Intrarenal Collecting System
Terri J. Vrtiska MD
Case 8-1
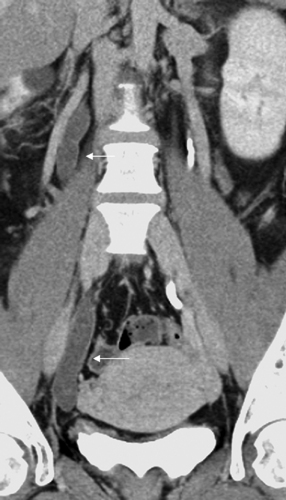
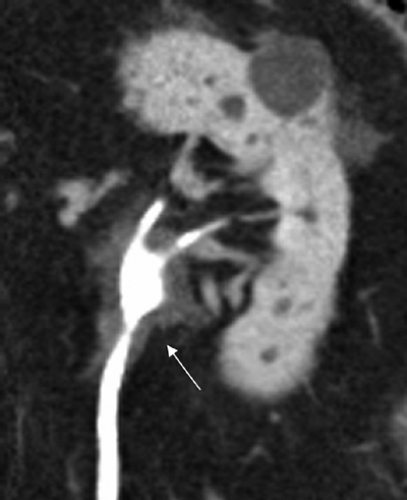
History: 69-year-old female with microscopic hematuria and recurrent stone disease.
Findings: Unenhanced volume rendered coronal image of the left kidney (A) demonstrates two small calculi in the lower pole of the left kidney (arrow). Enhanced maximum intensity projection image of the left kidney obtained during the excretory phase (B) and enhanced volume rendered image of both kidneys also obtained during the excretory phase (C) demonstrate multiple brushlike and round collections of contrast material throughout the papillae of both kidneys (arrows).
Diagnosis: Medullary sponge kidney
Discussion: Renal tubular ectasia is diagnosed by identifying linear collections of contrast material in the collecting ducts appearing as linear, paint brush-like striations (see Cases 4-10 and 11-2). The discrete linear collections (that resemble a paint brush) should not be confused with the indistinct normal papillary “blush” (see Case 4-2). Relative to CT in the past, the improved spatial resolution of multidetector CT allows for both the diagnosis and the depiction of the extent of this abnormality of the upper urinary tract collecting system.
One or more papillae may be affected. The findings are bilateral in 60% to 80% of cases. The isolated finding of linear collections is termed benign renal tubular ectasia. When the collections are cystic and associated with urolithiasis or medullary nephrocalcinosis, as in this case, the term medullary sponge kidney can be applied. Clinical presentation includes infection, symptomatic stone disease, and/or hematuria.
Case 8-2
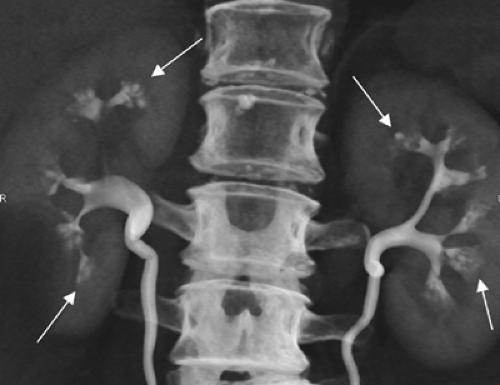
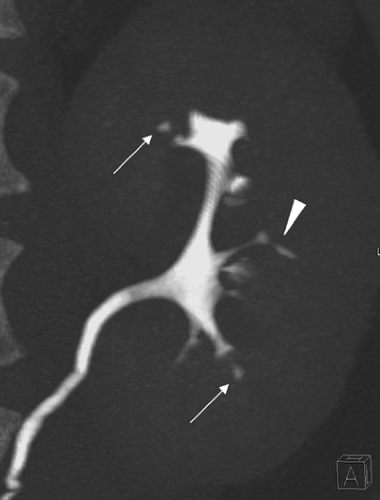
History: 19-year-old female status post bilateral ureteral reimplantation for reflux nephropathy.
