(1)
Department of Vascular Surgery, Evangelisches Krankenhaus Königin Elisabeth Herzberge, Berlin, Germany
An infection of a vascular access for hemodialysis constitutes a serious complication which particularly occurs in immuno-compromised patients. Many infections are avoidable. The influence of puncture techniques on infections is discussed in Chap. 17.
7.1 Prevention of Infections
Infections occuring directly after surgery have other causes than later ones. Therefore they are discussed separately.
7.1.1 Prevention of Perioperative Infections when Creating a Vascular Access
An infection arises with contamination and supporting local factors.
The microbial contamination of a wound may be minimized by:
A thorough shave of the operative and prepped fields.
Covering the field with incise film when using vascular prosthetic grafts.
Other Influences That Favor Infections Which Can Be Influenced
1.
Correct timing of surgery. For obvious reasons do not operate during septicemia.
2.
Potential catheter locations. If you operate on an upper extremity, preferably use the side that is contralateral to a catheter, as otherwise (increased flow velocities after AV access surgery) this might facilitate bacteremia if there is bacterial colonization of the catheter.
3.
Choose the correct incision. The skin incision should be placed directly over the vessels which were selected for anastomoses to avoid large cavities. With a few exceptions (incision at the apex of a looped graft, creation of a distal cephalic fistula), choose longitudinal incisions only.
4.
Use atraumatic operative techniques. Use bipolar diathermy with a fine forceps only. Don’t pull apart the wound edges more than necessary.
5.
Maintain careful hemostasis. It should not be necessary to place a drain except for special cases.
6.
Close wounds in layers in order to avoid subcutaneous cavities.
7.
Perform redo surgery in time if a hemotoma requires this step.
8.
Consider the intraoperative administration of antibiotics when using prosthetic grafts.
7.1.2 Prevention of Perioperative Infections in Redo Surgery
Redo surgery sometimes necessitates the exposure of the vessels in places where they are covered by only a thin layer of subcutaneous tissue. Thus the risk of a wound infection is increased. As mentioned above, a longitudinal incision parallel to the vessel, meticulous hemostasis, and exact wound closure including the subcutaneous tissue are important factors.
7.2 Therapy of Infections of AV Fistulas
7.2.1 Early Postoperative Infections
Early postoperative infections are extremely rare after the creation of AV fistulas (0.1 % in our patients over the last 13 years). Long operations, large wound areas, and hemotomas favor infections. With slight superficial soft tissue infections, the administration of antibiotics and additional cooling may be sufficient. Redo surgery is necessary with deep infections reaching the vessels in order to remove necrotic and infected tissue. After thorough flushing and drain placement, the wound is closed completely. In the few such cases that we have observed, the evacuation of hematomas or abscesses, wound debridement, and additional administration of antibiotics have led to complete restitution while preserving functioning fistulas.
7.2.2 Late Postoperative Infections
Late postoperative infections are much more frequent than early infections. In the majority of cases they involve frequent punctures sites which lie close to each other. From a clinical point of view there are three kinds of late infections:
Inflammatory infiltration of the skin and subcutaneous tissue over the vein
Isolated necroses at puncture sites
Extended soft tissue infections of the punctured vein
Inflammatory Infiltration Of The Skin And Subcutaneous Tissue Over The Vein
Characteristics are erythema, edema, and painfulness.
Therapy
Antibiotics, local cooling, and immobilization.
Isolated Necroses at Puncture Sites
Isolated, mostly 2–8 mm slough and necrosis cover the puncture site with or without inflammation of the surrounding tissue.
Frequently there is a tissue defect corresponding in size to the crust which extends through the tissue to the vessels. Only the existence of an intraluminal thrombus adjacent to the wall prevents bleeding. Mostly there are no inflammatory signs of the surrounding tissue.
Therapy
Depending on morphological conditions (subcutaneous position, mobility of the vein, topographical considerations), the surgical therapy varies.
Local Excision
While the assistant manually compresses the vein, the surgeon transversally excises the affected tissue and vascular defects, closes the vessel, the subcutaneous tissue, and the skin. This is only possible in a few cases (Fig. 7.1a, b).
