Fig. 26.1
CT scan showing a very rare case of adrenal myelolipoma on the right side. This is a low-density benign tumour consistent with fat content (Courtesy of S. Novellas, Radiology, Arnault-Tzanck Institute, Saint-Laurent- du- Var and CHU Nice, Nice, France)
Before IV contrast injection, a density ≤10 Hounsfield Units (HU), a homogenous appearance, and neat contours are features of a benign tumour, while malignant cortical adrenal tumours generally have a consistent density value ≥18 HU. Another characteristic feature seen in primary ACC, pheochromocytomas and metastatic tumours is the relatively slow contrast wash out [2]. A decrease of more than 40 % of the maximal enhancement 10 min after the injection has been reported to be pathognomonic of an adenoma [3].
The tumour size is another important feature to differentiate between a benign mass and an ACC. According to statistical data collected from a large series, the likelihood of malignancy doubles (to 10 %) at a threshold of ≥4 cm and rises to more than ninefold (47 %) for tumours ≥8 cm [4, 5] (Fig. 26.2a, b).
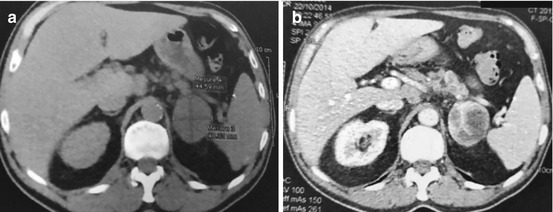
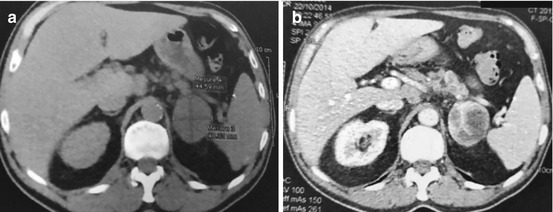
Fig. 26.2
(a, b) CT scan showing a 45 × 40 mm enhancing mass above the left kidney consistent with a left adrenal ACC in a 70-year-old man
Gadolinium-enhanced MRI may be an alternative in patients allergic to iodinated contrast.
Once suspicion of an ACC is raised by other investigations, 18F-FDG PET appears to be the standard imaging means to “ascertain” the diagnosis because of its reported 100 % sensitivity and negative predictive value (Fig. 26.3a–d) [6]. A threshold ratio of 1.8 between the maximum standardized uptake values (SUVmax) of the tumour and that of the liver demonstrated 100 % sensitivity and specificity after correlation with the final histological diagnosis [6]. A cutoff SUV of 3.1 was also proposed as a reliable demarcation point between malignant lesions and adrenal adenomas with sensitivity, specificity, positive predictive value and negative predictive value of 98.5 %, 92 %, 89.3 %, 98.9 %, respectively [7].
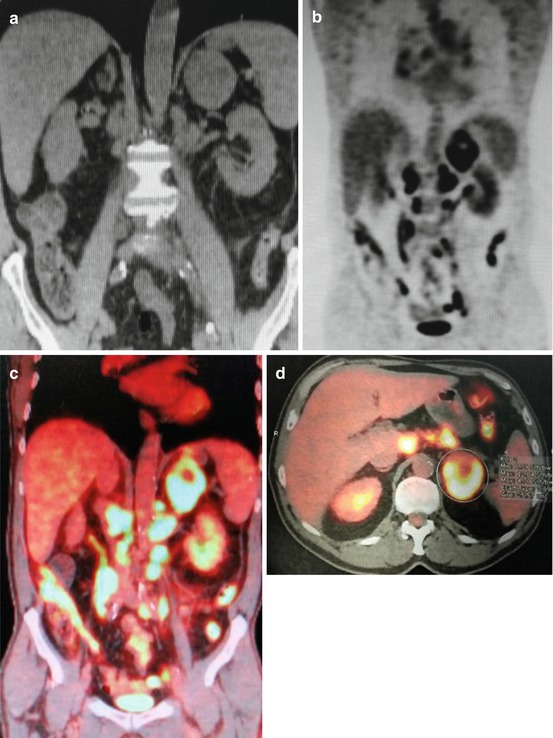
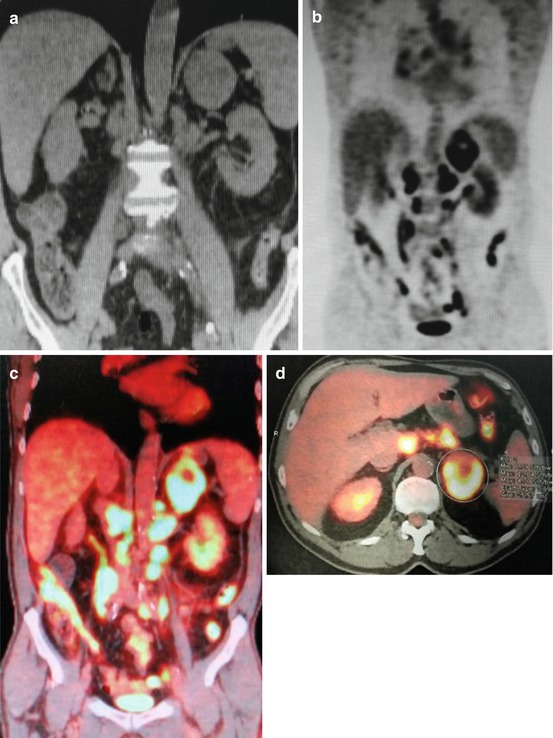
Fig. 26.3
(a–d) Same patient of Fig. 26.2. (a) Plain CT scan. (b) FDG-18F-PET. (c) Fusion PET-TDM showing a 45 × 48 mm hypermetabolic left adrenal tumour with SUV max 12, consistent with a ACC. There is a necrotic centre. There are also multiple hyperactive associated LNs SUV max from 9.1 to 13.1. (d) PET-TDM in horizontal section
Nine histological criteria of Weiss were used to predict tumour malignancy and prognosis: Fuhrman nuclear grade III or IV (see Chap. 13, Table 13.2), >5 mitosis/50 HPF, atypical mitosis, cytoplasm characteristics (less than 25 % of clear vacuolated cells being an unfavourable factor), diffuse architecture, tumour necrosis, venous invasion, sinusoid invasion and capsular invasion [8]. Each criterion is scored 1 when present. A total score >3 is predictive of malignancy. In view of the possible subjectivity inherent to the interpretation of some criteria of Weiss, a retrospective study proposed to double the weight of the 2 most reliable ones, i.e. the mitotic rate and the cytoplasm characteristics. In this modified Weiss criteria, presence of atypical mitosis, tumour necrosis and capsular invasion are still considered with a score 1 while the remaining has been abandoned [9].
