Fig. 1.1.
(a) Schematic showing guide attached to ultrasound probe for guided technique. The guide controls the angulation of the needle. (b) Schematic showing free hand technique (without guide). The operator controls the angulation of the needle. Images courtesy of Paul Wiernicki, RDMS, RVT.
Knowledge of the lesion’s location on CT or MR is used to target the lesion under US. If the lesion is difficult to see under ultrasound independently, ultrasound machines with fusion imaging capability can be used. CT and MR images from a patient’s prior study can be imported into the machine’s computer and fused with real-time ultrasound images to localize a lesion (Fig. 1.2).
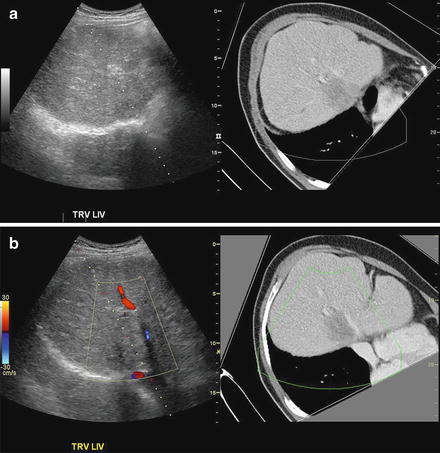
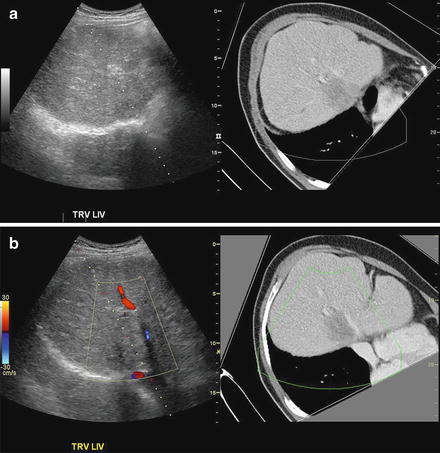
Fig. 1.2.
(a) Use of CT images to localize lesion under ultrasound with fusion technique. (b) Second image shows fusion plus color Doppler, to show absence of large central hepatic blood vessels in the path of the biopsy. Pathology of the lesion was moderately differentiated adenocarcinoma. Note the dotted line on the image, denoting the projected path of the biopsy needle.
CT Guidance
To some extent, the actual needle insertion is performed blind to minimize radiation to the patient and to the performing physician as well as to minimize artifacts from motion and from the needle. CT can be used to determine THE depth and angulation of the needle NEEDED to reach the lesion. A CT scanner equipped with CT fluoroscopy where the operator may direct the radiation to a small set of axial slices (typically three) centered around the target may be helpful in directing/redirecting the needle along the right path to the lesion. Sampling of the lesion once the target has been reached is also performed blindly with the patient outside of the CT gantry. Most CT fine needle aspirations are performed using a coaxial approach with an introducer, therefore trying to sample different areas within the INTRODUCER can be difficult.
Endoscopic Guidance
Gastroenterologists using endoscopic ultrasound perform this procedure. An ultrasound probe is attached to the endoscope. Although fine needle aspiration via endoscopic ultrasound is used commonly today in the diagnosis of pancreatic tumors, expanding the technique to other organs has only happened fairly recently. Based on proximity of the lesion to the gastrointestinal tract, endoscopic ultrasound can only visualize lesions in the left hepatic lobe, left kidney, and left adrenal gland. This technique is being performed only at certain centers across the country. In contrast to US-guided FNAs, endoscopic procedures are more invasive and time consuming and require deep sedation.
Biopsy Technique
The most important part of the procedure is the planning of the approach. Once the imaging modality has been chosen, the target visualized, the tract planned, and the patient is comfortable, the procedure may begin.
The area on the skin where the needle will enter is marked. The skin is cleaned with Betadine or more preferably with ChloraPrep® (2 % Chlorhexidine Gluconate/70 % Isopropyl Alcohol) because of its faster action and broader spectrum to fight bacteria. The site is covered with sterile drapes or towels to keep a sterile field. One percent buffered lidocaine is used for local anesthesia. A small wheal is made under the skin. Once the skin is numb, deeper anesthesia is applied under imaging guidance. The liver has a capsule with nerve endings that are irritated by the biopsy which, when breached by the needle, may cause the patient pain. It is the site of the deeper anesthesia for liver biopsies. For the kidney and adrenal gland, anesthesia is introduced to the level of the lesion and along its tract.
Once deeper anesthesia has been achieved, the biopsy portion may begin. If the biopsy is performed under CT guidance, an introducer is placed into the lesion for a coaxial approach. Similarly, a guide is placed on the ultrasound probe to direct the needle to the target. Once the lesion is reached, the stylette is removed and the needle is moved in a swift, repetitive, up and down motion in the lesion. This capillary action allows the cells to be drawn up into the needle. The needle is then removed from the target, and the cells are placed on the slide for pathology. Sometimes, and particularly in a very fibrous lesion, aspiration via an attached syringe is necessary to obtain sufficient material.
Typically core needle biopsies are requested at the time of the biopsy, and these can be performed using the same approach as the fine needle aspiration.
Needle Selection and Visualization
The most common needles used for fine needle aspiration are 22 gauge Chiba or spinal needles which come in a variety of lengths. Occasionally, 25 or 20 gauge needles can be used. In many cases a renal lesion, particularly one suspected of being a renal cell carcinoma, may yield only blood on fine needle aspiration with a 22 gauge needle. A smaller gauge may create fewer traumas and bleeding and yield more diagnostic material. Core biopsies are typically performed with larger gauge needles: 20, 18, or even 16 gauges.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







