Fig. 12.1
Storz HD fixed video camera with its control unit

Fig. 12.2
Storz HD pendulum video camera

Fig. 12.3
Fiber-optic cables of different diameters

Fig. 12.4
Storz Xenon light source
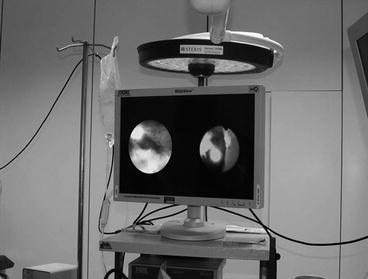
Fig. 12.5
Storz 16:9 HD monitor

Fig. 12.6
Video tower housing all video network devices
The standard-definition (SD) analogic video signal (with the transformation of the endoscopic image into an electromagnetic wave thanks to a chip on the camera head sent to a standard monitor) has been nowadays largely overcome by the digital high-definition (HD) systems (exploiting serial waves of numbers instead of a simple electromagnetic wave). Digital HD systems must be supported by an adequate video network, in order to avoid to lose the advantages of such improved image quality.
12.1.1 Camera Heads and Their Setting
The Storz HD camera heads (H3-Z and the latest pendulum version) (Fig. 12.1, 12.2) have an optimized weight and ergonomic handling, reducing fatigue and improving control during procedures. The integrated 3-chip camera head with the latest CCD (charge-coupled device) sensor technology assures detailed, high-contrast, quasi-3D, and noise-free images, with natural color reproduction across the entire zoom range. Ergonomically located buttons allow to program the camera head features according to the endoscope in use. HD camera heads have a 16:9 aspect ratio versus the 4:3 of the SD camera heads, increasing by more than 35 % the amplitude of the endoscopic field and by five times more the image resolution.
Since these camera heads have been conceived for laparoscopic procedures, thus for vision in wide-body hollows and to be coupled with big optics, the transposition of their use in ureteroscopy and nephroscopy requires a particular setting, in order to obtain an optimal vision.
Rigid, semirigid, and flexible ureteroscopes and nephroscopes require preliminary white balance, with the exception of the digital CMOS flexible nephroscope. Enhancement and brightness are set up according to the instrument to be used and the size/color of the working space (ureter versus renal pelvis and calyces):
Low enhancement and small endoscope A/low brightness for the rigid nephroscope;
Filter A enhancement and small endoscope A brightness for the flexible nephroscope;
Enhancement off and small endoscope B brightness for the semirigid ureteroscope;
Filter B enhancement and small scope B brightness for the flexible ureteroscope.
12.1.2 Light Source and Optic Cables
Optic cables with different diameters (2.5 mm for all flexible endoscopes and the semirigid ureteroscope, 3.5 mm for the rigid nephroscope) (Fig. 12.3) differ in the amount of light transmitted. The Xenon light source should also be regulated in order to avoid bad vision due to too much light and tissue reflection. In addition, injecting too much light into the cable does not improve luminosity, but light transforms into heat and burns the optical fibers of the endoscope.
The flexible digital CMOS (Complementary Metal-Oxide Semiconductor) nephroscope has a distal chip directly transforming the image into a digital signal on the tip of the instrument and needs no light source nor optic cable or white balance, having an integrated LED (light-emitting diode) technology in the handle (enhancement off, zoom × 2).
12.2 Imaging Equipment
The operating table for RIRS/PNL has to be radiolucent, with the possibility to translate it for housing the C-arm and to avoid radiopaque transverse bars underneath. Furthermore, the patient must have the chance to be put in lithotomic position (see also Chaps. 11 and 19). For a supine PNL, it is better to use an independent C-arm rather than an X-ray device integrated to an endourology table, requiring two different tables for the right and left side, or to change the position of the patient upside down (putting the head in the place of the feet) (see also Chap. 3). The individual C-arm (Fig. 12.7) can be placed as required either on the right or on the left side of the patient, leaving all the needed space to the surgeon. If fluoroscopy-only guidance is used, it is also important to be able to tilt the C-arm towards head or legs of the patient. This allows to target the kidney first in the anteroposterior incidence, then with a 30° tilt of the C-arm cephalad, to obtain information about the depth of the needle trajectory (see also Chap. 11) [1]. In order to maximally decrease radiation exposure of both patient and surgical staff and also to improve safety of the puncture, the combined use of ultrasound (Fig. 12.8) is crucial.
