Each histologic type of renal cell carcinoma (RCC) has different pathologic and clinical parameters; however, the independent role of histologic type in outcome prediction remains contested. Most studies show relevance for outcome of each histologic type when correlated with survival by univariate analysis, whereas few studies show differences in outcome once other key prognostic factors, such as stage and grade, are considered. These studies highlight the challenges to prove outcome relevance. Despite the contested independent value of type for outcome prediction, separation of RCC into types is well accepted and can be substantiated on clinical, pathologic, molecular, and general outcome differences.
Each type of renal cell carcinoma (RCC) shows differences in pathologic and clinical parameters, including prognostic relevance; however, the outcome prediction for each type remains controversial. In general, chromophobe and papillary RCC have been associated with more favorable outcomes than clear cell RCC, whereas those of collecting duct and unclassified types have been less favorable. Large series examining outcomes have shown prognostic significance of histologic types by univariate analysis; however, only a few series retain prognostic significance on multivariate analysis. The studies in which histologic type retains prognostic significance are single-institution studies with standardized assignment of histologic type. In contrast, multi-institutional studies or pooled data sets do not show independent prognostic significance of histologic type nor do smaller series from single institutions in which statistical strength is underpowered. Data on outcomes are more recently determined through evaluation of histologic types separately against matched clear cell types or accrued through pooled data sets. This article summarizes the outcomes data for chromophobe, papillary, collecting duct, and unclassified RCC, and also reviews the impact of histologic type on patients with metastatic RCC. As greater knowledge on RCC is gained, newer entities are emerging that may shift distribution of cases. Despite the contested role of histologic type as an independent predictor of outcome, separation of RCC into types is now well accepted and substantiated in clinical, biologic, molecular, and sometimes also in outcome differences.
Renal cell carcinoma classification and other prognostic factors
The current 2004 World Health Organization (WHO) classification of renal cell carcinoma (RCC) follows on the earlier Heidelberg and Rochester classifications, which in turn represent expansions of the Mainz classification. The current classification recognizes the heterogeneity of RCC and describes distinct types of RCC with unique morphologic and genetic characteristics. The major histologic variants of RCC are clear cell, papillary, chromophobe, and collecting duct, and account for 90% to 95% of RCCs ( Table 1 ). The classification also includes the less commonly encountered types of renal medullary carcinoma, Xp11 translocation carcinoma, carcinoma associated with neuroblastoma, and mucinous, tubular, and spindle cell carcinomas. An important category included within the classification is the unclassified type, which is assigned when a tumor does not readily fit into any other group.
| RCC Subtype | Proportion (%) | Outcome vs Clear Cell RCC |
|---|---|---|
| Clear cell RCC | 80 | — |
| Papillary RCC | 10 | Favorable |
| Chromophobe RCC | 5 | Favorable |
| Collecting duct | 1 | Unfavorable |
| RCC, unclassified | 4–6 | Unfavorable |
| Multilocular clear cell RCC | Exact proportion undetermined but rare tumors likely to account for <2% of tumors overall | Low malignant potential |
| Renal medullary carcinoma | Highly aggressive | |
| Xp11 translocation carcinoma | Undetermined | |
| Carcinoma associated with neuroblastoma | Similar to clear cell RCC | |
| Mucinous tubular and spindle cell carcinoma | Favorable with exception |
In determining the prognostic strength of this classification system, one should recognize that it is already in its eighth year since publication and likely to be updated in the near future to incorporate additional emerging entities within the classification of RCC ( Table 2 ). The impact of newer types on the overall proportion of cases within each type is uncertain, although it may be low because of the rarity of these emerging entities.
| RCC Subtype | Prevalence | Outcome Relevance |
|---|---|---|
| Tubulocystic carcinoma | Rare | Not fully determined |
| Thyroid-like (follicular) renal carcinoma | Rare | Not fully determined |
| Acquired cystic disease-associated RCC/carcinoma associated with end-stage renal disease | Rare | Not fully determined |
| Clear cell papillary RCC | Rare | Not fully determined |
| Oncocytic papillary RCC | Rare | Not fully determined |
| Leiomyomatous RCC | Rare | Not fully determined |
In evaluating studies on outcome, one should realize that the overwhelming group, clear cell RCC, is likely to disproportionately outweigh all other groups in studies subject to statistical analysis. Furthermore, a comparison of other newly introduced and rarely encountered types within the classification is limited by insufficient accumulated data and the small number of cases in each type. Inferences on the behavior of these newer types are insufficient for conclusive determination as are based on case reports or small series data.
The prognostic utility of histologic type as an independent prognostic factor remains debated, with some convinced of its value and others not. The current American Joint Committee on Cancer (AJCC) Staging Manual (7th edition), used routinely to characterize tumors, recommends the use of the WHO 2004 classification, stating that “the more common histopathologic types have distinct molecular characteristics and are associated with prognostic or predictive significance as reflected by their integration in predictive algorithms for RCC.” This statement about the prognostic impact of histopathologic type reflects a view that may not be widely accepted. This article further evaluates this issue.
To understand the role of histopathologic subtype, one must be aware of its value in the context of other recognized prognostic factors in RCC. Prognostic factors may be subdivided into (1) anatomic (TNM stage, tumor size), (2) histopathologic (nuclear grade and histologic subtype), and (3) clinical (symptoms and performance status; laboratory results). Of these factors, pathologic stage and nuclear grade represent the major prognostic variables used routinely in localized RCC. Increasingly, other prognostic variables have been added to stage and grade to improve predictive strength.
The role of stage as defined in the TNM classification is widely accepted and has been well validated as a key prognostic parameter in RCC. With higher stage, including lymph node invasion and metastasis to other organs, patients have a progressively worse prognosis and shorter survival. The TNM system which defines stage is progressively modified to incorporate new evidence and is most recently revised in the AJCC 7th edition, released in 2010. The TNM classification denotes that risk of malignancy increases with size. Frank and colleagues have validated this showing that for each 1-cm increase, the likelihood of malignancy and high grade features in renal tumors increases. More recently, size has been shown to correspond with higher grade, with a 0% incidence of high-grade features in tumors smaller than 1 cm, increasing to a 59% incidence in tumors larger than 7 cm.
Nuclear grade as described in the Fuhrman system is the most commonly used grading scheme for RCC, and has been shown in multiple prior studies to correlate with tumor size, stage, and metastasis in clear cell type RCC. Its role in papillary and chromophobe RCC is not widely accepted and has been questioned. Recently, newer nuclear grading schemes for chromophobe and papillary RCC have been proposed and await validation.
Other histologic features include coagulative tumor necrosis and sarcomatoid transformation, which have been proven to be independent predictors of adverse outcome in clear cell RCC. Sarcomatoid transformation, once considered a distinct subtype, is now recognized as a high-grade dedifferentiation that may occur in any subtype of RCC. It is characterized by spindle cell morphology, often with marked nuclear pleomorphism, and occurs in a minority (<5%) of all RCC. It is associated with higher stage and worse prognosis, resulting in a 5-year disease-specific survival of 22% compared with 79% in tumors without sarcomatoid transformation.
Histologic type of RCC: morphologic, clinical, and molecular features of each type
Clear Cell RCC
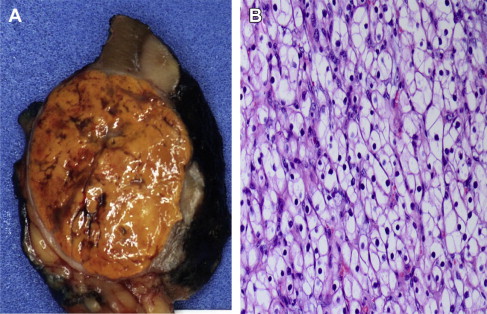
Clear cell RCC is defined (WHO 2004) as a malignant renal neoplasm composed of cells with a clear or eosinophilic cytoplasm within a delicate vascular network. The typical tumor is solid with a golden yellow appearance ( Fig. 1 ), and microscopically shows neoplastic cells that may be clear or eosinophilic when higher grade. Approximately one-third of all patients have metastatic disease at initial presentation, and 20% to 40% experience local recurrence or distant metastasis after nephrectomy. The molecular/genetic clear cell RCC pathogenesis is based on two key molecular pathways: the hypoxia-inducible pathway associated with mutation of the Von Hippel-Lindau (VHL) tumor suppressor gene, and the mammalian target of rapamycin (mTOR) signaling pathway.
Papillary RCC
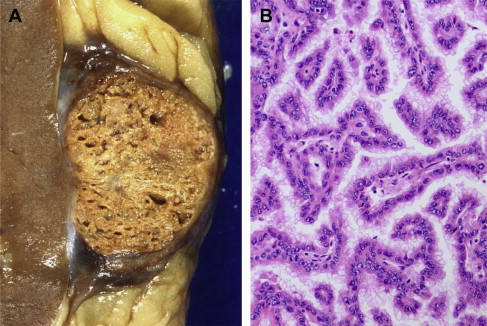
Papillary RCC accounts for approximately 10% of all RCC and nearly 29% of RCC in African Americans. On macroscopic examination, these tumors are well circumscribed, often with a fibrous pseudocapsule, and have a variegated appearance ranging from streaked dull yellow to uniformly dark brown ( Fig. 2 ). Microscopically, the tumors show papillary or tubular architecture and occasionally may be solid. In the WHO classification, two types of papillary RCC are described: type 1, in which the neoplastic cells lining the cores are small with scant cytoplasm, and type 2, in which the cells are of higher nuclear grade with prominent nucleoli and have eosinophilic cytoplasm. The molecular pathway, different from that of clear cell type, also differs between types 1 and 2. In type 1, mutations of the MET oncogene (on chromosome 7) result in activation of the intracytoplasmic tyrosine kinase domains, which activate the hepatocyte growth factor pathway. The molecular pathway of type 2 is still to be fully elucidated but is suggested to be similar to that of the familial syndrome of hereditary leiomyomatosis and renal cell carcinoma, with a mutation in the fumarate hydratase gene (on chromosome 1). This results in upregulation of hypoxia-inducible factors (proangiogenic and growth factors).
