Fig. 7.1
Open retropubic radical prostatectomy: Incision of the prostatic apex
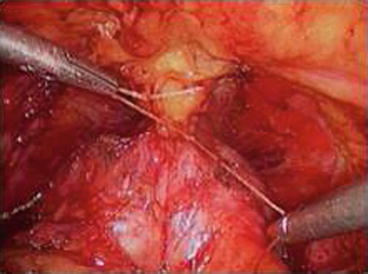
Fig. 7.2
Prostatic bed after removal of the prostate
7.3 Radical Prostatectomy: Oncological Results
Today there are several consolidated studies with longtime follow-up showing benefit for RP in terms of overall survival (OS) and cancer-specific survival (CSS), compared with conservative management (Table 7.1). Recently two large randomized trials comparing RP versus observation were published [7, 8]. In the Scandinavian prostate cancer group-4 randomized trial (SPCG-4) 665 patients were enrolled and randomized to surgery or watchful waiting: after 12 years of follow-up, 12.5 % of the surgery group and 17.9 % of the watchful waiting group had died of prostate cancer (difference = 5.4 %, 95 % confidence interval [CI] = 0.2–11.1 %), for a relative risk of 0.65 (95 % CI = 0.45–0.94; p = 0.03). At 12 years, 19.3 % of men in the surgery group and 26 % of men in the watchful waiting group had been diagnosed with distant metastases (difference = 6.7 %, 95 % CI = 0.2–13.2 %), for a relative risk of 0.65 (95 % CI = 0.47–0.88; p = 0.006). Likewise in the study of Prostate Cancer Intervention versus Observation Trial (PIVOT) [8] after a median follow-up of 10 years, 171 of 364 men (47.0 %) assigned to radical prostatectomy died, as compared with 183 of 367 (49.9 %) assigned to observation (hazard ratio, 0.88; 95 % confidence interval [CI], 0.71–1.08; p = 0.22; absolute risk reduction, 2.9 percentage points). Among men assigned to radical prostatectomy, 21 (5.8 %) died from prostate cancer or treatment, as compared with 31 men (8.4 %) assigned to observation (hazard ratio, 0.63; 95 % CI, 0.36–1.09; p = 0.09; absolute risk reduction, 2.6 percentage points). After a follow-up of 15 years, the SPCG-4 trial showed that RP was associated with a reduction of all-cause mortality: RR = 0.75 (0.61–0.92). Another interesting data emerges from SPCG-4 study [9]: After a follow-up of 15 years, the SPCG-4 trial showed that RP was associated with a reduction of all-cause mortality, and according to a post hoc statistical subgroup analysis, the number to treat to avert one death was 15 overall and 7 for men younger than 65 years of age. These data suggest that an age > or < of 65 years and favorable tumor characteristics (PSA < 10 ng/ml and Gleason score <7) could be useful parameters to guide physician in the choice between available treatments. With the intent of reducing the invasiveness of traditional open surgery and improving functional results, several urological centers have developed the technique of laparoscopic RP (LRP) [10]. More recently, Robotic systems have been introduced in an attempt to reduce the difficulty involved in performing complex laparoscopic urologic procedures [11]. The presence of three-dimensional (3D) magnification and tools that are able to duplicate hand movements with high accuracy has allowed many urologists to hypothesize that, despite the absence of tactile feedback, the application of robotic surgery to RP might yield real advantages, not only in terms of shorter learning curves but also in the ability to improve functional results without impairment of early oncologic outcomes. A recent systematic review including studies reporting oncological outcomes for LRP and RALRP had showed favorable results in terms of positive surgical margins rate (PSM): LRP and RALP were associated with PSM similar to those of open RRP [12].
