 17, 20 |
Loss of Y | |
Chromophobe RCC | Monosomy of 1, 2, 6, 10, 13, 17, 21 |
Hypodiploid DNA | |
Collecting duct carcinoma | Losses of 1, 6, 14, 15, 22 |
Deletions of 8p and 13q | |
Mucinous tubular and spindle cell carcinoma | Loss of chromosomes 1, 4, 6, 8, 9, 13, 15, 22 |
Table 5.2.
Types of primary renal carcinomas.
Clear cell (conventional) RCC |
Papillary RCC |
Chromophobe RCC |
Collecting duct carcinoma |
Medullary RCC |
Mucinous Tubular and Spindle Cell Carcinoma |
Renal Cell Carcinoma with Xp11.2 Translocation |
Unclassified RCC |
Grading of RCC
Fuhrman grading is used in surgically resected specimens for predicting prognosis. The grades are based on nuclear size, nuclear shape, and size of nucleoli. Grade I, round uniform nuclei, approximately 10 μm, inconspicuous or absent nucleoli; Grade II, larger nuclei, approximately 15 μm, with irregular outlines, prominent nucleoli using ×40 objective; Grade III, larger nuclei, approximately 20 μm, with markedly irregular borders and prominent nucleoli using ×10 objective; Grade IV, markedly atypical nuclei, larger than 20 μm, prominent nucleoli using ×10 objective, and often spindle cell component (Fig. 5.9a–c). Grade I and Grade IV tumors are rare in most series.
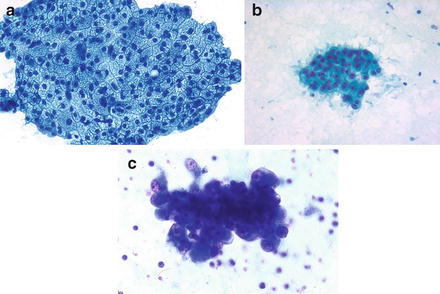
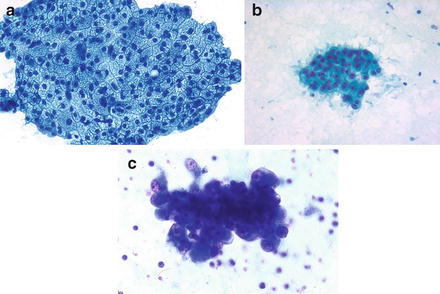
Fig. 5.9.
Clear cell (conventional) renal cell carcinoma (CCCRCC): Grading of RCC. (a) Low grade RCC (Fuhrman Gr. 1–2). Uniform, round nuclei with slight variation in size, inconspicuous nucleoli. (b) High grade RCC (Fuhrman Gr. 3). Large nuclei with macronucleoli. (c) High grade RCC (Fuhrman Gr. 4). Large pleomorphic nuclei with large nucleoli. (a–c, Papanicolaou stain, low power). (a, c) Reprinted with permission from: Fine Needle Aspiration Cytology, eds. MK Sidawy, SZ Ali, Churchill Livingston/Elsevier, 2007, Chapter 10, Kidney and Adrenal Glands, YS Erozan, pages 299–346
Agreement between the grading in needle biopsy specimens, both core biopsies and FNAs, and grading in surgical resected specimens has been found to be moderate, with biopsy specimens having a tendency to undergrading. The difference may be explained by the grading of surgical specimens being based on the area showing the highest grade of changes.
Accuracy of FNA in the Diagnosis of RCCs
FNAs are highly accurate for the diagnosis of RCCs. Subtypes of RCC are also diagnosed with very high accuracy in clear cell type. The accuracy of correct identification of papillary RCC and chromophobe RCC varies in published series.
Clear Cell (Conventional) Renal Cell Carcinoma (CRCC)
Clear cell (conventional) is the most common subtype, comprising 70 % of renal cell carcinomas. Sporadic CRCCs are usually solitary tumors. Multiple, bilateral tumors are rare in sporadic CRCC, but they are typical of hereditary forms such as Von Hippel–Lindau syndrome.
Histologically, the tumor is comprised of polygonal or cuboidal cells with clear or granular cytoplasm and distinct cytoplasmic borders surrounded by a thin-walled vascular network. Cytoplasm of clear cells contains lipid and glycogen. Various architectural patterns, including pseudopapillary forms, can be seen. Cystic changes, hemorrhage, and necrosis are common.
Cytomorphology:
Ultrasound- or CT-guided FNAs with on-site evaluation yield cellular material composed predominantly of tissue fragments and cell clusters (Fig. 5.10a, b). Tumor cells have clear or finely vacuolated cytoplasm with distinct cellular cytoplasmic borders (Fig. 5.11a, b). Most of the tumors have small round nuclei with inconspicuous or small nucleoli which correspond to Fuhrman Grade 2 (Fig. 5.11b). Higher grade tumors have larger nuclei with prominent nucleoli (Fig. 5.11c). One of the characteristic cytopathologic features of this tumor is crossing delicate vasculature in the tissue fragments (Fig. 5.12). Pseudopapillary fragments may be seen. They lack the fibrovascular stalk of the true papillary formations found in papillary renal cell carcinomas.
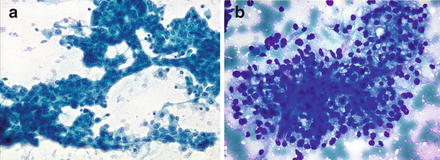
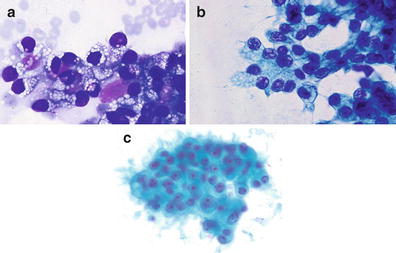
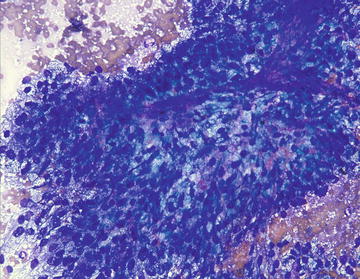
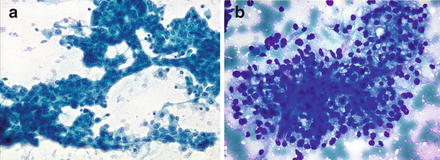
Fig. 5.10.
Clear cell (conventional) renal cell carcinoma: (a) A large tissue fragment with focal glandular formations. Tumor cells have enlarged nuclei, slightly varying in size with inconspicuous nucleoli and moderate to large amounts of dense cytoplasm. (Papanicolaou stain, low power) (b) Another large tissue fragment composed of tumor cells with large, vacuolated cytoplasm. (Diff-Quik, low power)
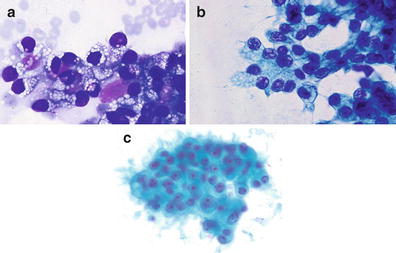
Fig. 5.11.
Clear cell (conventional) renal cell carcinoma: Vacuoles. (a) (Diff-Quik, high power). (b) Tumor cells have enlarged nuclei with irregular borders, coarse chromatin pattern, prominent nucleoli, and dense vacuolated cytoplasm. (Papanicolaou stain, high power). (c) Clear cell (conventional) renal cell carcinoma—High grade. Enlarged, round nuclei with bland chromatin and smooth nuclear borders. This tumor is high grade because of the macronucleoli. (Papanicolaou stain, high power). Reprinted with permission from: Fine Needle Aspiration Cytology, eds. MK Sidawy, SZ Ali, Churchill Livingston/Elsevier, 2007, Chapter 10, Kidney and Adrenal Glands, YS Erozan, pages 299–346
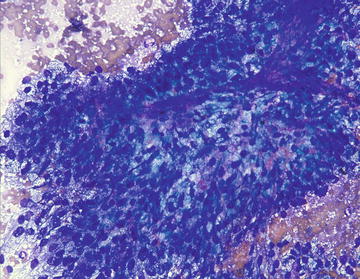
Fig. 5.12.
Clear cell (conventional) renal cell carcinoma: A large tissue fragment of tumor with crossing vessels. (Diff-Quik, low power)
Immunohistochemistry:
CRCC is usually positive for AE1/AE3 keratins, vimentin, RCC, CD10, CAIX, PAX-8, PAX-2 and negative for CD117, Ksp-cadherin, and parvalbumin.