Findings: Coronal volume rendered combined nephrographic/excretory phase images of the right (A) and left (B) kidneys and the entire urinary tract (C) from a CT urogram using the split bolus technique demonstrate duplication of the right intrarenal collecting system and ureter. There are bilateral parenchymal scars, particularly in the upper poles of both kidneys (arrowheads). In the right upper pole, there is a small, linear-shaped collection (arrow) of contrast material in the papilla adjacent to a scar. There is also mild caliectasis bilaterally.
Diagnosis: Reflux nephropathy (chronic pyelonephritis)
Discussion: Historically, reflux nephropathy has been referred to as chronic pyelonephritis (see Cases 6-10 and 7-1) and is associated with vesicoureteric reflux (VUR). However, reflux nephropathy is the preferred term because the changes seen in this condition almost always result from VUR during childhood. Although VUR often disappears during adulthood, the resulting mild caliectasis and renal parenchymal scars persist. Renal parenchymal scarring that results from reflux nephropathy can be differentiated from scarring due to renal infarcts. Ischemic infarcts are limited to the cortex and do not affect the underlying calyces, whereas reflux nephropathy scars involve the full thickness of the renal parenchyma and are associated with caliectasis. Reflux nephropathy can lead to progressive renal failure in adults. Approximately 10% to 20% of patients requiring dialysis or renal transplantation are due to progressive renal parenchymal loss from reflux nephropathy.
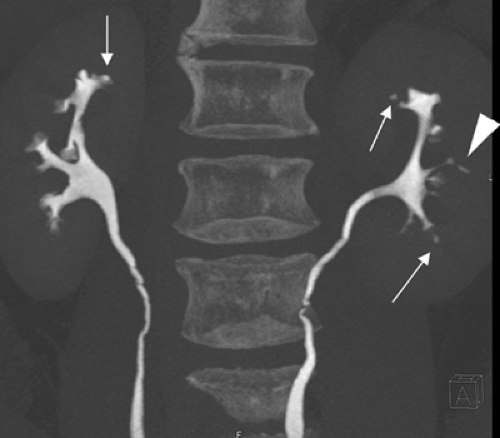
Case 8-3
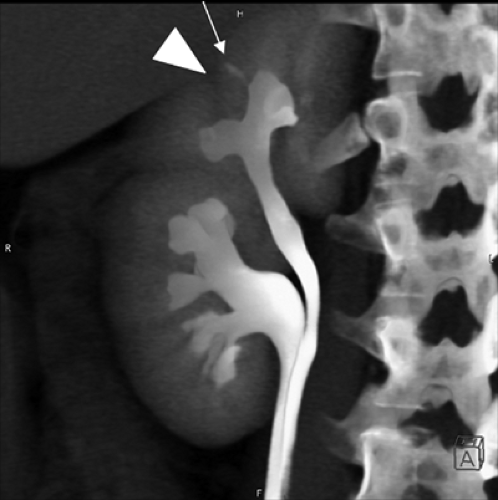
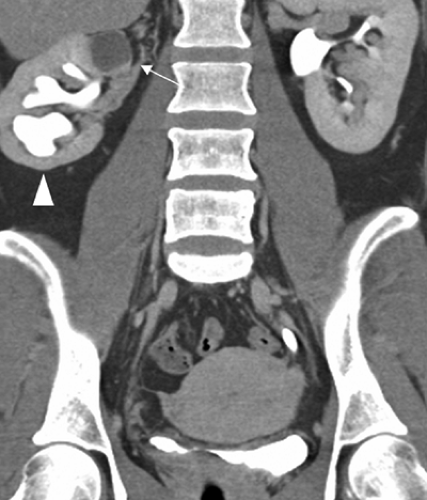
History: 39-year-old female with microscopic hematuria, flank pain, and a right-sided ureterocele on cystoscopy.
