In the past decade, there has been a seismic shift in the use of imaging for Crohn disease (CD) away from small-bowel follow-through (SBFT) to cross-sectional techniques, most commonly computed tomography enterography (CTE) and magnetic resonance enterography (MRE). Because of rapid advances in CT and MRI hardware, as well as routine use of oral contrast agents designed to distend the lumen of the small bowel, cross-sectional techniques have become a first-line imaging modality, promising accurate assessment of the mucosa as well as the extraintestinal manifestations of penetrating disease. In most situations, the choice of cross-sectional modality (clinically) is essentially a tradeoff between the ease and cost of the study (which favor CTE) and the desire to minimize radiation exposure (which favors MRE).
In this new era, fluoroscopic studies, including SBFT, have been relegated to a more focused, problem-solving role including evaluation of possible obstruction and road mapping of complex fistulae. Ultrasound of the small bowel currently does not provide the comprehensive assessment of cross-sectional techniques. It is limited in the United States by the lack of Food and Drug Administration (FDA)-approved intravenous contrast agents.
Imaging of CD remains an active and evolving research topic as investigators hope to reliably differentiate active from chronic disease, predict disease response to medical therapy, and potentially assess bowel motility, while simultaneously reducing exposure to ionizing radiation. The next decade promises great steps forward.
Cross-Sectional Enterography: CTE and MRE
What is Enterography?
Enterography refers to the use of oral contrast agents designed to distend the lumen of the small bowel, without being reabsorbed. Although water may distend the upper tract, it does not provide adequate distension of the terminal ileum, the most commonly affected bowel segment in CD.
Adequate distention of the small bowel is critical for reliable and reproducible diagnostic enterography, as it facilitates evaluation of both mucosal enhancement and bowel wall thickening. If the lumen is not distended, the mucosa cannot be evaluated accurately, and collapsed bowel segments are too easily mistaken for pathologic bowel wall thickening.
In addition to distending the small bowel, oral contrast agents should be hypoattenuating (“dark”) on CT and hypointense (“dark”) on T1-weighted MRI images to allow evaluation of the adjacent, brightly enhancing mucosa. Contrast agents that are hypointense on both T1- and T2-weighted images may be additionally helpful, but are not in widespread use.
Unfortunately, in daily practice, the distention achieved by oral contrast agents is variable. This variation is in part due to physiologic differences in bowel motility, but successful bowel distension is also dependent on the patient’s ability and willingness to drink the contrast. Overall, however, routine use of oral agents has been shown to be reliable and better tolerated than enteroclysis. Although CT or MR enteroclysis may still have a role for detection of low-grade small-bowel obstruction, neither is routinely performed at our institutions.
There is no shortage of effective oral contrast preparations for enterography. As a general rule, as the osmolality of the agent increases, the palatability decreases and side effects (nausea, diarrhea, and flatulence) increase. At our institutions, we routinely use 0.1% low-density barium sulfate suspension (VoLumen, E-Z-EM, NY) for both CTE and MRE.
The volume and timing of oral contrast also vary among institutions. We currently ask patients to drink 450 mL of VoLumen (one bottle) over 15 minutes, beginning 45 minutes before imaging. They are then given a second bottle to drink over the next 15 minutes and finally 450 mL of water 15 minutes before imaging begins. We use water immediately before imaging because it is intended only to distend the proximal small bowel and we can therefore reduce the amount of hyperosmolar fluid administered and its subsequent side effects ( Fig. 1 ).

Intravenous contrast should be administered for CTE or MRE whenever possible. Standard dosing varies slightly between institutions, but whatever agent and volume is typically used for a routine abdominal CT or MRI at a given institution may be used. CT is typically performed during the “enteric” phase, approximately 50 seconds after injection (although a more standard portal venous phase will also suffice), whereas MR should be performed dynamically; that is, imaging should be performed at multiple time points (or phases) after contrast administration.
