How Should Changes in Plasma Creatinine Be Interpreted?
Renal (glomerular) function is best determined by measuring the glomerular filtration rate (GFR). The most common methods utilize the endogenous substance creatinine, which is formed by the metabolism of creatine in skeletal muscle and excreted by glomerular filtration (although it is not a perfect marker of GFR, as there is also some tubular secretion). The plasma (or serum) creatinine concentration will reflect both the production rate of creatinine (which is proportional to muscle mass) and the excretion rate of creatinine (which depends on renal function). In the steady state, production will equal excretion, and plasma creatinine will be stable when repeatedly measured. Determination of GFR by creatinine clearance is discussed later in this chapter. Most of the time, clearance methods are not needed in clinical practice, and GFR is estimated from the plasma creatinine concentration using various formulae, as will also be discussed later in this chapter.
CHRONIC RENAL FAILURE (CHRONIC KIDNEY DISEASE)
By definition, a patient with chronic kidney disease (CKD) has had kidney disease for months to years (at least 3 months by standard definitions) (Table 2.1). GFR may or may not be impaired. By current convention, if estimated GFR (eGFR) is moderately impaired (30-59 mL/min/1.73 m2), this is termed stage 3 CKD, whereas more severe impairment (15-29 mL/min/1.73 m2) and very severe impairment (<15 mL/min/1.73 m2) are termed stage 4 CKD and stage 5 CKD, respectively. As GFR decreases, plasma creatinine will progressively rise, generally over months to years. The change in plasma creatinine is very slow, and thus the concentration
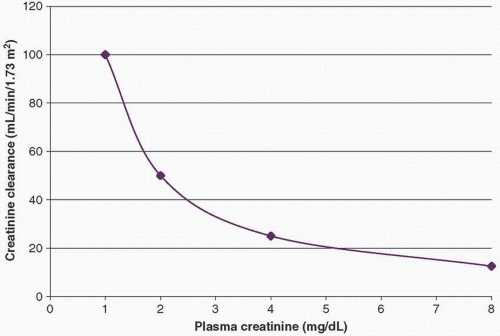
will be stable if measured daily. (If it rises every day, this is acute or acute-on-chronic renal failure.) This is because, in CKD with diminished GFR, production still equals excretion of creatinine, though at an increased plasma creatinine level. As CKD progresses, there will be an exponential increase in plasma creatinine as renal function declines. This is shown in Figure 2.1. The reason for the exponential increase merits further discussion.
will be stable if measured daily. (If it rises every day, this is acute or acute-on-chronic renal failure.) This is because, in CKD with diminished GFR, production still equals excretion of creatinine, though at an increased plasma creatinine level. As CKD progresses, there will be an exponential increase in plasma creatinine as renal function declines. This is shown in Figure 2.1. The reason for the exponential increase merits further discussion.
TABLE 2.1 Chronic Kidney Disease versus Acute Kidney Disease | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Determination of GFR in CKD by Creatinine-Based Methods
Measured Creatinine Clearance
When a substance is cleared from the blood by glomerular filtration, the excretion rate of the substance (assuming no secretion or reabsorption by the tubules) will equal the volume of plasma that is totally cleared of the substance. Therefore,
Plasma concentration × Clearance = Urine concentration × Urinary flow rate, or
Clearance = (Urine concentration × Urinary flow rate)/Plasma concentration [(UV/P)]
For example, if a patient excretes 1,440 mg of creatinine in 24 hours (1 mg/min) and the plasma concentration is 1 mg/dL (0.01 mg/mL), the creatinine clearance = 1 mg/min/0.01 mg/mL = 100 mL/min.
Creatinine-Based Formulae
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree