Fig. 24.1
T2-weighted fast spin-echo transverse (a) and coronal (b) MR images and corresponding coronal ADC map (c) obtained using an endovaginal coil in a woman with stage Ib1 tumor. An area of diffuse abnormal intermediate signal intensity (arrows) is seen on T2-weighted images (a, b), which corresponds with area of restricted diffusion in (c) (arrow), lending greater confidence to diagnosis of invasive cervical carcinoma
Parametrial extension can be assessed on both CT and MRI, although image contrast is better on the latter. Both result in false-positives from interpreting inflammatory soft tissue strands as invasive tumor; comparison with hysterectomy specimens showed an accuracy of 87% for MRI, 80% for CT and 82.5 % for examination under anesthesia [25]. Images transverse to the cervix are preferred [26]. There is no advantage in using fat-suppression [27], neither does contrast-enhancement provide additional benefits (accuracy of parametrial extension 83 % on T2-W images compared with 72 % for gradient–enhanced, T1-W fat suppressed images, [28]. More recently, diffusion-weighted imaging, which is proving of major benefit in diagnosis of soft-tissue tumors, has been successfully employed to improve detection of small cervical tumors: combining the information from the apparent diffusion coefficient maps derived from DW-MRI sequences with the standard T2-W data improves sensitivity and specificity from 56 and 75 % respectively to 89 and 67 % respectively [24].
Endometrial Cancer
As the primary management of endometrial cancer is surgical, T-staging of the tumor is done at histopathology. However, accurate T-staging on pre-operative imaging serves to guide the need for nodal dissection and the use of adjuvant therapies.
T2-W MRI is the preferred modality for T-staging the tumor; CT lacks contrast between tumor and myometrium. On T2-W imaging the abnormal uterus has a well-defined zonal anatomy in post-menarche, pre-menopausal women with a high signal intensity endometrial stripe, a low signal-intensity inner myometrium (junctional zone) and an intermediate signal intensity outer myometrium. In these cases, definition of an intermediate signal intensity endometrial tumor against the low signal intensity junctional zone can be relatively clear, making the assessment of myometrial invasion fairly straightforward. However, endometrial cancer primarily affects the post-menopausal age group where the zonal anatomy of the uterus disappears and the junctional zone increases in signal intensity. In these cases, outlining the extent of invasion of tumor into the myometrium lacks contrast on T2-W imaging and the use of gadolinium to highlight a poorly vascular tumor against a much more avidly enhancing myometrium is often used. However, contrast-enhanced images need to be acquired dynamically with a temporal resolution of <30 s in order to be sufficiently accurate, as after 3 min, enhancement of the tumor itself and washout of contrast from the myometrium mean that these structures become isointense with each other and contrast between them is lost. The need for high temporal resolution images acquired dynamically results in a compromise on spatial resolution, with pixel sizes of 3–5 mm and leads to a loss of sensitivity for T-staging. In postmenopausal women, the accuracy in estimating myometrial invasion with T2-W images, contrast-enhanced T1-W images, and DCE-MRI was 66.7, 77.8, and 92.6 %, respectively [29]. In a more recent study of 45 women, Nasi et al. showed that gadolinium enhancement with better temporal resolution had a global sensitivity and specificity of 90.6 and 93.3 %, respectively, with a mean Negative Predictive Value of 96,3 % and a mean Positive Predictive Value of 88 % compared to the FSE T2-W sequence (global sensitivity and specificity of 80.6 and 87.6 %, respectively, mean Negative Predictive Value 92.6 %, mean Positive Predictive Value 86 %) giving contrast-enhanced sequences a higher staging accuracy (95 % vs. 78 %) [30]. DCE-MRI images in combination with T2-W sequences give more accurate assessment of myometrial invasion [31] (Fig. 24.2). Deep myometrial invasion (>50 %) is associated with a 40 % risk of nodal metastases so that MRI has an important role in distinguishing superficial from deep myometrial invasion. More recently, DW-MRI has been shown in preliminary studies to have superior diagnostic accuracy in the assessment of myometrial invasion and significantly higher staging accuracy compared with DCE-MRI [32]. In a retrospective study of 48 patients, Beddy et al. showed diagnostic accuracy, sensitivity, and specificity, respectively, of 90, 84, and 100 % for DWI vs 71, 61, and 88 % for DCE-MRI. DW-MRI has also been successfully employed in differentiating benign from malignant endometrial lesions: derived apparent diffusion coefficient values have been shown to be significantly lower in malignant disease (0.84 ± 0.19 × 10−3 mm2/s vs. 1.58 ± 0.36 × 10−3 mm2/s, [P < 0.01]) [33–35].