The technique outlined in the preceding, and discussed in more detail later, is how we perform enterography under ideal circumstances. Careful attention to technique results in the best chance of obtaining high-quality images and reliable, useful diagnostic information. However, one practical consideration is worth noting. What if the patient will not or cannot drink the oral contrast? In these situations, the study should be performed without it. Most patients who refuse to drink the oral contrast do so because they are too sick to tolerate it. Anecdotally, the findings in these patients will often be significant enough that they will be detected without the additional sensitivity provided by good bowel distension.
CT Enterography
The efficacy of CTE has been repeatedly proven in clinical trials and the technique has gained widespread acceptance. Mayo Clinic, for example, reported a nearly 10-fold increase in its use between 2001 and 2004. This marked increase has occurred in parallel to decreased use of the fluoroscopic SBFT, which CTE has largely replaced. Using the technique described previously, high-quality images allowing for robust small-bowel evaluation are routinely obtained with this quick, well tolerated exam.
The findings of CD on CTE have been well described and include bowel wall thickening, abnormal mural enhancement and stratification, and the “comb sign.” Mural hyperenhancement may be symmetric (nonspecific) or asymmetric (more suggestive of CD). Mural stratification, or the “target” sign, refers to the differential enhancement of the bowel wall layers: enhancing mucosa (bright), submucosal edema (dark), and enhancing serosa (bright). Bowel wall thickening is diagnosed when the small-bowel wall exceeds 3 mm in thickness in a well distended bowel loop. The presence of bowel wall thickening in conjunction with asymmetric mural hyperenhancement is essentially pathognomonic for CD. Finally, the “comb sign” refers to engorgement of the vasa recta and is highly suggestive of active inflammation ( Figs. 2 and 3 ).

There is a wide range of reported accuracy of CTE within the literature, owing in part to technologic changes/advances that often occur faster than the latest literature can reach press. But it is also due to routine use of inadequate reference standards, most commonly ileocolonoscopy. When ileocolonoscopy is used as the sole gold standard, patients with small-bowel inflammation detected on CTE (or MRE) may be misclassified as falsely positive simply because the endoscope did not reach the diseased segment. This is of particular concern in the CD population because of the prevalence of stenotic ileocecal valves, skipping of the terminal ileum, and intramural CD inflammation. In one large series of patients with suspected CD and normal endoscopic examination of the terminal ileum, 54% actually had active small-bowel disease when radiologic, serologic, and clinical factors were used as the reference standard. When the difficulties related to adequate reference standards are taken into consideration, the sensitivity of CTE for detection of CD is approximately 90%.
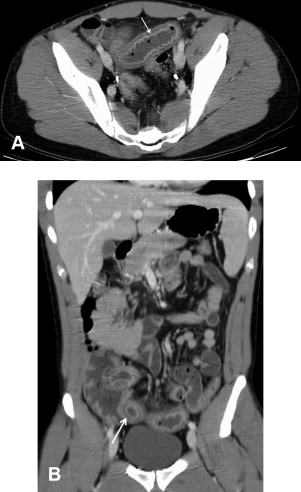
In addition to this impressive sensitivity for detecting mucosal disease, CTE reliably detects sequelae of penetrating disease, such as fistula and abscess formation, with an accuracy of approximately 94% ( Fig. 4 ). Anecdotally, the low-density oral contrast routinely administered for CTE occasionally complicates the diagnosis of interloop abscess, as both normal bowel and abscess will contain low-density fluid (as opposed to routine abdominal–pelvic CT, in which bowel contents are “bright” due to barium-containing oral contrast and abscesses are “dark” because they contain unopacified fluid). If there is difficulty deciding whether a fluid-containing structure is an abscess or a bowel loop, high-attenuation oral contrast can be administered and the study repeated. Because CTE is exquisitely sensitive for detecting active CD, it may also have a role in monitoring response to increasingly powerful (and potentially toxic) medical treatments. Persistent inflammation is a risk factor for disease progression and complications. Unfortunately, clinical symptoms do not necessarily correspond with biological activity. Subjecting a patient to repeated invasive colonoscopies increases both cost and risk, and may not be practical depending on disease location. A recent retrospective study illustrated that radiologic improvement did not correlate closely with clinical symptoms, serum biomarkers, or endoscopic appearance; however, 60% of patients did show radiologic improvement after infliximab therapy. This suggests that CTE may be an important biomarker for early disease response.