Key features:
Cellular specimen with predominantly tissue fragments
Neoplastic cells with clear or finely vacuolated cytoplasm
Tissue fragments of tumor with transgressing thin-walled blood vessels
Differential diagnosis:
The most important differential diagnosis is the differentiation of CRCC from metastatic tumors with clear cell features. Adrenal cortical carcinoma and hepatocellular carcinoma are among these neoplasms. Papillary carcinomas with focal clear cell changes should also be considered. In the absence of clear cell changes, oncocytoma and chromophobe RCC may enter into the differential diagnoses.
Papillary Renal Cell Carcinoma (PRCC)
Papillary renal cell carcinoma comprises 10–15 % of renal parenchymal neoplasms. They are three times more common in men than in women. More than half of these neoplasms are discovered incidentally by abdominal ultrasound or computed tomography performed for other purposes. Multiple tumors are more common than conventional type. The survival rate, generally, is better than for conventional RCCs. The application of Fuhrman grading for prognoses is controversial. Genetically they show trisomy of chromosomes 7 and 17, with loss of the Y chromosome.
Characteristic histological features are papillary structures lined with neoplastic cells. Solid papillary and tubulopapillary forms are common. Aggregates of foamy histiocytes in the fibrovascular cores and hemosiderin pigment in the tumor cells and histiocytes are typically found. Two types have been classified: Type 1, the most common, composed of a single layer of neoplastic cells with scant, eosinophilic cytoplasm, small ovoid nuclei, and inconspicuous nucleoli. Abundant psammoma bodies may be seen. Type 2 tumors are composed of tumor cells with abundant eosinophilic cytoplasm with higher grade nuclei.
Cytomorphology:
Diagnostic FNA specimens are hypercellular, comprised predominantly of tissue fragments, cellular aggregates, and some single cells. There are usually some tissue fragments with characteristic papillary formation (Fig. 5.13), fibrovascular core surrounded by neoplastic cells which exhibit scant to moderate amounts of cytoplasm and round or ovoid nuclei with inconspicuous or small nucleoli (Fig. 5.14). Varying proportions of neoplastic cells may have clear cell features. Globular forms and loose cellular aggregates can be the predominant component (Fig. 5.15). The presence of abundant psammoma bodies is one of the characteristic features of these neoplasms (Fig. 5.14). Foamy histiocytes and hemosiderin pigment in tumor cells and histiocytes (Fig. 5.16a–c) are characteristic features of papillary RCC which help to differentiate this tumor from other types of RCCs. Clear cell features, focally or predominantly, could be present.
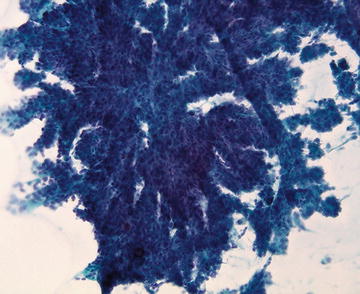
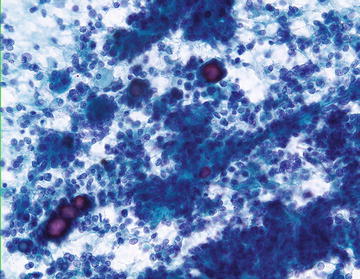
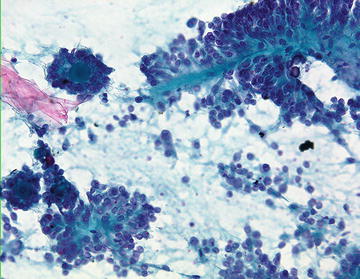
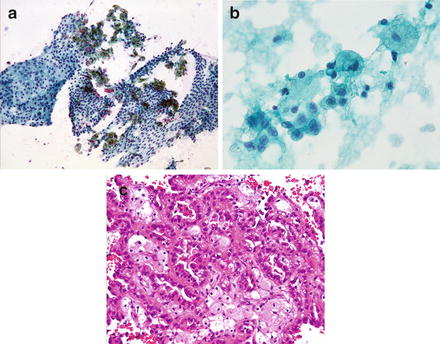
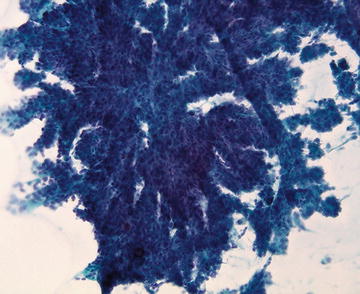
Fig. 5.13.