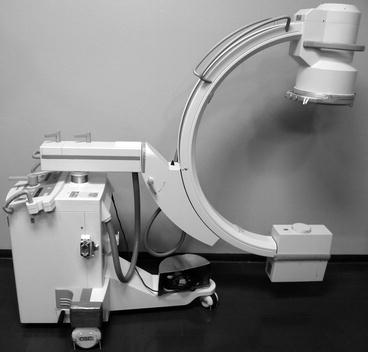

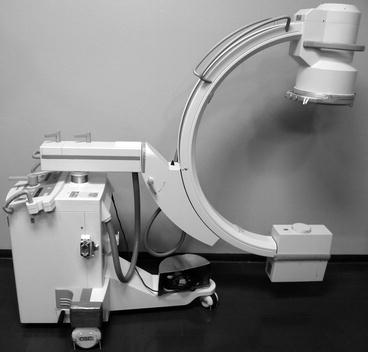
Fig. 12.7
Independent C-arm for fluoroscopy

Fig. 12.8
Ultrasound device
12.3 Nephroscopes and Ureteroscopes
The choice of the nephroscope is of utmost importance. Rigid nephroscopes have the advantage of a superior optical quality due to the rod lens system. The optimal nephroscope should have a sufficient working length, a large working channel, a reduced outer diameter, and a watertight entry site for instruments and accessories.
In older nephroscopes the cranked (Fig. 12.9) or 45° offset optics and the light cable were located on opposite sides of the shaft. Therefore, in supine position, collision with the border of the surgical table of this type of nephroscope could occur, resulting in limited maneuverability. For this reason, when we started with ECIRS years ago, we changed the kind of support under thorax and ankle of the patient, in order to enlarge the space of movement of the instrument.
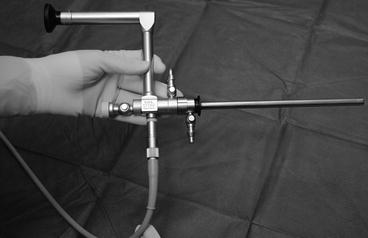
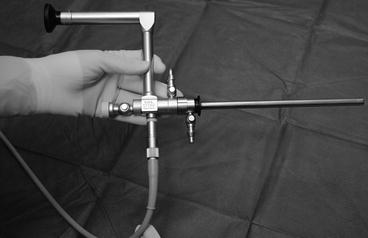
Fig. 12.9
Cranked offset optics with the light cable on the opposite side of the shaft in first-generation nephroscopes
Presently, all major manufacturers produce models in which the optical and light cables and the irrigation lines are all located on the same side of the shaft (Fig. 12.10a, b). With such nephroscopes, problems due to a conflict with the surgical table are only exceptionally encountered. Most nephroscopes have a continuous flow design, with an inflow and an outflow valve. However, when using a plastic Amplatz sheath, the outer shaft with the outflow valve loses its role; in fact, the irrigation fluid can flow out between nephroscope and Amplatz sheath. Furthermore, the shaft additionally increases the diameter of the scope, and this can be a disadvantage when accessing a calyx with a narrow infundibulum. Therefore, it is preferable to choose a nephroscope that can also be used without the outer shaft.
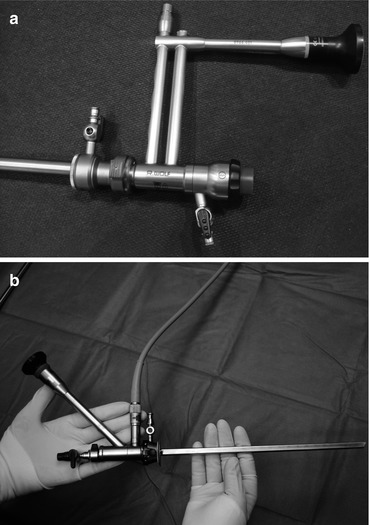
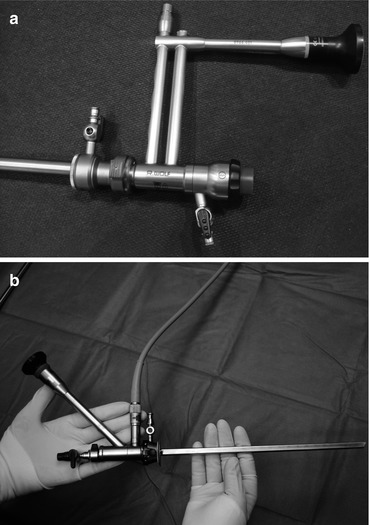
Fig. 12.10
Wolf (a) and Olympus (b) nephroscopes
In the market there are also midi (Fig. 12.11) and mini-nephroscopes (Fig. 12.12a, b, c).
