Fig. 6.1
(a, b) Laparoscopic views of peritoneal carcinomatosis with the characteristic numerous white nodules on both parietal and visceral peritoneum (This was seen 2 months after a history of bladder perforation during resection of a tumour which turned out to be a high-grade MIBT)
A bimanual examination performed under general anaesthesia when the patient’s abdominal, perineal, and pelvic musculature is fully relaxed, before and after the TURBT, may be helpful for an initial assessment of the clinical stage. Large muscle-invasive tumours which are palpable before the resection are usually not felt after the procedure.
Random biopsies performed on normal-looking bladder mucosa to detect CIS are not recommended since the chances of a positive result are very low (<2 %) [3]. However, biopsies are indicated when urine cytology is positive or in the presence of mucosal lesions suggestive of CIS.
The use of hexaminolevulinate (Hexvix®) fluorescence has been shown to improve detection of Ta, T1, and CIS lesion, thereby improving the quality of the resection with a positive impact on the recurrence-free survival rate [5, 6].
The confirmatory diagnosis is obtained by a histopathological study of the TURBT specimens or the tumour biopsy. This is performed using H&E staining and reported according to different classifications:
WHO 1973: Grade 1 well differentiated, grade 2 moderately differentiated, and grade 3 poorly differentiated. This is gradually being replaced by the most recent classification below.
WHO 2004: Low-grade and high-grade tumours.
The next priority for the pathologist is to assess muscle invasion and categorize the disease as muscle-invasive (MIBT) (Fig. 6.2) or non-muscle-invasive bladder tumour (NMIBT).
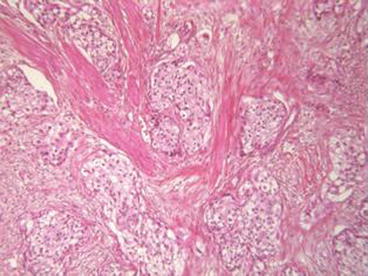
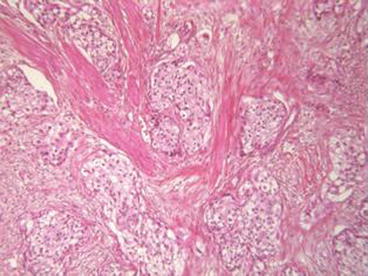
Fig. 6.2
TURBT specimen showing islands of tumour invading the muscle layer, i.e. a pT2 stage (Courtesy of A. Durlach, Pol Bouin Laboratory, University Hospital of Reims, France)
6.1.1 Novel Biological Parameters
Substaging T1 (T1a, T1b, and T1c) by evaluating the extension and depth of the lamina propria invasion has a good prognostic value: T1a = superficial invasion of lamina propria, T1b = invasion into the muscularis mucosa (MM), and T1c = invasion beyond the MM but not to the muscularis propria [7, 8]. Although not yet included in the current TNM classification, this substaging is recommended by the American expert panel in order to differentiate a simple microinvasion just beyond the basement membrane from a deeper invasion where the possibility of understaging is greater [9].
Lymphovascular invasion in T1 correlates with disease progression and metastases [10] (Fig. 6.3). Its presence in either T1 or T2 TURBT or radical cystectomy specimens is a strong predictor of frequent recurrences and a shorter survival rate [11]. However, its mention in the histopathological report (HPR) for T2 disease is only considered optional by the European expert panel [12].
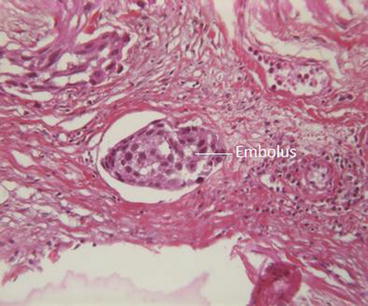
Fig. 6.3
Microphotograph of a TURBT specimen showing lymphovascular invasion (Courtesy of A. Durlach, Pol Bouin Laboratory, University Hospital of Reims, France)
Urothelial carcinoma subtypes: Several studies have identified three major molecular subtypes of urothelial carcinoma which carry important prognostic difference and various responses to conventional chemotherapy. Depending on the authors, these subtypes were named basal, luminal, and p53-like tumours [13] or urobasal, genomically unstable, and squamous cell carcinoma-like [14].
