| 19 | Interventional Tumor Therapy |
 Pathology of Malignant Colon Tumors
Pathology of Malignant Colon Tumors
The vast majority of malignant colon tumors are epithelial adenocarcinomas (ca. 80%), while the remainder (ca. 20%) are mucinous adenocarcinomas. Signet-ring cell carcinomas and undifferentiated carcinomas are very uncommon as are nonepithelial malignant colon tumors (e.g., malignant lymphomas and fibrosarcomas), the latter comprising less than 1% of all colon tumors. Malignant lymphoma is primarily localized in the cecum and is infiltrative or polypoid, growing rapidly, and metastasizing early without signs of stenosis. It is usually detected late when symptoms of pain, fever, and possibly ascites appear. The most common localization of colon carcinoma (adenocarcinoma) is in the rectum (40%). However, colon carcinoma can only be excluded with certainty using total colonoscopy. In nearly 5% of patients, there are secondary or third carcinomas. Metastasis first involves regional lymph nodes, then supplying arteries, and finally occurs as distant spread in the liver, bones, lungs, and peritoneum. Distal rectal carcinoma metastasizes primarily also in the brain, skin, bones, and neighboring organs (bladder, vagina).
 Indications for Endoscopic Tumor Therapy
Indications for Endoscopic Tumor Therapy
Adenomas with severe dysplasia (carcinoma in situ) can be curatively treated by means of endoscopic polypectomy or mucosectomy (for flat adenomas). Rectal T1 carcinomas (T1Sm1, N0, M0) can also be removed by means of endoscopic resection of the intestinal lumen. However, there is a 3% risk of lymph node invasion. Thus, among younger patients and among patients with higher tumor stages, transabdominal resection should be attempted if possible.
The major indications for interventional endoscopic tumor therapy are:
 preoperative hemostasis,
preoperative hemostasis,
 preoperative removal of an obstruction/ileus,
preoperative removal of an obstruction/ileus,
 palliative tumor therapy in inoperable patients (advanced tumor stages or older comorbid patients).
palliative tumor therapy in inoperable patients (advanced tumor stages or older comorbid patients).
 Hemostasis Methods and Relief of Obstruction
Hemostasis Methods and Relief of Obstruction
Bleeding tumors can be most expediently treated with argon plasma coagulation (20–50 W). Injection of tissue glue (fibrin or acrylic glue) or application of hemoclips is seldom necessary.
Ileus symptoms can be relieved by inserting a decompression tube, traversing the stenosis with a metal stent, or by using ablative methods such as laser and argon plasma coagulation (APC). These three procedures have all but replaced cryptotherapy. Tumor control using ethoxysclerol or alcohol has not gained acceptance everywhere; PDT and therapeutic ultrasound of the colorectal area are still in the experimental phase.

Fig. 19.1 Laser equipment, ND:YAG laser (Medilas II, Dornier, Munich).
 Palliative Tumor Therapy in Inoperable Patients
Palliative Tumor Therapy in Inoperable Patients
Laser
Results. Table 19.1 shows results achieved in 83 consecutive patients by the working group of headed by J.F. Riemann (5). Median long-term survival rate was nine months (0.25–116 months).
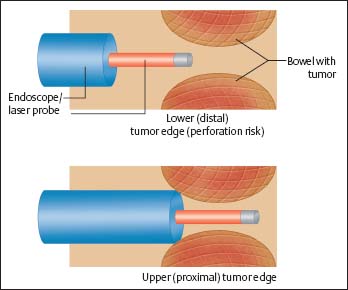
Fig. 19.2 Laser ablation/APC tumor ablation, schematic illustration.
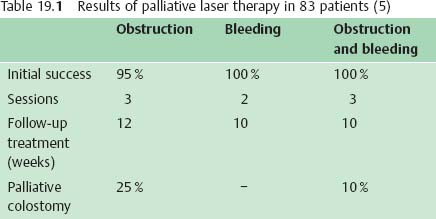

Fig. 19.3 Balloon dilation, tumor stenoses prior to laser/ APC application.

Fig. 19.4 Coagulation vapor must be suctioned during APC ablation.
Complications. The greatest concern in terms of complications is hemorrhage, which can lead to abscess, peritonitis, and fistulization. Hemorrhage occurs in ca. 2–5% of patients and must be treated with abscess drainage and antibiotics. Colostomy is often unavoidable.
APC (Argon Plasma Coagulation)