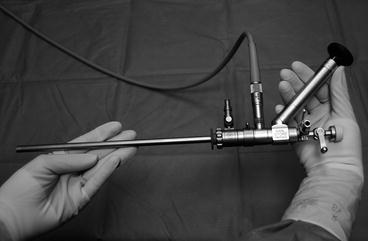
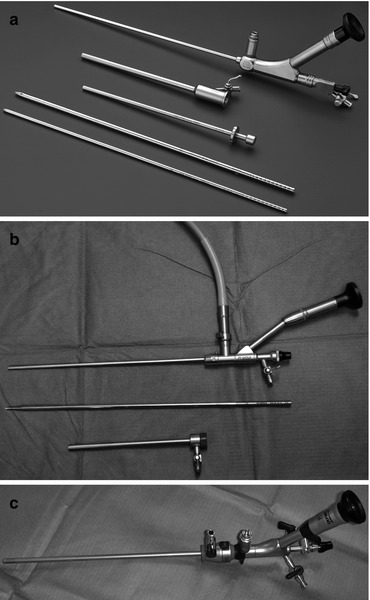
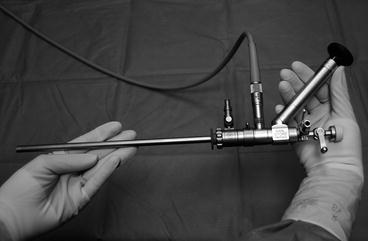
Fig. 12.11
Storz 17 Ch with outer shaft of 22 Ch rigid nephroscope
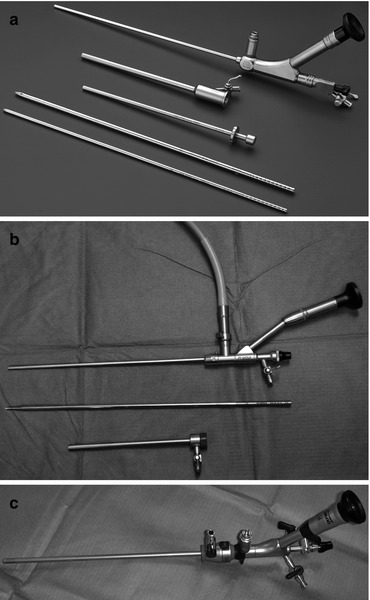
Fig. 12.12
Mini-PNL set with Storz (a) Wolf (b) Olympus (c)
A flexible cystoscope is crucial during a contemporary PNL/ECIRS. It allows to access peripheral calyces that are not reachable with a rigid instrument. This allows to avoid the need for multiple tracts, especially in case of staghorn stones. The limitation of analogic flexible instruments (Fig. 12.13a) is the small diameter of the working channel and their perceived inferior optical quality, because of the “honeycomb” effect produced by the fiber-optic bundles. Actually this can be adequately corrected by the right set up of the filters. Digital nephroscopes (Fig. 12.13b) have a very high quality of imaging. Usually the lithotripsy energy source for any flexible instrument is the laser, because of the reduced diameter and significant flexibility of the fibers employed.
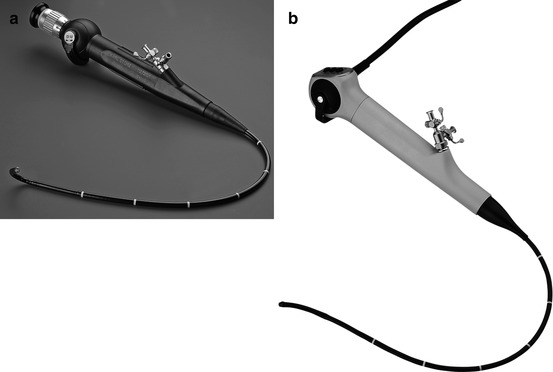
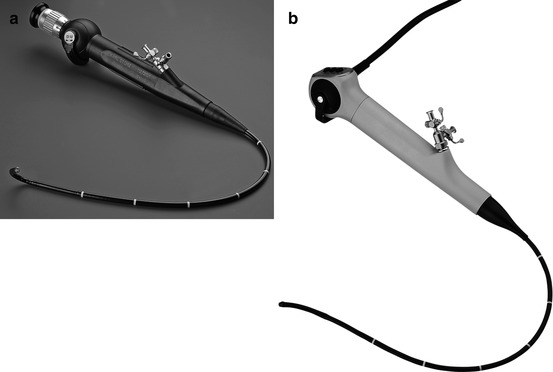
Fig. 12.13
Analogic (a) and digital (b) flexible Storz nephroscopes
One of the major advantages of the supine position is its ability to use two endoscopes simultaneously, one through the Amplatz sheath and the other transurethrally. In case of simultaneous renal and ureteral stone, the latter can be treated with a rigid ureteroscope (Fig. 12.14a, b, c) and holmium laser. The use of a ureteroscope has also the advantage of preventing the migration of small fragments into the ureter during fragmentation. In addition, through the ureteroscope it is possible to maintain a continuous and abundant irrigation which helps washing out small fragments through the Amplatz throughout the fragmentation process.