However, histopathological diagnosis of ACC remains challenging as the distinction from a benign adenoma is generally difficult. A French study has identified 3 molecular predictors using tumour RNA micro-arrays as novel tools for the detection of malignancy and for predicting survival [10]: the combination of DLG7 and PINK1 for malignancy signature and the combined expression of BUB1B and PINK1 as predictors of survival.
More recently a novel steroid metabolomics1 approach was proposed to help in the differential diagnosis between an ACC and an adrenal adenoma [11]. This is a simplified diagnostic tool based on the identification of only 9 adrenal steroids from a 24-h urinary collection with properties that are most helpful in differentiating the malignant from the benign variety. This investigation is virtually equal in sensitivity and specificity to the currently used fastidious 32 steroid-based study.
Transcutaneous biopsy of the ACC is currently not recommended for the diagnosis of a primary ACC because of poor diagnostic value and possible complications (bleeding, tumour cell spillage), although a recent retrospective study has shown that it does not affect the recurrence-free or overall survival [12].
The use of a fine-needle biopsy should be restricted to [13]:
A suspected secondary tumour in patients with a history of other cancers (particularly lung, breast, kidney), with no signs of other metastases
A heterogeneous mass with high unenhanced attenuation value (>20 HU) after exclusion of pheochromocytoma
26.2 Disease Extension Investigations and Staging
These consist of the use of gadolinium-enhanced MRI and/or 18F-FDG PET scans.
Adrenal tumours metastasize most frequently to the lungs (72 %) and liver (55 %). Other sites include the peritoneum (33 %), bones (24 %), the contralateral adrenal gland (15 %) and brain (10 %) [14].
The first staging classification of ACC was proposed by MacFarlane over half century ago [15], which included four criteria: tumour size, lymph nodes, local invasion and metastases. This was later modified by Sullivan [16], and the first TNM classification was introduced in 2003 by the Union Internationale Contre le Cancer (UICC). More recently the European Network for the Study of Adrenal Tumours (ENSAT) developed a revised staging system [17] (Table 26.1). Its superiority in predicting cancer-specific mortality was corroborated by subsequent studies [18, 19].




Table 26.1
New Staging System for adrenocortical carcinoma (European Network for the Study of Adrenal tumour Classification 2008). ENSAT 2008
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