Fig. 24.2
T2-weighted sagittal image (a) and DCE image (b) in a woman with stage 1a endometrial carcinoma. An intermediate T2 signal intensity mass is distending the endometrial cavity (a, blue arrow). The myometrium enhances avidly on the DCE image and the tumor enhances less avidly (b, white arrow), therefore invasion of the myometrium is more easily visualized, in this case there is minimal invasion
A minimum of two planes is required to delineate the tumor against the inner myometrium. The sagittal plane which visualizes the longitudinal axis of the endometrial cavity and a plane truly transaxial to the uterine body to image the uterus in cross-section are preferred. Spatial resolution is optimized to achieve an in-plane pixel size of 0.5 mm with a 3–4 mm slice thickness; this can be accomplished while maintaining a sufficient signal to noise ratio within the capability of most 1.5 and 3 T scanners with an external pelvic array coil. Smaller pixels merely result in an increase in image noise and a reduction in diagnostic accuracy.
Lesions within the endometrial cavity are often hemorrhagic, particularly if there has been a recent biopsy or curettage. This is a common diagnostic pitfall and can lead to an overestimation of disease burden or extent. It is therefore imperative to acquire T1-W images where sub-acute hemorrhage is easily recognized as high signal-intensity within the endometrial cavity. The irregular margins, nodularity and nodular nature of the tumor mass have also been used to differentiate endometrial stromal sarcoma from endometrial cancer [36] although in an organ where tissue sampling is relatively simple, the need for this histological differentiation on imaging is unlikely to have major clinical impact.
Ovarian Cancer
Ovarian cancer is usually recognized late because of lack of symptoms. By the time women present with abdominal distension and discomfort peritoneal dissemination is widespread with ascites. Previous studies have investigated ultrasound for screening, but these have not proved cost-effective [37]. In >3,500 women at high risk of ovarian or fallopian tube cancer screened at 37 UK centers, annual transvaginal ultrasound and serum CA125 screening had positive and negative predictive values of 25.5 % (95 % CI, 14.3–40.0) and 99.9 % (95 % CI, 99.8–100) respectively at the incident screen [38]. The longer term follow up from this study is ongoing and due to report in 2015.
Ovarian cancer is recognized by complex partly solid, partly cystic masses within one or both ovaries as disease is frequently bilateral. The solid components are in the form of nodules, septations or papilliform fronds and when recognized in these patterns are characteristic of epithelial ovarian cancer. Rarer histological subtypes (cystadenocarcinomas, endometroid adenocarcinoma and clear cell variants) may also be recognized by classical appearances of the solid components of the masses on T2-W imaging [39]. For example, granulose cell tumors are predominantly solid intermediate signal-intensity homogenous masses with small, often punctuate cystic/necrotic components. Conventional and contrast-enhanced MR imaging also are useful to evaluate morphologic features, including lesion complexity, signal intensity, and enhancement of solid areas. At dynamic contrast-enhanced MR imaging with semiquantitative analysis, early enhancement characteristics may help differentiate some complex benign and malignant lesions. Diffusion-weighted imaging has a limited but useful role in evaluating adnexal masses: Those with a hypointense solid area on both diffusion-weighted (b = 1,000 s/mm2) and T2-weighted images are likely benign, whereas those that are hyperintense on diffusion-weighted images (b = 1,000 s/mm2) with intermediate signal intensity on T2-weighted images are likely malignant [40].
The extent of peritoneal disease is still best ‘evaluated’ on CT because it enables coverage from the dome of the diaphragms to the pelvic floor within a few seconds. The associated ascites provides a low density background against which the nodules and plaques of peritoneal disease are outlined. The use of contrast agents both in CT and MRI has been explored, but their use does not provide advantages over unenhanced images [41]. Ovarian lesions generally are poorly enhancing and are not highlighted within a mesentery where normal vascular enhancement is prominent or against normally enhancing bowel wall. DCE-CT and MRI techniques lack the coverage of the whole abdomen and pelvis with sufficient spatial and temporal resolution [6]. Their utility is therefore confined to characterizing single lesions that require better delineation [42] (Fig. 24.3).