Findings: Coronal thick slab maximum intensity projection images (A, C), axial image (B), and volume rendered image (D) obtained during the excretory phase of a CT urogram performed using split bolus technique demonstrate a nonopacified cystic lesion in the upper pole of the right kidney [arrow in (A)] as well as moderate dilatation and parenchymal scarring of the lower pole of the right kidney [arrowhead in (A)]. Opacified ureteral segments are noted on the axial CT image [arrowheads in (B)]. An unopacified tubular structure, consistent with a dilated ureter of an obstructed right upper pole moiety, is best demonstrated on the thick coronal maximum intensity projection series [arrows in (C)], a segment of which is also seen on the axial image [arrow in (B)]. The volume rendered image (D) demonstrates only the opacified intrarenal collecting systems and ureters bilaterally. The unopacified right upper pole renal collecting system can only be suspected by its impression upon the lower pole renal collecting system. These findings combined with a ureterocele noted at cystoscopy are consistent with an obstructed right upper pole moiety of a duplicated intrarenal collecting system as well as with vesicoureteral reflux and scarring in the lower pole moiety.
Diagnosis: Ureteral duplication with upper pole moiety obstruction and lower pole moiety reflux
Discussion: The findings of a duplicated system, a dilated upper pole moiety ureter, lower pole atrophy, and a ureterocele detected at cystoscopy are consistent with an obstructed upper pole moiety of a duplicated intrarenal collecting system as well as with vesicoureteral reflux and scarring of the lower moiety of the right kidney. In this case, chronic obstruction led to parenchymal loss and cystic change in the right renal parenchyma. However, in other cases, the upper pole moiety may be markedly hydronephrotic; the resultant extensive downward displacement of the lower pole moiety causes the “drooping lily” sign. Duplication of the intrarenal collecting system and ureter is a common, often asymptomatic congenital anomaly. Some form of collecting system duplication anomaly is found in 15% of patients. A consistent relationship of the duplicated ureters’ insertions into the bladder occurs in 85% of patients: The upper pole moiety ureter inserts in a position inferior and medial to the lower pole moiety ureter. This anatomic relationship is known as the Weigert–Meyer rule. The upper pole moiety ureteral insertion site in the bladder is ectopic (i.e., located in an anomalous position either in or outside the bladder). The ectopic ureter is also often associated with a ureterocele.
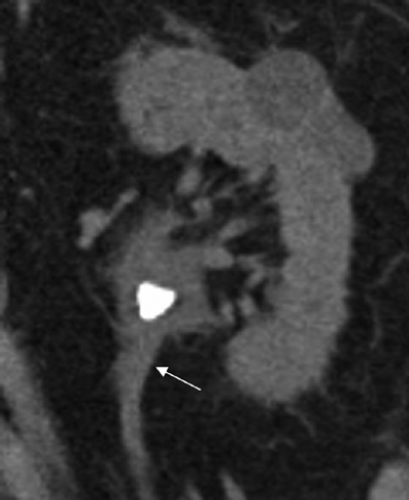
Case 8-4
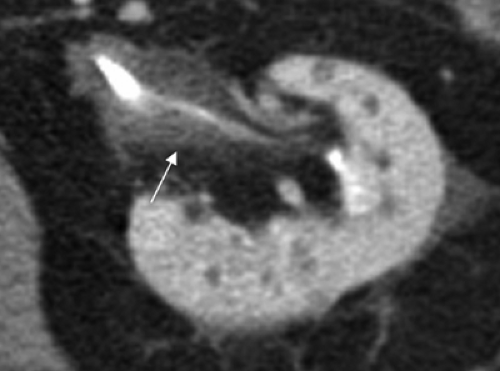
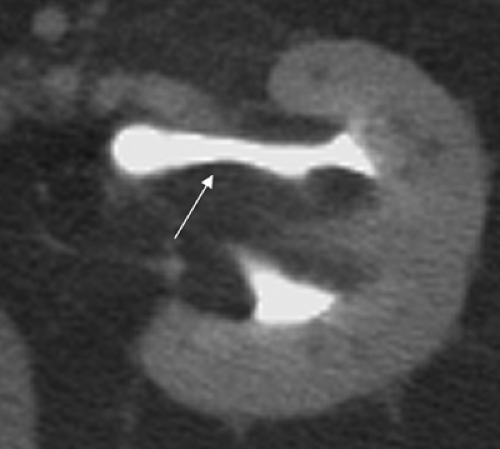
History: 28-year-old male with history of stone disease.