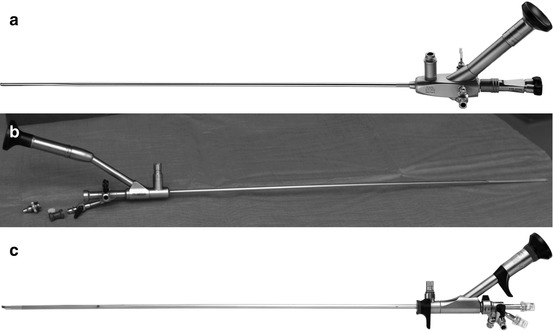
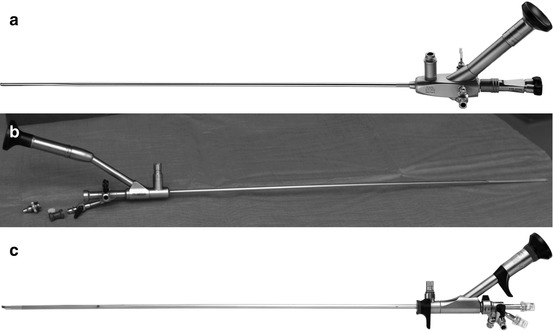
Fig. 12.14
Storz (a) Wolf 6–7.5 Ch (b) and Olympus (c) semirigid ureteroscopes
The use of flexible ureterorenoscope (Fig. 12.15) retrogradely together with a rigid or flexible nephroscope anterogradely allows to reach any district of the renal cavities. For this reason among the instruments semirigid and flexible ureteroscopes must be at disposition.
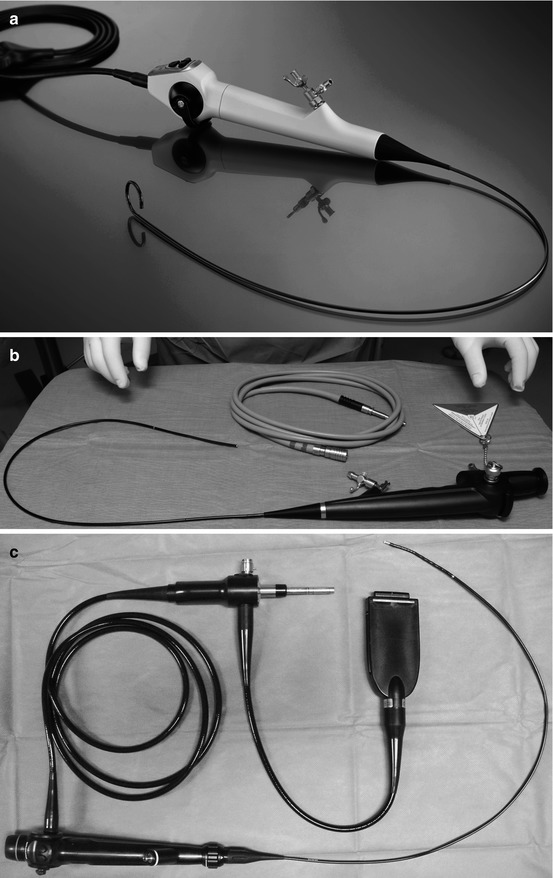
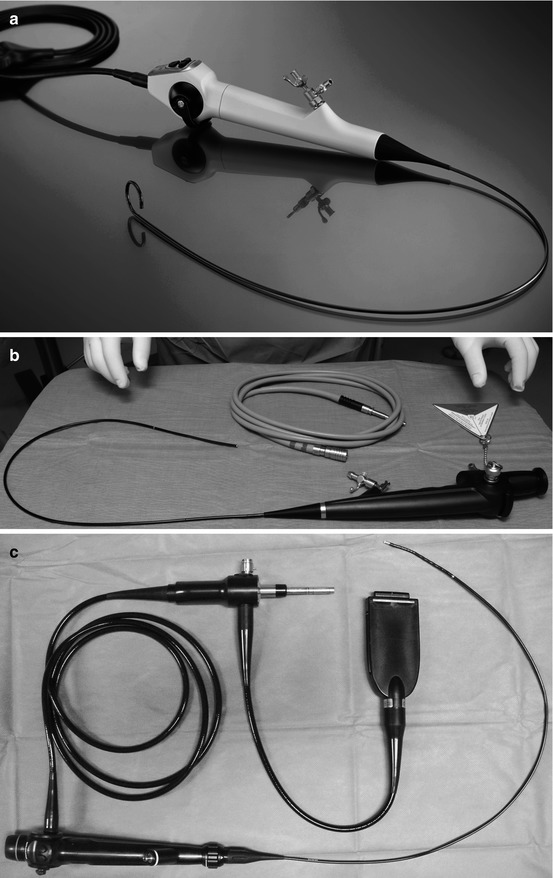
Fig. 12.15
Storz flexible video-ureterorenoscope Flex-XC (a) Wolf fiber-optic analogic Viper (b) and digital Olympus (c) flexible ureteroscopes
In summary, in order to achieve maximal efficiency during ECIRS, the optimal set of endoscopes includes rigid and flexible nephroscopes and rigid and flexible ureteroscopes.
12.4 Irrigation Systems
12.4.1 Facing the Issue of Hypothermia
During percutaneous surgery, continuous irrigation with saline is required. Because of the amount and duration of such irrigation at room temperature, hypothermia is a concrete risk for the operated patient. Thus, heating to 38 °C of the irrigant fluids is fundamental. There are specific urologic systems that deliver large volumes of irrigation at body temperature, with optimal flow rates and offering a bubble-free field of vision (Fig. 12.16). If such a device is not available, an alternative is the use of a microwave oven. The only thing to remember is to switch off the heating during ultrasound lithotripsy, in order to avoid overheating. This precaution is not necessary when using laser and ballistic lithotripsy.


Fig. 12.16
Level 1 device by Smiths Medical for sustaining/elevating the irrigation bags (a) and for heating (b)
12.4.2 Facing the Issue of Optimal Endoscopic Vision and Intrarenal Pressures