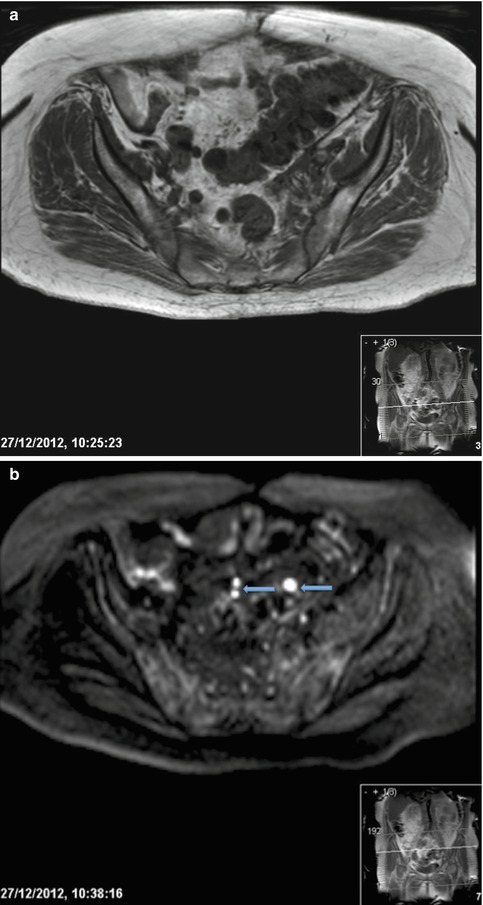
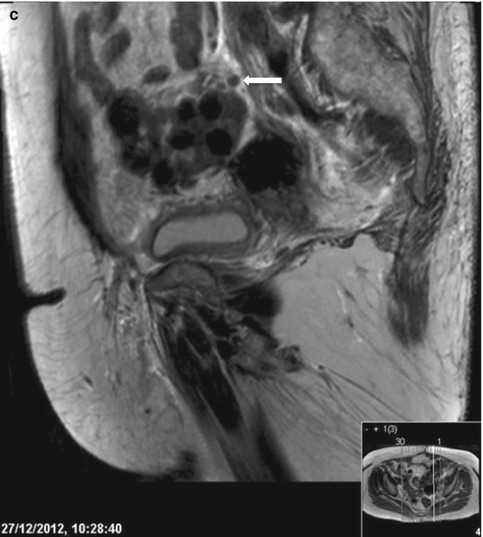
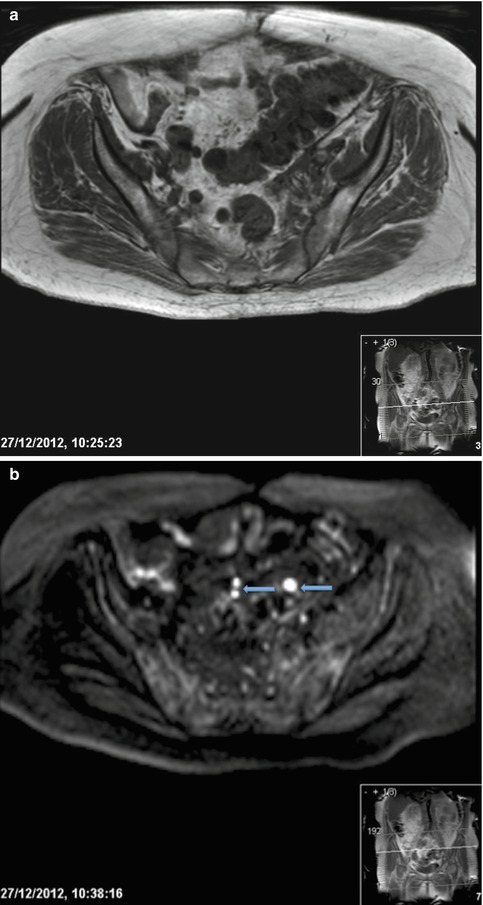
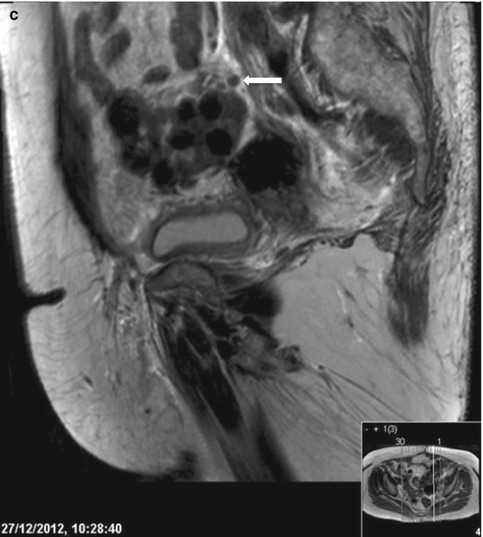
Fig. 24.3
T1-weighted axial image of the pelvis (a) and corresponding b1200 DW-MRI image (b) and sagittal T2-weighted image (c) in a woman with ovarian carcinoma. Diverticular disease is present in the sigmoid colon and the signal intensity of peritoneal and serosal deposits is similar to bowel making assessment of deposits difficult on T1-weighted images (a). DW-MRI increases the conspicuity of disease, image (b) demonstrates three areas of bright signal (blue arrows), the larger lesion is a serosal deposit and the two smaller lesions correlate with small peritoneal deposits seen on image (c) (white arrow)
Newer techniques such as DW-MRI are revolutionizing the imaging assessment of ovarian cancer, as not only is image contrast improved but they are also quantitative [43, 44]. On heavily DW images (high b-value) tumor appears bright against a dark background and is therefore easily recognized (Fig. 24.4). However, normal bowel wall also shows diffusion restriction and appears bright so that it is difficult to separate serosal deposits from normal bowel. Use of threshold values of the apparent diffusion coefficient is