Inflammatory Bowel Disease and the Liver
Jason J. Lewis
Carl L. Berg
INTRODUCTION
Disorders of the hepatobiliary system often occur in patients with inflammatory bowel disease (IBD). As early as 1874, an association between liver steatosis and ulcerative colitis (UC) was described (1). This association, however, is not limited to UC, as further studies have described evidence of hepatic dysfunction in the setting of Crohn’s disease (CD) (2). These disorders may represent conditions that share a pathogenic mechanism with IBD, such as primary sclerosing cholangitis (PSC), disordered physiology as with cholestasis, or direct complications of IBD, such as hepatic abscess or portal vein thrombosis (3). Additionally, many of the current pharmacologic agents used to treat IBD have known liver toxicity profiles. Within this chapter, we will focus on many of the common hepatobiliary complications that a clinician can be expected to recognize and manage while treating the patient with IBD.
PRIMARY SCLEROSING CHOLANGITIS
PSC, first described in 1924 (4), is a chronic progressive cholestatic liver disease of unknown etiology characterized by inflammation of the biliary tree leading to obliterative fibrosis (5). The natural history is progressive with most patients developing cirrhosis (6). Though not as common as end-stage liver disease resulting from hepatitis C, PSC is currently the fifth most common indication for liver transplantation in the United States (7). Of those patients with PSC who have concomitant IBD, approximately 87% have UC. Between 2.5% and 7.5% of patients who present with UC have or will have PSC. Given that the prevalence of UC in the United States is estimated to range from 40 to 225 per 100,000 people, the estimated prevalence of PSC would be approximately 1 to 6 per 100,000 people (8).
While the cause of PSC is unknown, there are many proposed pathologic mechanisms. Some of these include chronic portal bacteremia, toxic bile acid metabolites produced by enteric flora, chronic viral infections, ischemic vascular damage, and genetic abnormalities of immune regulation (8). Study of the proposed pathophysiology has yet to result in promising medical therapy.
The clinical presentation of PSC is often asymptomatic or subtle, with many patients presenting with vague symptoms of malaise, weight loss, and pruritus. However, 10% to 15% of patients present with symptoms concerning for acute cholangitis, such as right upper quadrant pain, fever, and jaundice (9).
Initial evaluation often begins with detection of a cholestatic abnormality in routine liver chemistry and should lead the clinician to rule out cases of secondary cholangitis. Laboratory abnormalities are not limited to elevated serum alkaline phosphatase and bilirubin. γ-Glutamyl transferase (GGT) in one study was found to be elevated in 94% of patients, even in the setting of a normal alkaline phosphatase, demonstrating an increased sensitivity for detecting PSC (10). Thirty percent of patients have hypergammaglobulinemia with specifically increased levels of IgM (11). Many other autoantibodies are found elevated in PSC, lending further support to the proposed immunologic pathology including, antineutrophil cytoplasmic antibodies
(p-ANCA) (12), antineutrophil nuclear antibodies (ANNA) (13), antinuclear antibody (ANA), and anticardiolipin antibody (11). The diagnosis of PSC is rarely made solely on the basis of abnormal lab values. The gold standard for diagnosis of PSC is direct visualization of the biliary tree that demonstrates classical structuring and beading of the bile ducts as seen in Figure 14.1 (14). Visualization is usually performed by endoscopic retrograde cholangiopancreatography (ERCP); however, magnetic resonance cholangiopancreatography (MRCP) is gaining favor as a result of improvements in noninvasive imaging. Direct comparison between the goldstandard ERCP and MRCP has shown favorable results in the detection of PSC, with MRCP demonstrating a sensitivity and specificity of 97% and 64%, respectively, and an overall accuracy of 84% (15). Liver biopsy is often nonspecific in the diagnosis, with stages progressing from portal triad inflammation to cirrhosis, while the pathognomonic “onion-skinning” lesions are not often seen (8). Therefore, the diagnosis is routinely made based on biliary imaging and staging of disease determined by liver histology.