Table 7.1
Studies reporting oncological results after radical prostatectomy for clinically localized prostate cancer
Study | No. of patients | % pT2 | % bDFS | % CSS | Surgical approach |
|---|---|---|---|---|---|
Bianco et al. (2005) [4] | 1,963 | 66 | 82 (5 years) | 99 | Open |
Han et al. (2001) [46] | 2,404 | 51 | 92 (5 years) | 99 | Open |
Eastham et al. (2008) [19] | 1,577 | 71 | 91 (5 years) | NA | Open |
Ploussard et al. (2010) [47] | 911 | 59 | 84 (2 years) | NA | LRP |
Rassweiler et al. (2006) [48] | 5,824 | 60 | 91 (5 years) | NA | LRP |
Hruza et al. (2012) [49] | 500 | 61 | 78 (5 years) | 98 | LRP |
Shikanov et al. (2009) [50] | 380 | 87 | 91 (2 years) | NA | RALP |
Patel et al. (2007) [51] | 500 | 78 | 95 (9.7 months) | NA | RALP |
7.4 Radical Prostatectomy in Locally Advanced Prostate Cancer
The incidence of locally advanced prostate cancer at the time of diagnosis has decreased because of the advent of serum PSA screening [13]. Despite this stage migration, a small percentage of patients continue to present with symptoms of clinical stage T3 disease (cT3). Although most patients undergo EBRT plus hormonal therapy, the optimum treatment for those patients is still under debate. Recent progress in surgical techniques has reduced the complication rates related to surgery, and oncological results in this set of patients are encouraging: cancer-specific survival curves at 5, 10, and 15 years that respectively range from 84 to 98 %, 84 to 91 %, and 76 to 84 % of patients, respectively. The overall survival rates at 5, 10, and 15 years range from 78 to 96 %, 63 to 77 %, and ≥50 % of patients, respectively. The biochemical-free survival rate (PSA < 0.2 ng/ml) at 5, 10, and 15 years ranges from 45 to 62 %, 43 to 51 %, and 15 to 49 %, respectively. These results are better than the results obtained with isolated EBRT and are of the same order as results reported after EBRT combined with hormonal therapy [14, 15]. RP is a reasonable first step in selected patients with very-high-risk PC and low tumor volume. Management decisions should be made after all treatments have been discussed by a MDT (including urologists, radiation oncologists, medical oncologists, and radiologists), and after the balance of benefits and side effects of each therapy modality has been considered by the patients with regard to their own individual circumstances. The problem remains the selection of patients before surgery. Actually the diagnosis of cT3 diseases is mainly based on digital rectal examination and PSA values [16]; however, Nomograms, including PSA level, stage, and Gleason score as well as new imaging tool as a PET-TC for lynphonode involvement or mMRI for local staging, can be useful in predicting the pathological stage of disease [17, 18].
7.5 Radical Prostatectomy: Complications
7.5.1 Erectile Dysfunction
Given that RP is a curative treatment for early prostate cancer with a proven long-term survival benefit [8], optimal outcomes of RP are not limited to cancer control, but also include urinary continence and preservation of erectile function (EF) [19]. Preservation of EF has become a goal in prostate cancer surgery with advances in our understanding of the prostate and cavernous nerve anatomy and with the introduction of nerve-sparing RP by Walsh (NSRP) [3] (Fig. 7.3). Recovery of EF after treatment for PC has become a main goal over oncological results even more in recent years where the diagnosis is made in younger patients and where different treatments with comparable oncological outcomes are now available. The introduction of NSRP technique has significantly improved the functional results in terms of recovery of sexual function [20] and several studies comparing open RP versus LRP and RALRP have demonstrated a significant advantage for robotic and laparoscopic techniques in terms of recovery of erectile function with a more evident advantage for RALRP [21, 22]. Given that NS technique and the number of neuro-vascular bundles (NVB) preserved are best predictor of recovery EF after RP, there are several preoperative factors that should be considered when physician with the patient faces the problem of what we can expect from surgery over oncological results. A recent systematic review of prognostic indicators for successful sexual outcome showed that the most important preoperative prognostic factors for the return of potency after surgery are the age of the patient and sexual function before the operation: potency rates vary between 61 and 100 %, postoperatively. For men between 50 and 70 years of age the overall potency rate declined to 70–85 %. After unilateral and bilateral nerve-sparing procedures potency is found in 47–58 % and 44–90 %, respectively. Men older than 70 years have low potency rates ranging from 0 and 51 %, despite nerve-sparing procedures [23]. Based on these results we can assume that Recovery of sexual potency has become a realistic option for relatively young patients suffering from an organ-confined prostatic carcinoma who used to have a normal sexual function before the operation (Table 7.2).