advocated to enable this differentiation. In future use of such thresholds and automated segmentation of lesions will enable estimations of the volume of burden of solid disease which can then be measured in longitudinal studies on chemotherapy. It should also be possible to use such information for assessing the optimal timing for debulking disease within a course of chemotherapy, thus individualizing and optimizing the surgical management in these patients.
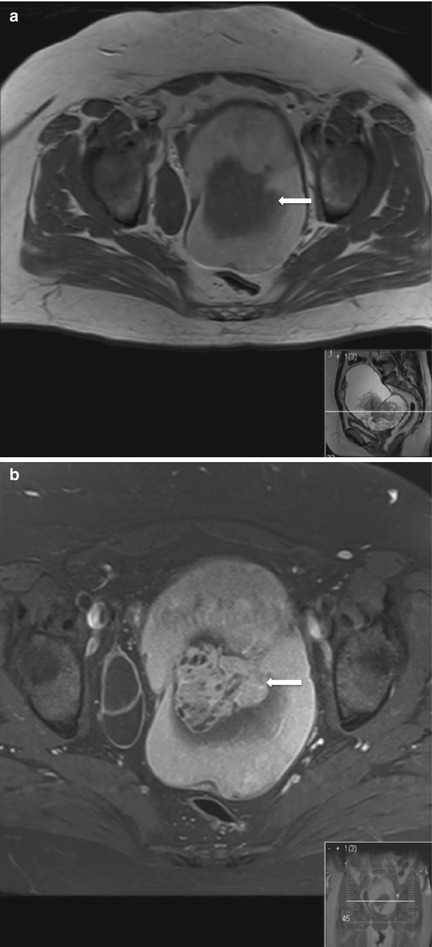
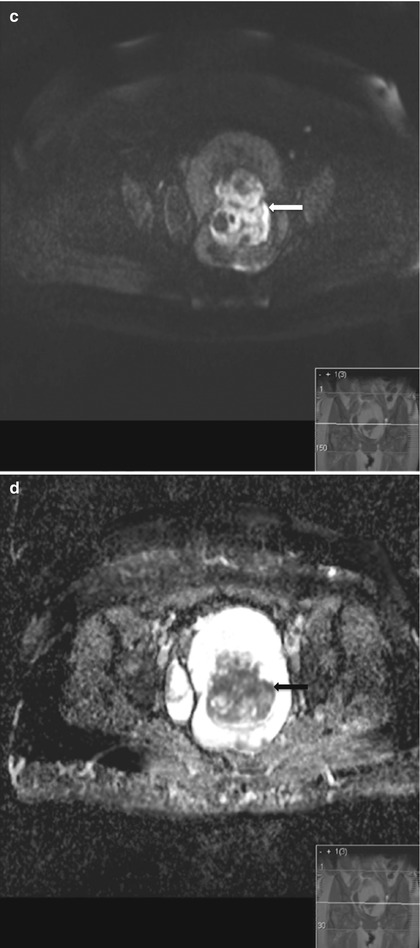
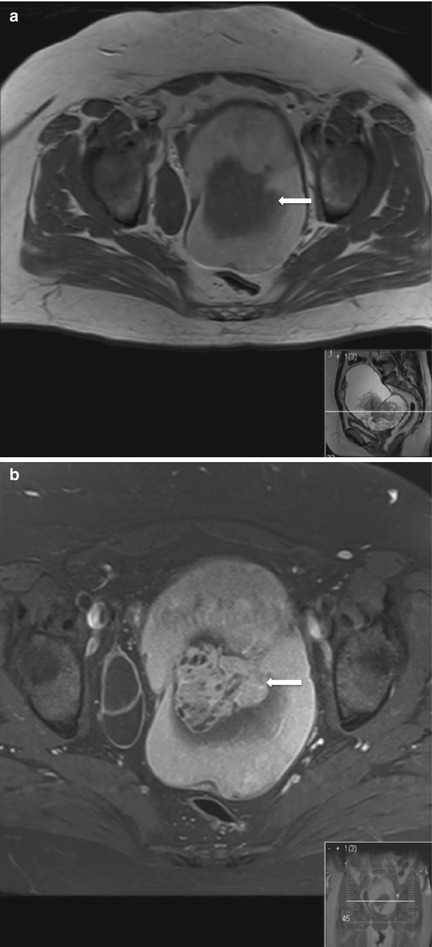
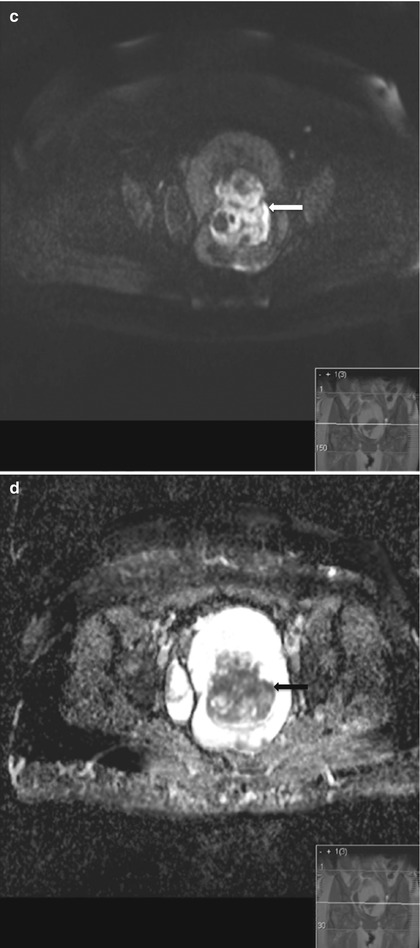
Fig. 24.4
T2-weighted axial image through the pelvis (a) with corresponding contrast enhanced image (b), b1200 DW-MRI (c) and corresponding ADC map (d) in a woman with a mucinous adenocarcinoma of the left ovary. The left adnexal mass has a high T2 signal intensity cystic component and an intermediate T2-signal intensity central solid component (a, arrow). The solid component enhances heterogeneously (b, arrow). On the high b-value DW image the solid area returns bright signal (c, arrow) with corresponding dark signal on the ADC map (d, arrow)
24.4 Imaging Nodal Stations (N-Staging)
Cervical Carcinoma
Lymph node status is the single most important prognostic factor in cervical cancer [10]. The 5-year survival rate without nodal metastases is estimated at 85 %, this reduces to 71 % with the presence of pelvic lymph nodes [45]. Lymphatic spread occurs first to the local paracervical and parametrial nodes, obturator nodes are frequent sites of disease and spread to iliac chains, para-aortic and retroperitoneal nodes although largely contiguous may not be necessarily so. Pre-operative imaging assessment aims to identify nodal disease which would require combined chemotherapy and radiation therapy rather than surgery (Fig. 24.5). Morphological features which suggest involved lymph nodes include round shape, irregular outline and size greater than 10 mm—however using this size cut-off on CT and MRI yields a low sensitivity [46]. If a parametrial lymph node is greater than 5 mm this is regarded as suspicious. Yang et al. showed that central nodal necrosis has a 100 % positive predictive value for metastases in squamous cell carcinoma of the cervix [47]. Signal intensity similar to the primary tumor also suggests nodal involvement. DWI-MRI has shown potential in detecting metastatic nodes; although some studies show significantly lower ADC values in diseased nodes compared to benign nodes [8] there is significant overlap in values which reduces specificity.
