Liver has three functional components: hepatocytes, central veins/sinusoids, portal tracts (triads)
Basic architecture: cords of hepatocytes (one cell thick), separated by vascular sinusoids
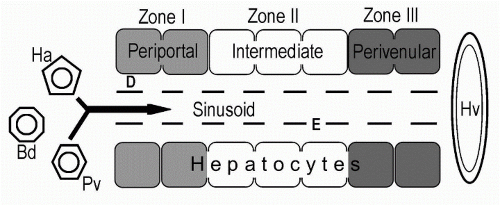
The sinusoids are lined with endothelial cells (E) and Kupffer cells (which have Mφ capabilities)
Central veins (aka, terminal hepatic venules, Hv) collect blood after it percolates through sinusoids and carry it back to larger hepatic veins (Hv)
Distributed at regular intervals are portal tracts (bile ducts-Bd, hepatic arteries-Ha, portal veins-Pv) The row of hepatocytes immediately adjacent to portal tract is termed ‘limiting plate’
Modified with permission from McNally P. GI/Liver Secrets. 3rd ed. New York: Elsevier/Mosby, 2006:237.
Functional unit of the liver is represented by Hepatic Acini: 3D units built around a central axis containing a portal tract and its blood vessels
From the portal area, plates of hepatocytes radiate outward toward central veins, located at the periphery of the acinus
The acinus is divided into three zones: 1 is closest to portal tracts, 3 is closest to the central vein; Zone 1 is best supplied by oxygen and nutrients
Bridging fibrosis: portal tracts & central veins connected by scar tissue
Cirrhosis: diffuse scarring altering the architecture into nodules of hepatocytes (must be diffuse by definition, not just focal nodular formation)
Micronodular: nodules ≤3 mm, most common with alcohol
Macronodular: nodules >3 mm, most common with viral hepatitis
▪
Types of liver cell injury:
Causes:
Fatty change (Steatosis)
Ethanol, Obesity, Diabetes, Drugs
Councilman bodies (Acidophilic bodies)
Viral hepatitis, Drugs, Nonspecific reactions; Represents apoptosis
Mallory Hyaline
Ethanol, Obesity, Diabetes, Drugs, Wilson’s, Biliary tract disease, Hepatocellular carcinoma
Hydropic change (Ballooning)
Viral hepatitis, Drugs, Cholestasis
Cholestasis
Duct obstruction or injury, Drugs, Viral hepatitis
Interlobular duct injury
Piecemeal necrosis
Viral hepatitis, PBC, Drugs, Wilson’s disease
Increased iron stores
Hemochromatosis, Transfusions, Hemolysis
Granulomas
Tuberculosis, Sarcoid, Fungi, Drugs (complete list below); I.e. think infection, drug, sarcoid
“Reverse cirrhosis”
Central vein to central vein (not portal triad to portal triad), seen with cirrhosis 2° to Heart Failure
See also Liver- Drug Induced Liver Disease (Chapter 4.11)
Alcohol Liver Disease can result in fatty liver, alcoholic hepatitis and alcoholic cirrhosis
Hepatocytes contain globules of fat, usually larger than & compressing the hepatocyte nucleus (referred to as Macrovesicular steatosis)
Initially the change is around the central veins, but may extend to involve the entire acinus
Biopsies of alcoholic hepatitis may show hepatocytes that are swollen with areas of necrosis, associated with inflammation (PMNs)
Hepatocytes may also contain Mallory hyaline: (also found in other causes of liver injury, as noted above)
Irregular ropelike strings of eosinophilic material in cytoplasm representing aggregates of microfilament cytokeratin
Although fat and neutrophils can resolve relatively quickly after alcohol abstinence, hyaline can take up to 6 weeks to disappear
Progression: initial scarring around central veins with spider web-like fibrosis long sinusoids; eventually bridging fibrosis connects central veins and portal tracts and adjacent portal tracts; When cirrhosis fully develops, most of the native central veins are obliterated
Alcoholic cirrhosis is Micronodular because scarring is relatively uniform throughout liver
If you get a biopsy report that says: ‘alcoholic hepatitis’: Caution! Better term is steatohepatitis, over 20 conditions can show hyaline with fatty change:
Obesity, Diabetes, Drugs/Vit A toxicity, Wilson’s, Prolonged cholestasis (PBC), Jejunal-ileal bypass/gastric stapling
Non-Alcoholic fatty liver disease (NAFLD) See also Liver- NAFLD (Chapter 4.22)
Microvesicular steatosis: AFLP, Meds (valproic acid, tetracycline), Reye’s syndrome, Jamaican vomiting sickness, Mitochondrial disorders
Those with viral hepatitis, a biopsy can help assess amount of inflammation (grade), degree of irreversible fibrosis/cirrhosis (stage) and chronicity
HAV: rarely need biopsy 2° rarely causing chronic liver disease; may help distinguish severe cholestasis in HAV from large duct obstruction
Acute hepatitis has predominantly parenchymal inflammation
HBV/HCV: can cause chronic liver disease ± acute/fulminant disease; the histological features can help determine both treatment and prognosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