Papillary carcinoma: Large papillary fragment. (Papanicolaou stain, low power)
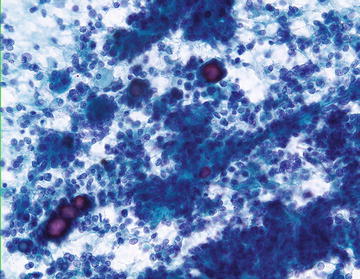
Fig. 5.14.
Papillary renal cell carcinoma: Papillary structures, single cells, and multiple psammoma bodies. (Papanicolaou stain, medium power)
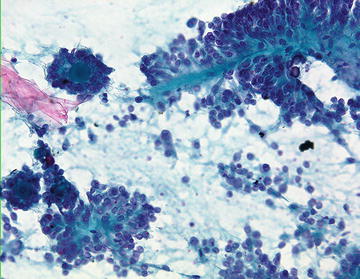
Fig. 5.15.
Papillary renal cell carcinoma: A papillary fragment with fibrovascular core and two globular structures forming psammoma bodies. (Papanicolaou stain, medium power)
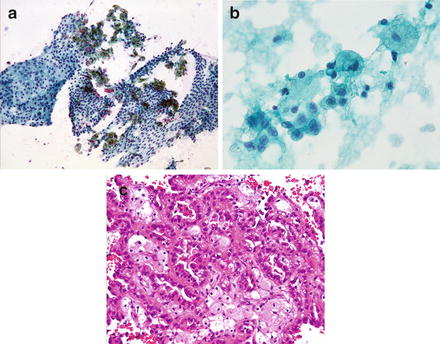
Fig. 5.16.
Papillary renal cell carcinoma: (a) Monolayer fragments of papillary carcinoma with hemosiderin pigment in the tumor cells and histiocytes. (Papanicolaou stain, low power) (b) A group of tumor cells and histiocytes. A few tumor cells have green intracytoplasmic hemosiderin pigment. (Papanicolaou stain, high power) (c) Tightly packed histiocytes surrounded by tumor cell. (Cell block, H&E stain, medium power)
Immunohistochemistry (IHC):
IHC is performed on the cell blocks or core biopsies. Papillary RCCs are strongly and diffusely positive for CK7 and AMACR (cytoplasmic, granular) and also positive for RCC, PAX-2, PAX-8, and CD10 (Fig. 5.17a–c).
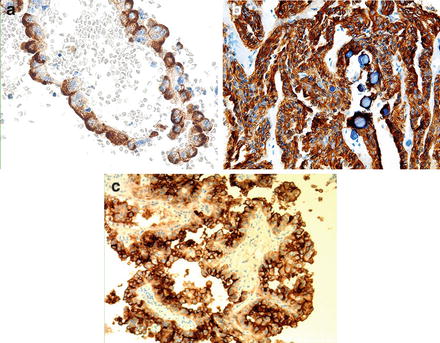
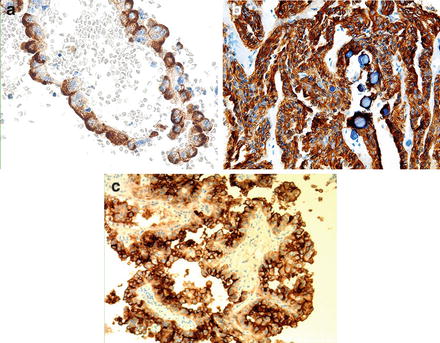
Fig. 5.17.
Papillary renal cell carcinoma: Cell block. Immunostains: (a) Strong reaction to RCC antibody. (H&E stain, low power) (b) Diffuse cytoplasmic staining with CK7 antibody. (low power) (c) Dense peripheral cytoplasmic staining with CD10 antibody. (low power). (a) Reprinted with permission from: Fine Needle Aspiration Cytology, eds. MK Sidawy, SZ Ali, Churchill Livingston/Elsevier, 2007, Chapter 10, Kidney and Adrenal Glands, YS Erozan, pages 299–346
Key features:
Hypercellular specimen with predominantly tissue fragments
Papillary forms with fibrovascular stalk
Neoplastic cells having round or ovoid nuclei with inconspicuous nucleoli and scant to moderate cytoplasm (Type 1)
Histiocytes, single or in aggregates
Hemosiderin pigment in histiocytes and neoplastic cells
Psammoma bodies, often abundant
Less frequently, large nuclei with prominent nucleoli and moderate to large amounts of cytoplasm (Type 2)
Differential diagnosis:
The characteristic cytomorphology includes papillary structures with foamy hemosiderin-laden histiocytes and hemosiderin pigment in the tumor cells. When the papillary tumor is composed of predominantly clear cells, the differential diagnosis includes mainly clear cell RCC and other rare subtypes, clear cell papillary RCC, and Xp11.2 translocation RCC. The presence of hemosiderin pigment in tumor cells, hemosiderin-laden histiocytes, and psammoma bodies are helpful features in differentiating PRCC from other renal neoplasms with clear cell features. Immunohistochemical and genetic profiles of these neoplasms are also different from PRCC.