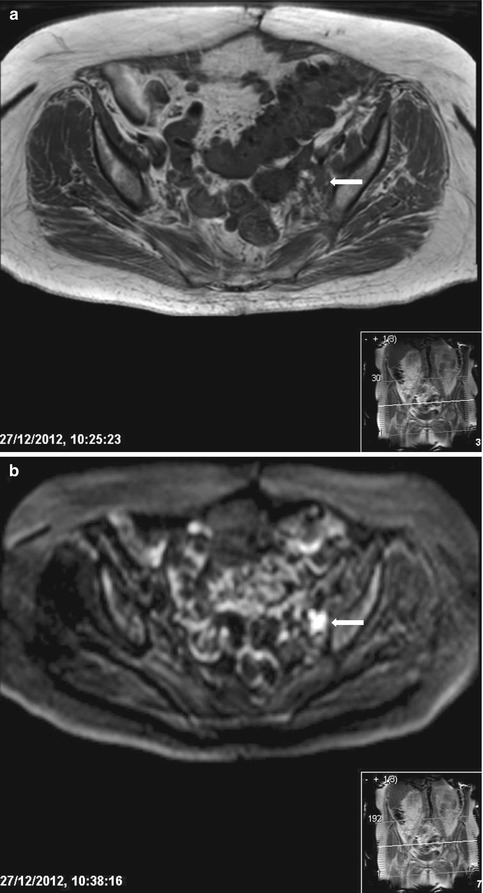
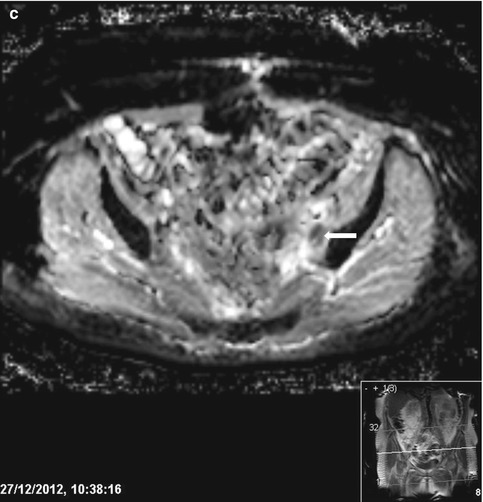
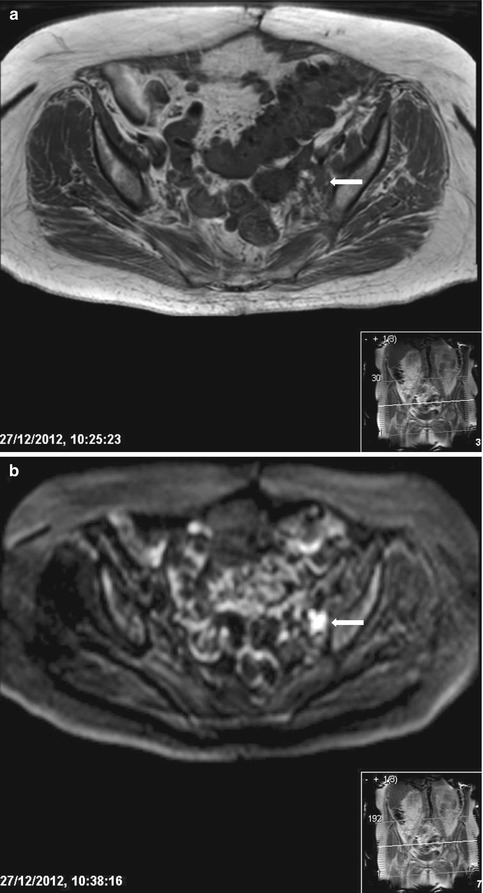
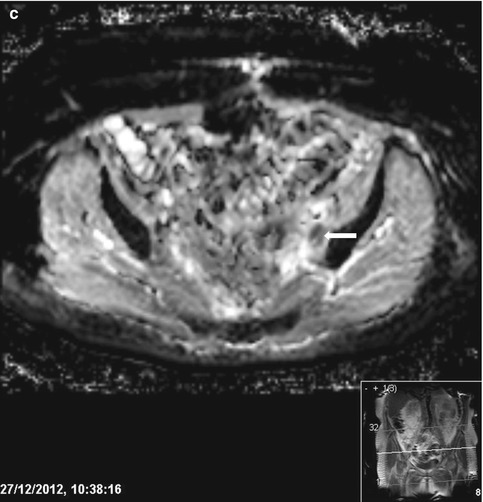
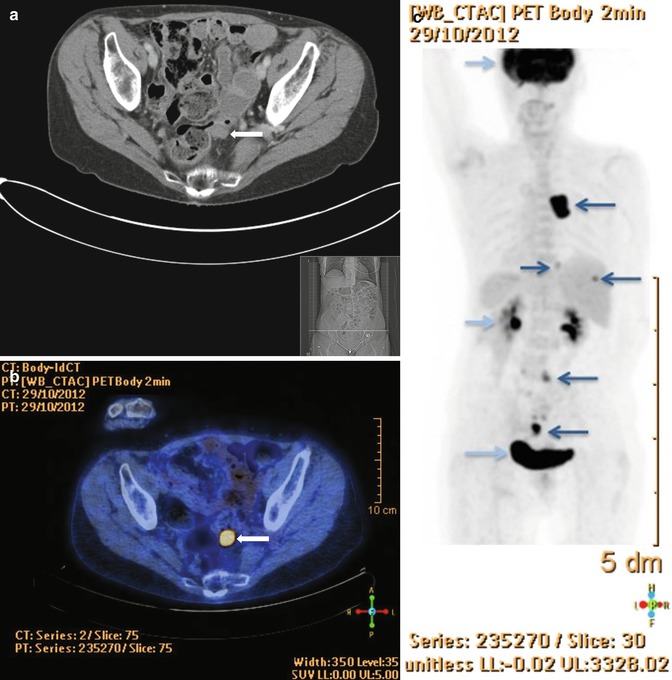
Fig. 24.5
T1-weighted axial image through the pelvis (a) and corresponding high b-1200 value DW-MRI image (b) and ADC map (c) in a patient with stage IIb cervical carcinoma. The 9 mm left external iliac node is of similar intensity to the bowel and vessels (a arrow), however the lymph node demonstrates restricted diffusion appearing very bright on the DW image (b) and dark on the ADC map (c) highlighting the value of functional MRI
18F-FDG PET/CT has been shown to be superior to MRI in detecting pelvic and para-aortic nodal disease in later stages of disease (FIGO II and greater), with sensitivities between 60 and 100 % and specificities between 55 and 95 % compared with MRI sensitivities of 71 % with no loss in specificity [47, 48]. Early work has shown that combining information from PET and MRI has higher accuracy compared to 18F-FDG PET/CT in nodal detection [49], but remains to be corroborated in larger studies.
Endometrial Carcinoma