Findings: Axial image of the right kidney (A), coronal maximal intensity projection image of the right kidney (B), and volume rendered image of both kidneys (C) obtained during the excretory phase of a CT urogram demonstrate a well-circumscribed contrast material-filled structure (arrows) arising from an upper pole calyx of the right kidney. Images (B) and (C) best demonstrate the communication of the structure with the normal right intrarenal collecting system via a narrow isthmus from an upper pole fornix.
Diagnosis: Congenital calyceal diverticulum
Discussion: A congenital calyceal diverticulum is a urothelial-lined outpouching of the urinary collecting system that is connected to a peripheral calyx via a thin necklike infundibulum most commonly in the upper or lower pole of the kidney (see Case 7-5). Approximately one-third of diverticula are complicated by stone disease (see Case 4-13). Additional complications include infection and abscess
formation, which may necessitate treatment such as stone extraction or ablation.
formation, which may necessitate treatment such as stone extraction or ablation.
On standard CT images obtained prior to excretion of contrast media into the renal collecting systems, these appear as water attenuation masses and are likely to be confused with cystic renal masses or abscesses. However, congenital calyceal diverticula generally can be differentiated from these lesions because they opacify with contrast material on the excretory phase images obtained during CT urography due to their communication with the renal collecting system. Renal cysts and abscesses rarely communicate with the intrarenal collecting system (see Case 6-4).
Coronal images acquired with CT urography are helpful for depicting the anatomic relationship of the diverticulum with the rest of the intrarenal collecting system, prior to percutaneous interventional treatment or surgery.
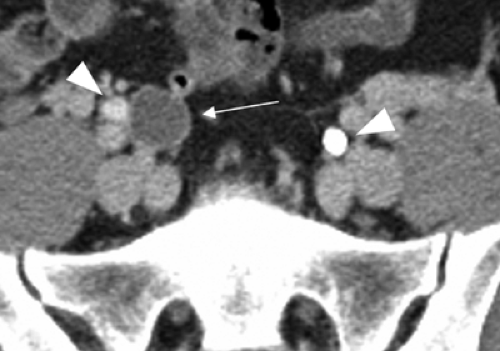
Case 8-5
History: 57-year-old male with history of gross hematuria. Medications include nonsteroidal anti-inflammatory drugs (NSAIDs), aspirin, and acetaminophen.
Findings: Coronal maximum intensity projection images obtained during the excretory phase of a CT urogram including localized views of the right kidney (A), the left kidney (B), and both kidneys (C) demonstrate a small extracalyceal contrast material-containing collection involving the upper pole of the right kidney [arrows over right kidney in (A) and (C)] and several small extracalyceal contrast material-containing collections involving the upper and lower pole of the left kidney [arrows over left kidney in (B) and (C)] as well as an eccentric linear collection extending into the lateral midportion of the left kidney [arrowheads in (B) and (C)].
Diagnosis: Papillary necrosis
Discussion: Papillary necrosis may present in patients with flank pain, hematuria, or decreased renal function. It can develop as a result of vascular compromise, infection, or obstruction of the sensitive renal papillae (see Case 6-9). Some of the traditional causes of papillary necrosis are no longer a concern clinically (e.g., phenacetin). However, papillary necrosis is associated with the ingestion of several currently used medications (e.g., NSAIDs) as well as common underlying medical conditions (diabetes, urinary tract infection, sickle cell anemia, and sickle cell trait). Changes of papillary necrosis demonstrated by CT urography are due to tracking of excreted contrast material into central or eccentric papillary cavities that communicate with calyces. Additional findings include calyceal blunting and renal parenchymal scarring. The “lobster-claw” sign of papillary necrosis is due to complete sloughing of the central papilla with distortion of a residual “claw-shaped” calyx. Rare findings include filling defects within the collecting system due to the total amputation and sloughing of papillae.
Case 8-6
History: 83-year-old male with history of diabetes, stone disease, hematuria, and flank pain.