Clinical history
The clinical history is the most important part of the diagnostic evaluation of the patient with
ED.
ED may represent an early marker of cardiovascular disease and even depression, which can then be addressed appropriately (
Montorsi et al., 2003a). The initial focus should address whether the patient does have
ED, and not a dysfunction of libido, ejaculation or orgasm. Various questionnaires have been formulated to aid the physician in this manner, as well as determining its severity. The most commonly used is the International Index of Erectile Function (
IIEF;
Table 9.2).
This is composed of 15 questions (full version), which can be completed prior to consultation (
Rosen et al., 1997). Specifically, it is important to determine the time of onset and duration, the particular situations where occurring, and the intensity of the problem. This is in order to classify the nature of
ED, so any further diagnostic evaluation can become more focused. Essentially,
ED can be of psychogenic or organic cause, or indeed mixed, which is thought to be currently the most common aetiology (
Melman and Gingell, 1999). Those of an organic nature tend to report an insidious onset of symptoms, which is not situational, with poor or absent nocturnal and morning erections. Directed questions can include assessment of the quality of the
erection. A reduction in penile rigidity (normally expressed as a percentage of their best) and sustainability may indicate a haemodynamic component, particularly veno-occlusive dysfunction. Pain or deformity of the penis may indicate Peyronie’s disease (
Roddy et al., 1991) (
9.1).
A full current and past medical history should be acquired, in order to elucidate relevant risk factors. This should involve a cardiovascular, neurological, metabolic and hormonal, and psychiatric history. Any past history of surgery and trauma, including complications, should be noted. A drug history is important, as there are many medications, such as antihypertensives (diuretics, β-blockers) that can cause impotence (
Slag et al., 1983). Recreational drugs in the form of cigarette smoking, alcohol, marijuana and cocaine, are also associated with
ED. Common causes of arterial insufficiency that can be identified include diabetes, hypertension, smoking, hyperlipidaemia and previous pelvic surgery. Corporal veno-occlusive dysfunction may occur due to previous injury or surgery to the penis, Peyronie’s disease, as well as diabetes and hyperlipidaemia leading to changes in the fibroelastic properties of the corporal tissue (
Roddy et al., 1991).
Physical examination
A full physical examination is mandatory, to assess for any direct causes, as well as any associated risk factors. The external genitalia should be examined for general sensation and anatomical deformities, such as Peyronie’s plaques.
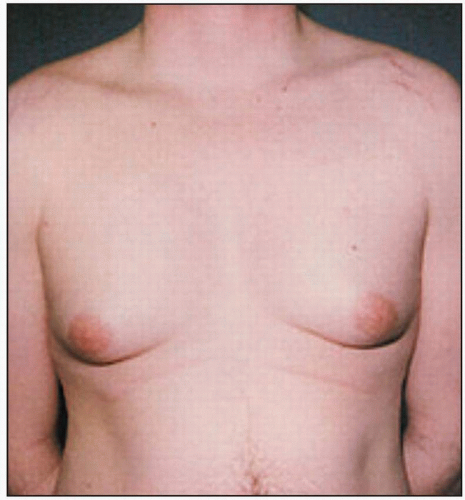
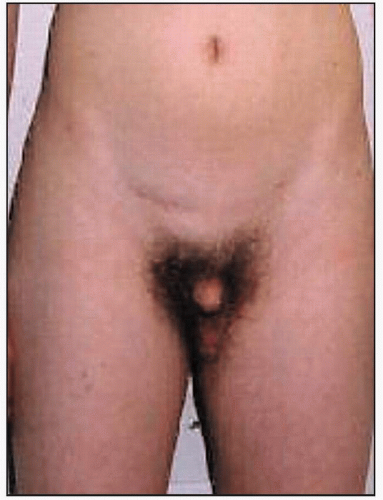
A rectal examination may reveal prostate cancer, prostatitis and reduced anal sphincter tone. The bulbocavernosal reflex can also be performed. The endocrine system should be assessed in the form of general thyroid status, looking for gynaecomastia (
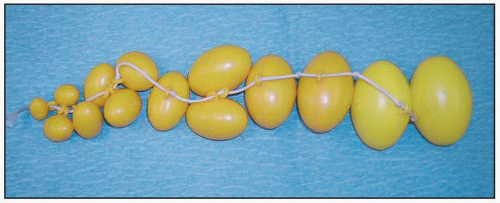
9.3) and small testes, suggesting hypogonadism (
9.4).
The patient’s vascular status should be sought through blood pressure measurement, peripheral pulses and any evidence of peripheral vascular disease (
9.5).
Laboratory tests
Most patients should be offered basic laboratory tests, such as baseline haematological and biochemical blood tests, lipid profile, and a random blood plasma glucose sample. Other tests can be directed through clinical suspicion, such as liver function tests, serum testosterone, prolactin, thyroid function, follicle-stimulating hormone and luteinizing hormone tests.
Non-surgical management of erectile dysfunction
Following a full history and examination, the treatment options can be discussed with the patient. It is reasonable at this point to commence a trial of medical management, provided there are no contraindications. However, it is important to explain that this may be unsuccessful, but that there are further investigative studies that may be of benefit, and surgical approaches for selected cases. The management of
ED has changed dramatically from the common use of penile prostheses in the 1970s, to intracavernosal injections, and now the choice of type 5 phosphodiesterase (
PDE5) inhibitor medications, and even transurethral therapy (
Table 9.3). The initial approach should always be to address the patient’s lifestyle characteristics. Smoking cessation, diet modification (including reduced alcohol intake), weight reduction (in obesity) and stress management are all simple but effective measures.