Lymphadenectomy is part of the surgico-pathological staging of endometrial cancer but is not performed in all centers. In low FIGO stage disease (<1B) lymphadenectomy may not be performed so that pre-operative imaging is particularly important in optimal surgical planning. The depth of myometrial and cervical stromal invasion are key prognostic factors of nodal metastases; pelvic nodes >8 mm in short axis are generally considered enlarged and likely to be metastatic. The middle and lower uterus drain to regional lymph nodes in the parametrium, paracervical and obturator nodes (stage IIIC disease), whilst the upper uterus drains to common iliac and para-aortic chains. The presence of enlarged para-aortic lymph nodes is associated with the highest impact on prognosis and indicates stage IIIC2 disease [50].
As with cervical carcinoma 18F-FDG-PET/CT is useful in the detection of nodal metastases in endometrial cancer. A recent meta-analysis has shown that the overall pooled estimates for sensitivity and specificity of 18F-FDG-PET or PET/CT scans in the detection of pelvic and/or para-aortic metastasis were 63.0 % (95 % CI, 48.7–75.7 %) and 94.7 % (95 % CI, 90.4–97.4 %), respectively with an overall diagnostic accuracy of 89.5 % [51]. MRI lymphography using iron-oxide nanoparticles showed promising results in preliminary studies [46], but awaits larger scale multicenter trials when the contrast agent becomes available.