Radiation
The potential negative consequences of exposure to diagnostic radiation warrant brief discussion, as they are now in the forefront of the minds of clinicians, radiologists, and patients alike. Two recent studies evaluated the radiation dose associated with commonly ordered CT scans as well as the potential risk of radiation-induced cancer due to CT scans alone. The authors calculated a projected rate of CT-induced cancer of 1/250 20-year-old women and 1/330 20-year-old men who underwent multiphase CT abdomen/pelvis scans. The risk of CT-induced cancer decreased as the age of the patients increased. It is critical to remember, though, that these risks are theoretical and are based on principles that are at least questioned, if not rejected, by many medical physicists. However, regardless of whether we can quantify the specific risk(s) of medical radiation, we can all agree that we should strive to limit exposure to the lowest possible dose necessary for diagnosis—the so-called ALARA principle (As Low As Reasonably Achievable).
CTE exposes patients to up to five times the ionizing radiation of the typical SBFT, the test it has largely replaced. That said, the radiation dose from a single CTE is not high enough to be particularly concerning. Newer CT techniques have demonstrated a significant decrease in radiation dose using modified protocols and reconstruction algorithms. One recent study demonstrated that a 50% reduction in dose could be achieved without sacrificing sensitivity for acute inflammation. Certainly, advances in scanner hardware and software technology will continue to lower the radiation dose of CTE.
However, the inflammatory bowel disease (IBD) population has two important characteristics that should alert physicians to use radiation judiciously. Patients are typically young at the time of diagnosis, and they will often require numerous examinations throughout their lives. Indeed, the increased lifetime radiation exposure of IBD patients compared to the general population has been well documented; the majority of this exposure is due to repeated CT exams.
All medical decisions should be informed by analyzing the potential risks and benefits of any course of action as well as the potential risks and benefits of inaction. Coordination between emergency room, primary care, and gastrointestinal physicians is critical to helping minimize unnecessary radiation in the young IBD patients. Radiation exposure should not be a concern in the elderly (in whom the risk is very small) or in patients who are acutely ill (in whom the potential benefit is very high). Overall, CTE is too useful clinically and cost effective to avoid based on radiation concerns. When used appropriately, it is a powerful tool to aid in the diagnosis and management of CD. Undoubtedly, investigators will continue to develop new ways to lower radiation dose while maintaining diagnostic efficacy.
MRE
In this relatively new era of radiation awareness, what dose is acceptable? There is no doubt that the organ and effective doses of CT will decrease significantly in the next decade. But, as discussed previously, patients with IBD are unique in their youth and need for serial exams. In this population, the option of MRE, which is free of ionizing radiation, is compelling.
Evaluation of the small bowel with MRE faces one major hurdle: bowel motion. Although MR pulse sequences have become increasingly fast, a single series can require greater than 20 seconds of imaging time, during which any bowel motion blurs the resulting image. This is an issue only for the contrast-enhanced images, as the remainder of the commonly used pulse sequences for MRE (single-shot fast-spin-echo and steady-state free-precession) are sufficiently rapid. Unfortunately, although the contrast-enhanced images are the most susceptible to motion, they are also the most critical.
Most centers therefore administer pharmacologic bowel paralytics to minimize small-bowel motion. Specific techniques vary between institutions; however, 1 mg of glucagon is most commonly used whether injected intravenously or intramuscularly, in a single dose or in split doses. These agents are not necessary for CTE because of the speed of acquisition of modern multidetector CT scanners. However, just as the radiation dose of CTE is certain to decrease, the speed of MR pulse sequences will certainly increase in the near future, which may render this problem irrelevant.
The findings indicative of CD on MRE are essentially the same as CTE, including wall thickening, abnormal enhancement, and engorgement of the vasa recta, with the addition of elevated T2 signal within or adjacent to the bowel wall. Elevated T2 signal is caused by the presence of fluid and is indicative of an active inflammatory process. When present, this finding is highly specific ( Figs. 5–7 ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