(p-ANCA) (12), antineutrophil nuclear antibodies (ANNA) (13), antinuclear antibody (ANA), and anticardiolipin antibody (11). The diagnosis of PSC is rarely made solely on the basis of abnormal lab values. The gold standard for diagnosis of PSC is direct visualization of the biliary tree that demonstrates classical structuring and beading of the bile ducts as seen in Figure 14.1 (14). Visualization is usually performed by endoscopic retrograde cholangiopancreatography (ERCP); however, magnetic resonance cholangiopancreatography (MRCP) is gaining favor as a result of improvements in noninvasive imaging. Direct comparison between the goldstandard ERCP and MRCP has shown favorable results in the detection of PSC, with MRCP demonstrating a sensitivity and specificity of 97% and 64%, respectively, and an overall accuracy of 84% (15). Liver biopsy is often nonspecific in the diagnosis, with stages progressing from portal triad inflammation to cirrhosis, while the pathognomonic “onion-skinning” lesions are not often seen (8). Therefore, the diagnosis is routinely made based on biliary imaging and staging of disease determined by liver histology.
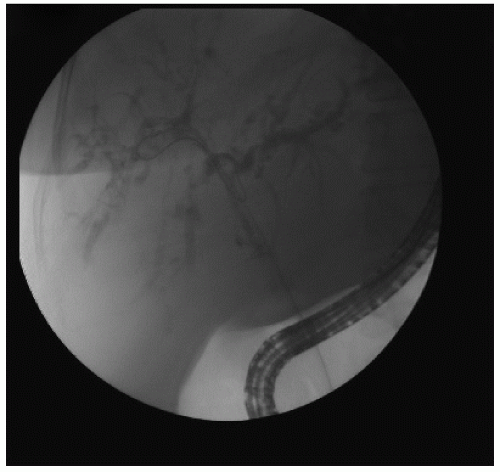 FIGURE 14.1 An endoscopic retrograde cholangiogram from a patient with primary sclerosing cholangitis demonstrating diffuse biliary stricturing characteristic of the disease. |
Medical therapy currently remains very limited, with endoscopic management of symptomatic strictures and liver transplantation for definitive therapy being the primary interventions. Treatment with ursodeoxycholic acid (Ursodiol) has shown benefit for patients with primary biliary cirrhosis (PBC); however, studies in PSC have not duplicated this benefit/result. Comparison with placebo was associated with an improvement of alkaline phosphatase, aspartate aminotransferase, bilirubin, and albumin, but showed no clinical benefit overall (16). For many patients the pruritus of PSC can be severe, and bile sequestering resins, such as cholestyramine, can be very effective in providing symptomatic relief (17).
Endoscopy can be an effective tool in the treatment of symptomatic strictures of PSC, ranging from pruritus to bacterial cholangitis. Repeated balloon dilation and stenting to maintain patency of the biliary tract has been studied and has suggested a survival advantage at 5 years when compared to the
predicted survival of that cohort using the Mayo Clinic survival model; 83% versus 65% (18).
predicted survival of that cohort using the Mayo Clinic survival model; 83% versus 65% (18).
In the setting of PSC resulting in advanced or end-stage liver disease, transplantation is the treatment of choice. Patients with cirrhosis due to PSC are subject to the same complications of spontaneous bacterial peritonitis, portal hypertension, and hepatic encephalopathy as other etiologies of cirrhosis. Five-year patient survival rates posttransplant are >85% for most centers (19). Recurrence of disease is relatively common in the grafted liver. Patients with PSC have a higher incidence of acute cellular and chronic ductopenic rejection compared to a non-PSC control group (20), further supporting the proposed pathophysiology of ongoing inflammation in PSC.
The most feared complication of PSC is cholangiocarcinoma, with a reported incidence of cholangiocarcinoma in PSC of 6% to 11% (3); however, this may be underreported. The diagnosis of cholangiocarcinoma can be very difficult to make in the setting of PSC in part due to the overlap of symptoms between the two. An attempt to characterize those with PSC who are at risk for cholangiocarcinoma has demonstrated that those who smoke and have variceal bleeds complicating their course are at increased risk, with no association being found between the duration of PSC and the incidence of cholangiocarcinoma (21




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