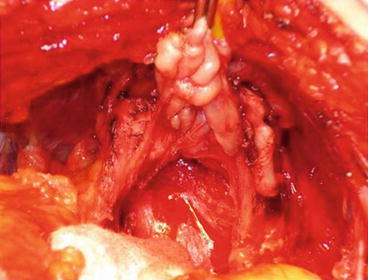
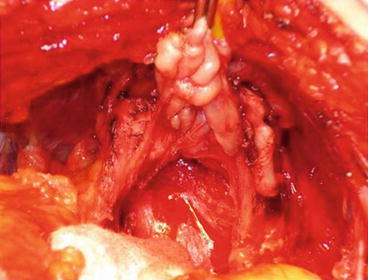
Fig. 7.3
Bilateral neuro-vascular bundles preservation after open radical retropubic prostatectomy
Table 7.2
Studies reporting erectile function recovery after nerve sparing radical prostatectomy for clinically localized prostate cancer
Study | No. of patients | Potency definition | Potency recovery % (Mo) | Surgical approach |
|---|---|---|---|---|
Kundu et al. (2004) [52] | 1,834 | ESI | 78 (18) | Open |
Noldus et al. (2002) [53] | 68 | ESI | 35 (12) | Open |
Rogers et al. (2006) [54] | 127 | ESI | 41 (12) | LRP |
Hoznek et al. (2001) [55] | 134 | ESI | 56 (12) | LRP |
Goeman et al. (2006) [56] | 550 | ESI | 42 (12) | LRP |
Curto et al. (2006) [57] | 677 | ESI | 58 (12) | LRP |
Menon et al. (2007) [58] | 2,652 | ESI | 70 (12) | RALP |
Joseph et al. (2006) [59] | 325 | ESI | 80 (12) | RALP |
Patel et al. (2007) [51] | 500 | ESI | 78 (12) | RALP |
7.6 Which Therapy for Which Patient: The Point of View of the Urologist
When evaluating a patient with early-stage prostate cancer, the decision regarding the “optimal” management strategy is complex. It is increasingly apparent that with the advent of PSA screening, stage migration has resulted in the diagnosis of many men with potentially clinically insignificant disease [24]. To date there are no studies that have clearly demonstrated any survival advantage for surgical intervention over nonsurgical therapies among patients with favorable-risk prostate cancer. Overall, excellent biochemical and survival outcomes can be achieved with any of the commonly used interventions including RP and EBRT. On the basis of these considerations, it is important to consider the different side-effect profiles relevant for each treatment modality and what we can aspect from surgery in terms of functional results and related quality of life. Today, the best candidates for RP are those patients with clinically organ-confined disease with comorbidities that allow a safe surgical procedure. From an oncological point of view, young patients (<65 years) can expect a significant advantage from surgery in terms of disease-free survival free (DFS) and it should be considered in a decision-making process even more in an MDT where urologist, radiotherapist and oncologists discuss each case suitable for treatment with curative intent. From the point of view of quality of life, to obtain best results from RRP in terms of recovery of erectile function, the best candidate to surgery seems to be a young man with clinically localized disease, with good preoperative erectile function and without comorbidities such hypertension or diabetes.
7.6.1 Radiation Therapy
Primary local management of prostate cancer remains controversial due to the various treatment possibilities available. Traditionally, the primary treatment modalities for patients with clinically localized prostate cancer have included surgical therapy and radiation therapy (RT). Nowadays, it is important to realize the necessity of an MDT for patients with low- (cT1-2a disease, Gleason score ≤ 6 and PSA < 10 ng/ml), intermediate- (cT2b-c and/or Gleason score 7 and/or PSA 1,020 ng/ml), or high-risk (cT3a and/or Gleason score > 7 or PSA > 20 ng/ml). Whereas radiation therapy is recommended as primary treatment modality in locally advanced prostate cancer, because it is improbable to completely excise the tumor by surgery [25], there is no a clear indication for primary treatment in clinically localized disease. There are no modern conclusive randomized clinical trials that compare surgical and radiotherapeutic treatments, and, consequently, there are no data showing superiority of one treatment approach over other [26]. Therefore, the MDT has become a must on the management decision to establish a personal patient’s best care therapy. During the decision-making process, patients should be actively involved in the choice of treatment and must be informed of the benefit and risks in quality of life and sexual function of each option, to balanced information [27].