During a supine PNL, the Amplatz is roughly horizontal (see also Chap. 13). Therefore, the pressure in the collecting system is near to 0 H2O cm. Pressure can be even negative, when using an ultrasonic lithotripter, because of its suction effect. Consequently, the renal pelvis can be collapsed during the whole procedure, and air bubbles may interfere with optimal vision.
Some surgeons use a peristaltic pump in order to obtain increased flow rate and intrapelvic pressure. The Level 1 irrigation and heating column produced by Smiths Medical can be used for all kind of nephroscopes and ureteroscopes (and for resectoscopes as well), combining the advantage of heating the irrigation fluid flowing without air bubbles with the possibility to vary the height of the column (see also Chap. 14), thus varying the gravity pressure of the flow of one or two simultaneous fluid bags (Fig. 12.16).
If a retrograde ureteroscopy is performed at the same time of PNL, the ureteroscope should have its own irrigation line. The role of a port seal is essential to avoid to lose fluid from the endoscope (see also Chap. 19). Because of the presence of the Amplatz sheath, higher pressures can be used than during a standard ureteroscopy, without the risk of overdistension of the renal cavities. This has also the advantage of washing out the small stone fragments created by the ureteroscope through the Amplatz.
Several irrigation devices are disponible for ureteroscopic irrigation, especially when using flexible instruments. In fact, deflection and full working channels decrease irrigation, worsen endoscopic vision, and increase renal pelvic pressures. Gravity irrigation can be increased with occasional manual pressure; there are also manual (hand- or foot-assisted) devices (Fig. 12.17), pneumatic cuffs for pressurized flow, and automated devices. Care should be taken to choose a pump that is validated for urologic use, in order to avoid medicolegal consequences in case of accidents. In any case, the main issue should be to be aware of the importance of avoiding prolonged high intrarenal pressures, predisposing to pyelorenal reflux and infectious complications (see also Chap. 19).