Chromophobe Renal Cell Carcinoma
Chromophobe renal cell carcinoma (CRRCC) is a rare tumor comprising only about 5 % of renal cell carcinomas. Histologically, the tumor has two cell types: one has abundant clear to pale cytoplasm and the other granular, eosinophilic cytoplasm with thick cytoplasmic borders (eosinophilic type). Nuclei with wrinkled borders (raisinoid nuclei) and perinuclear clearing are characteristic features. Binucleation is common (Fig. 5.18).
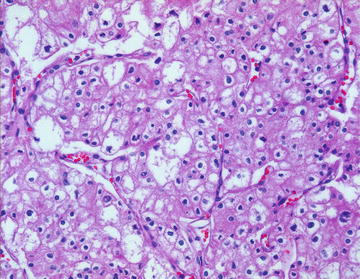
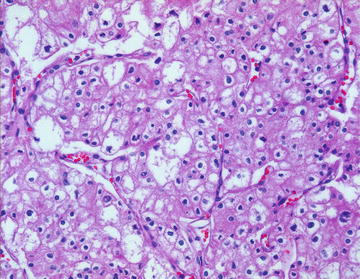
Fig. 5.18.
Chromophobe renal cell carcinoma: Tumor cells with eosinophilic, granular, pale or clear cytoplasm and hyperchromatic nuclei with irregular borders. Nuclei vary in size and most have clear areas surrounding the nucleus. Resected tumor. (H&E stain, medium power)
Cytomorphology:
FNA specimens are cellular with cohesive aggregates and single tumor cells (Fig. 5.19a). The latter have large pale or dense granular cytoplasm (Fig. 5.19b). Frequent binucleation and variation in nuclear size are characteristic features. Irregular nuclear borders and occasional intranuclear pseudoinclusions are also seen (Fig. 5.19c). The perinuclear clearing seen in histologic preparations is less apparent in cytologic preparations (Fig. 5.18).
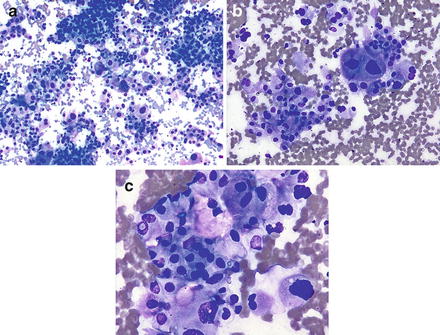
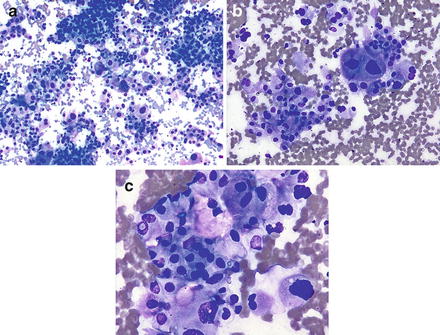
Fig. 5.19.




Chromophobe renal cell carcinoma: (a) Tissue fragments and single tumor cells. Marked variation in nuclear and cell size. Irregular nuclear borders and perinuclear clearing seen in some of the cells. (Diff-Quik stain, low power) (b) Binucleation, anisonucleosis, irregular nuclear borders, and a thin rim of perinuclear clearing in some cells. (Diff-Quik stain, high power) (c) Intranuclear pseudoinclusion. Marked anisonucleosis. (Diff-Quik stain, high power). (c) Reprinted with permission from: Fine Needle Aspiration Cytology, eds. MK Sidawy, SZ Ali, Churchill Livingston/Elsevier, 2007, Chapter 10, Kidney and Adrenal Glands, YS Erozan, pages 299–346
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