This chapter provides highlights of the curative treatment options, both surgical approach or radiotherapy management. We review the various form of radiation therapy—three-dimensional conformal radiation therapy (3D-CRT), intensity-modulated radiation therapy (IMRT), image-guide radiation therapy (IGRT), brachytherapy, proton therapy—and its outcomes. Regardless of RT form or technique, definitive RT represents a valid treatment option in all patients with localized prostate cancer and it is recommended in locally advanced disease.
7.6.2 Radiation Therapy
Radiation therapy (RT) is continuing to evolve in recent era. Nowadays, the radiotherapy state of the art guarantees different radiotherapeutic approach available to the management of prostate cancer. Over the past 20 years, EBRT has gradually developed and has been replaced by more sophisticated forms of EBRT, such as IMRT, IGRT and proton therapy. These advances in therapeutic methods have turned into a better clinical outcome. Randomized trials have demonstrated that an increase in radiation total dose can safely be achieved without an increase in serious acute or late morbidity, when a highly conformal radiation technique—included three-dimensional photon and proton beams—is used [28, 29]. The significant improvement in radiation therapy techniques has entailed a rise in the cost and in the treatment time. To reduce cost and to increase therapeutic benefit, hypofractionated regime (higher dose per fraction with a shortened overall treatment time) has been suggested as solution, based on the presumed low α/β ratio of prostate cancer compared with surrounding normal tissue [30]. But the real effectiveness of this approach is still uncertain. Likewise, brachytherapy (permanent interstitial implantation, low-dose rate, or high-dose rate) has significantly developed in techniques, optimization, and dose distributions, becoming a valid alternative treatment in early prostate cancer and a co-adjuvant option in selected advanced stage.
7.7 External Beam Radiation Therapy
EBRT represents a well-established primary treatment options for clinically localized prostate cancer, considering that both modern RT and surgery resulted in equal cancer control.
In the last several decades, 3D-CRT has successfully replaced two-dimensional planning treatment, due to significant reduction in grade 3 or greater acute and late toxicity, and implementation of radiation total dose over 70 Gy [31]. Nowadays, the increasing availability of highly conformal irradiation techniques and advances in imaging technology, particularly RMN, are similarly affording new opportunities to optimize RT and diminish toxicity. The primary goal is to increase the dose gradient between target volume and surrounding areas, providing adequate coverage of the prostate and dose restriction to bladder and rectum. With the advent of IMRT, dose conformation and dose escalation have become possible. Of sure, benefit from IMRT requires meticulous delineation of target volume and organs at risk, accurate quality control in radiation planning and delivery, and limiting of interfraction and intrafraction variability—variability that can be reduce and minimize by daily prostate localization using IGRT [32].
EBRT Results
The role of radiation dose escalation is essential in tumor control, as supported by the growing evidence from clinical trials. Kuban et al. [29] randomized 301 patients with stage T1b to T3 prostate cancer to either 70 Gy or 78 Gy. The modest escalation dose improved freedom from biochemical and clinical progression (78 % vs. 59 %, p = 0.004), with the largest benefit in prostate cancer patients with PSA >10 ng/ml (78 % vs. 39 %, p = 0.001). In the Dutch trial [33] patients were randomly assigned to receive 68 Gy or 78 Gy and results showed better outcome in 78 Gy arm (54 % vs. 47 %, p = 0.04). In the MRC trial [34] patients were randomized to 64 Gy or 74 Gy and benefited from dose escalation (HR 0.67, 95 % CI 0.53–0.85, p = 0.0007) (Table 7.3
Table 7.3
Studies reporting oncological results after external beam radiation therapy (EBRT) for clinically localized prostate cancer
Study
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
|---|