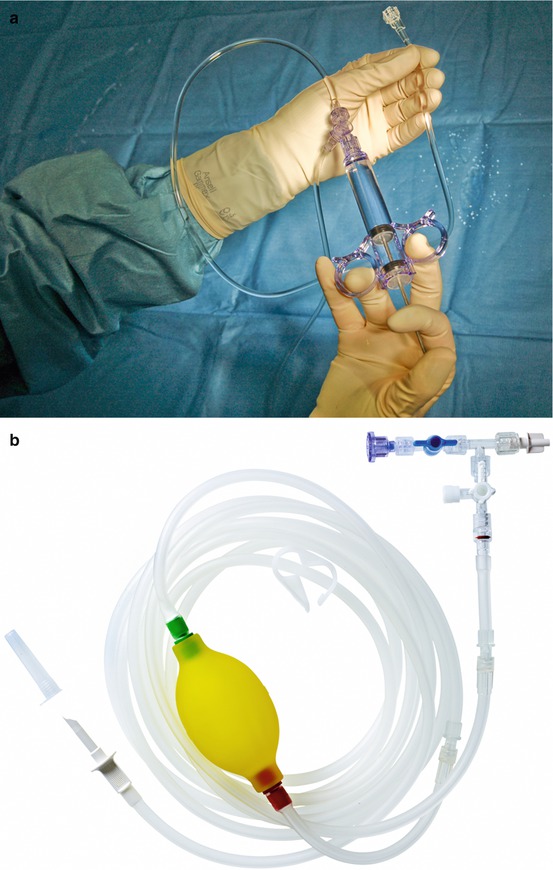
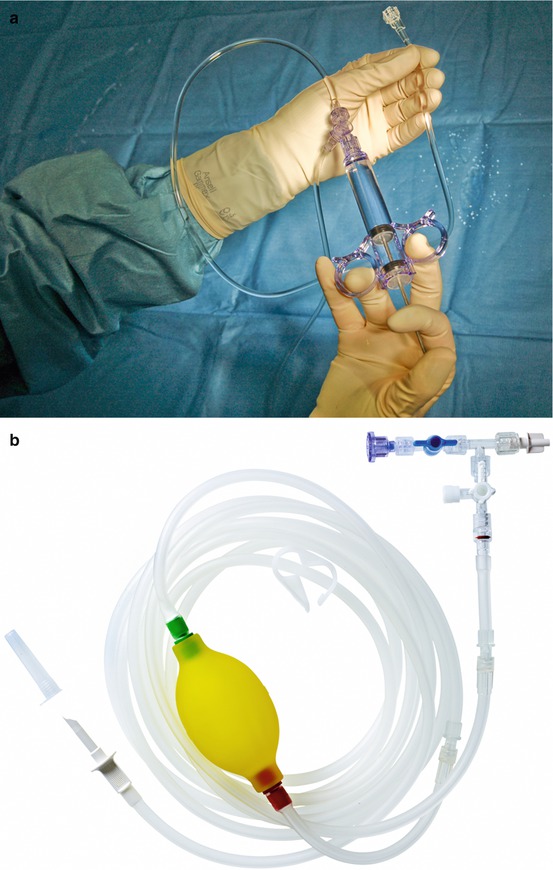
Fig. 12.17
Boston Scientific manual pump device (a) and Coloplast Porgés HiLine irrigation device (b)
12.5 Disposable Accessories
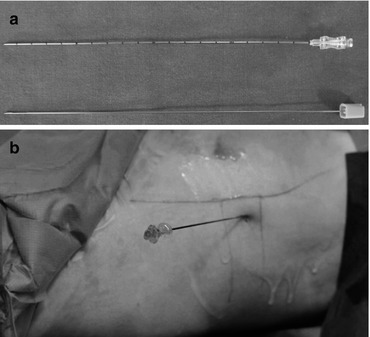
12.5.1 Access Needle
Accurate puncture of the collecting system is the fundamental initial step of percutaneous surgery. The needle should be only slightly flexible and enable soft tissue penetration, reaching deep targets without excessive deviations (Fig. 12.18). Enhanced visualization of the needle tip when used with ultrasonic imaging is essential. The 18 gauge Chiba needle is composed of a 22 gauge cannula and fitted stylet. Some urologists use a small trocar instead.