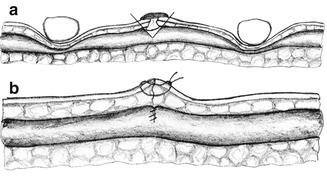
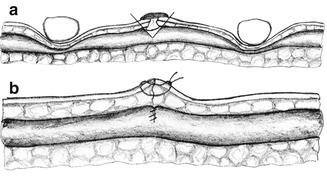
Fig. 7.1
Treatment of infected puncture site of a fistula. (a) Excision of the infected tissue under manual compression of the vein. (b) After completion
Resection of a Segment
Also under manual compression, the infected puncture site is exposed via a transverse incision. After the oval excision of the infected puncture site, the afferent and efferent sides of the vein are mobilized (if possible) and reunited after resection of the affected segment. It is important to cover the anastomosis sufficiently (Fig. 7.2a, b). Antibiotics are selected according to bacterial sensitivity.
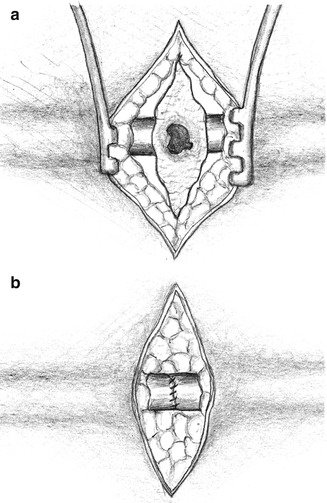
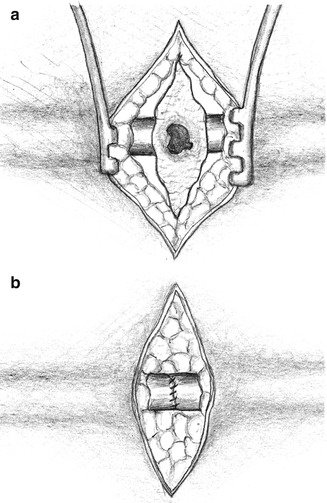
Fig. 7.2
Segmental resection of the infected puncture site of a fistula. (a) After isolation of the relevant segment. (b) After completion
Extended Soft Tissue Infections Of The Punctured Vein
Extended soft tissue infections of the punctured vein frequently also show intracutaneous bullae and skin necroses.
Therapy
Depending on the state of the vein proximal to the infected site.
Vein Proximal to the Infection Suitable for Punctures (Fig. 7.3)
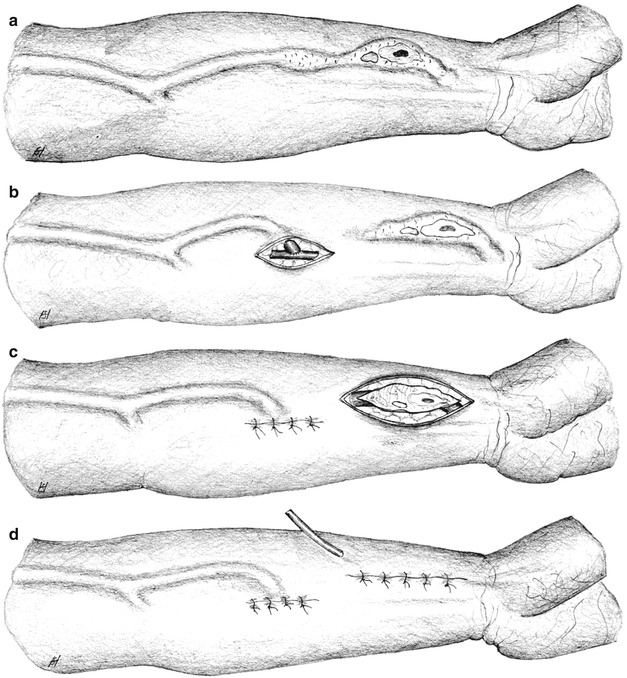
Fig. 7.3
Course of action for extended distal infection of a fistula whose proximal segment is suitable for puncturing. (a) Baseline status. (b) After proximal new anastomosis. (c) Isolation of the infected venous segment. (d) Final result
Apply incise film.
Isolate the vein and the corresponding artery in an area which is definitely not infected, make a longitudinal incision, transect the vein and anastomose the proximal stump to the corresponding artery (Fig. 7.3b).
After closing the first wound, cover it with incise film to prevent microbial spread.
Make a spindle-shaped incision circumscribing the infected vein and free the vein up to the anastomosis (Fig. 7.3c).
Ligate the anastomosis, resect the infected vein, insert a drain, and close the wound (Fig. 7.3d).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