Study of the fibroblast growth factor receptor 3 (FGFR3) mutation or overexpression status: FGFR3 mutation has been found in the majority of low-grade NMIBT and in a minority of MIBT. However, in the latter there were an additional number of tumours harbouring FGFR3 overexpression, and about half of the cases of MIBT showed either FGFR3 mutation or overexpression [15]. Therefore, FGFR3 was suggested to be a promising target for therapy in bladder cancer [16].
The tumour staging is categorized according to the 2010 AJCC classification [17] (Table 6.1).
Primary tumour (T) | |
Tx | Primary tumour cannot be assessed |
T0 | No evidence of primary tumour |
Ta | Non-invasive papillary carcinoma |
Tis | Carcinoma in situ: “flat tumour” |
T1 | Tumour invades subepithelial connective tissue |
T2 | Tumour invades muscularis propria |
pT2a | Tumour invades superficial muscularis propria (inner half) |
pT2b | Tumour invades deep muscularis propria (outer half) |
T3 | Tumour invades perivesical tissue |
pT3a | Microscopically |
pT3b | Macroscopically (extravesical mass) |
T4 | Tumour invades any of the following: prostatic stroma, seminal vesicles, uterus, vagina, pelvic wall, abdominal wall |
T4a | Tumour invades prostatic stroma, uterus, vagina |
T4b | Tumour invades pelvic wall, abdominal wall |
Regional lymph nodes (N) | |
Nx | Regional lymph nodesa cannot be assessed |
N0 | No regional lymph node spread |
N1 | Single lymph node metastasis in the true pelvis (hypogastric, obturator, external iliac, or presacral lymph node) |
N2 | Multiple lymph node metastases in the true pelvis |
N3 | Metastasis to the common iliac lymph nodes |
Distant metastasis (M) | |
M0 | No distant metastasis |
M1 | Distant metastasis |
Anatomic stages/prognostic groups | |
Stage 0a | Ta, N0, M0 |
Stage 0is | Tis, N0, M0 |
Stage I | T1, N0, M0 |
Stage II | T2a or T2b, N0, M0) |
Stage III | T3a or T3b or T4a, N0, M0 |
Stage IV | T4b, N0, M0 or any T, N1–3, M0 or any T, any N, M1 |
At the time of diagnosis, it has been estimated that 75–85 % of all urothelial bladder tumours are non–muscle invasive and that 60–70 % will recur within the first year after TURBT, but only 10–20 % will progress to become muscle invasive or ̸ and metastasize [3]. It is this progression risk which is assessed by classifying the NMIBT as low-, intermediate-, or high-risk tumours (see below).
6.1.2 Progression Risk Factors
Traditionally, after staging and grading their infantries, strong armies were defined as those who could recruit larger numbers of soldiers to increase the size of their troops or who needed less time to prepare for new battles and those who were capable of deep penetration beyond the enemy lines.
These military principles also apply to the progression risk factors and aggressiveness of the BC.
Tumour stage: T1 is more prone to progress than Ta.
Tumour grade: High grade is more prone than low grade. CIS must always be considered as high-grade tumour, while Ta is more often regarded as low grade.
Tumour number.
Tumour size.
Time (in months) elapsed between the first tumour resection and the first recurrence.
The depth of lamina propria infiltration. This helps to differentiate between T1a and T1b.
Based on the abovementioned factors, three risk groups were defined in NMIBT (similar to the d’Amico groups described for PC) [18, 19]:
Low risk: solitary low–grade Ta, <3 cm, seen for the first time and not recurring on subsequent follow–up at 3 months. Carries a 7.1 % progression risk at 5 years and a 4.3 % mortality risk at 10 years.
Intermediate risk: multifocal and/or recurrent low-grade Ta (pT a G1–2) or first-time-seen single high-grade Ta (pTaG3) or low-grade T1 (pT1G2). Carries 17.4 % progression risk at 5 years and 12.8 % mortality at 10 years.< div class='tao-gold-member'>Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