Ovarian Carcinoma
Primary lymph node drainage from the ovaries is to the para-aortic lymph nodes, secondary drainage occurs through the broad ligament to obturator, internal and external iliac lymph nodes and through the round ligament to inguinal lymph nodes. The presence of regional lymph nodes stages the disease as FIGO IIIC and is associated with a 5-year survival of 34 % [10]. Supra-renal para-aortic lymph nodes may result in a patient being unsuitable for primary surgical resection underlining the importance of imaging in pre-operative assessment. In the evaluation of nodal disease, 18F-FDG-PET/CT is the most accurate imaging technique available, as it is capable of identifying metastatic deposits in nodes deemed unenlarged by size criteria on morphological imaging. Yoshida et al. demonstrated malignant involvement in normal sized lymph nodes in ovarian cancer and showed that 18F-FDG-PET/CT improved staging accuracy from 53 to 87 % when compared with CT alone [52].
24.5 Imaging Metastatic Spread (M-Staging)
Nearly 80 % of patients with endometrial cancer present with stage 1 disease; hematogenous spread to other organs and bones is rare at presentation. The lungs are the commonest site involved [53] and sometimes peritoneal deposits are seen. Similarly, distant spread of cervical cancer to the lungs, liver and bones can occur but is rare at presentation. In contrast, the majority of patients with ovarian cancer often present with advanced disease due to the general non-specific nature of associated symptoms. Peritoneal metastases outside the pelvis including subcapsular liver deposits and/or regional lymph node metastases are common at presentation. Stage IV disease is recognized when metastatic deposits are identified beyond the peritoneal cavity or within liver parenchyma. Surgical staging is the gold-standard but increasingly where treatment is with primary chemotherapy followed by interval debulking surgery, a “staging CT” is common place with a quoted accuracy of 70–90 % [54].
CT allows detection of peritoneal disease, ascites, nodal, visceral and bone disease which aids surgical planning. Detection of peritoneal deposits depends on a number of factors, size (over 1 cm), presence of ascites, and administration of oral and intravenous contrast. Calcified deposits are easier to detect on CT. In the absence of disseminated disease, primary debulking surgery is recommended. If disease is widespread, the likelihood of suboptimal surgical debulking is high and primary chemotherapy is given. In these cases, image-guided biopsy may be necessary to provide a definitive histological diagnosis. CT features which suggest a high risk of suboptimal cytoreduction, such as extensive subhepatic disease, also may be used to select patients for laparoscopic evaluation prior to laparotomy.
Additional roles for CT are in diagnosing primary peritoneal carcinoma which cannot be distinguished from ovarian cancer pathologically as well as in identifying ovarian metastases from a gastrointestinal, breast or pancreatic primary tumor.
Newer techniques such as DW-MRI are now being increasingly investigated in whole body protocols for identifying metastases, but data acquisition techniques are still variable across scanners and, unless rigorously conducted, the examinations can be prone to significant image artifact. DWI-MRI has proven useful in detection of small peritoneal, serosal and subcapsular liver deposits which are seen as bright signal intensity areas on high b-values. DWI-MRI is also useful in detecting low volume peritoneal disease and identifying lesions in difficult anatomical locations for example the right sub-diaphragmatic space, although correlation with conventional imaging is necessary [43].
24.6 Imaging Response and Recurrence
Disease response on DW-MRI is recognized as an increase in ADC because of an increase in apoptosis and necrosis within the tumor mass increasing extracellular space and allowing more free water diffusion within the tissue. A sound basis for applying thresholds of response and non-response depends on establishing a robust measurement and understanding the limitations, particularly in a multicenter setting where equipment variations affect the reproducibility of the technique [55]. In ovarian cancer, although 18F-FDG PET/CT is still the norm for follow-up and for detecting recurrence (Fig. 24.6), DW-MRI of the pelvis and abdomen is being increasingly recognized [56]. It is currently under evaluation in a multicenter clinical trial, and may replace CT in assessing response and relapse in this disease not only because of its high sensitivity, but also because of its provision of quantifiable data. Its reproducibility is of importance in this disease where intensive longitudinal follow-up is required to recognize a pattern of relapse and remission and implement appropriate chemotherapeutic regimens as patients develop treatment related toxicities or become resistant to selected chemotherapeutic agents.