Chromophobe RCC
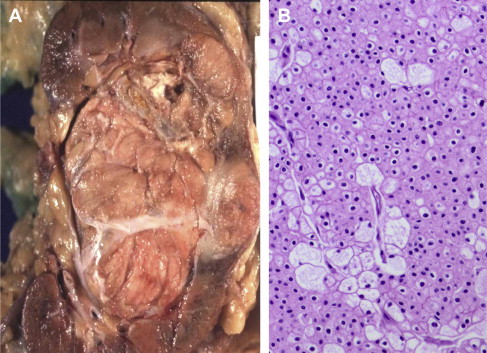
Chromophobe RCC accounts for approximately 5% of surgically removed renal epithelial tumors, and typically has a pale tan appearance ( Fig. 3 ). Thoenes and colleagues first described this entity in 1985, showing a 4.6% incidence in a series of 697 RCC cases. Microscopically, it is characterized by a solid pattern of large polygonal cells with transparent reticulated cytoplasm, prominent cell membranes, wrinkled nuclei, and perinuclear halos. In the series to date, most tumors have been confined to the kidney; however, a small number (<5%) may present with metastasis or show sarcomatoid transformation. Insight on the molecular pathway driving these tumors is suggested from study of the Birt-Hogg-Dube syndrome, a hereditary form of this tumor in which there are frequently multifocal and bilateral tumors. The Birt-Hogg-Dube gene (on chromosome 17) produces a protein folliculin, which functions as a tumor suppressor and may activate the mTOR pathway.
Collecting Duct Carcinoma
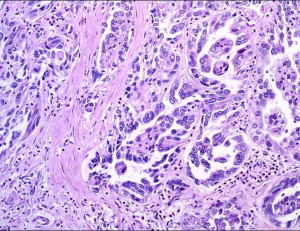
Collecting duct carcinoma is a rare subtype of RCC, accounting for less than 2% of RCC (range, 0.4%–1.8%). Based on limited earlier evidence in the literature (case reports and small case series), these tumors are recognized to be highly aggressive, often presenting at advanced stage and resulting in a poor prognosis. They have been described as occurring in a wide patient age range, with a male predominance of approximately 2:1. These tumors are usually large when diagnosed and have a firm white to gray appearance, with irregular borders and areas of necrosis. The histologic features show an infiltrative tubular or tubulopapillary pattern, associated with a desmoplastic stromal reaction, and frequent high nuclear grade ( Fig. 4 ). The molecular pathway underlying CDC is poorly understood. Cytogenetic abnormailities include monosomy of chromosomes 1, 6, 14, 15 and 22 with allelic loss on chromosomal arms 1q, 6p, 8p, 13q, and 21q. A minimal deletion located at 1q32.1–32.2 was mapped in up to two thirds of CDC suggesting a tumor suppressor gene in this region.
Unclassified RCC Category
The unclassified RCC category is a diagnostic category, not a specific type, and is used to assign RCCs that do not fit into the other RCC types based on histologic evaluation. It is recognized to be a heterogeneous group that therefore cannot be defined in a limited manner. Features that may cause a carcinoma to be placed in this category include a composite of other RCC subtypes, sarcomatoid morphology without recognizable epithelial elements, mucin production, mixtures of epithelial and stromal elements, and unrecognizable cell types. The assignment to this category varies from 0.7% to 5.7% in published series, reflecting varied criteria. Differences in outcome across series may be partly attributed to the definition used for unclassified RCC.
Histologic type of RCC: morphologic, clinical, and molecular features of each type
Clear Cell RCC
Clear cell RCC is defined (WHO 2004) as a malignant renal neoplasm composed of cells with a clear or eosinophilic cytoplasm within a delicate vascular network. The typical tumor is solid with a golden yellow appearance ( Fig. 1 ), and microscopically shows neoplastic cells that may be clear or eosinophilic when higher grade. Approximately one-third of all patients have metastatic disease at initial presentation, and 20% to 40% experience local recurrence or distant metastasis after nephrectomy. The molecular/genetic clear cell RCC pathogenesis is based on two key molecular pathways: the hypoxia-inducible pathway associated with mutation of the Von Hippel-Lindau (VHL) tumor suppressor gene, and the mammalian target of rapamycin (mTOR) signaling pathway.
Papillary RCC
Papillary RCC accounts for approximately 10% of all RCC and nearly 29% of RCC in African Americans. On macroscopic examination, these tumors are well circumscribed, often with a fibrous pseudocapsule, and have a variegated appearance ranging from streaked dull yellow to uniformly dark brown ( Fig. 2 ). Microscopically, the tumors show papillary or tubular architecture and occasionally may be solid. In the WHO classification, two types of papillary RCC are described: type 1, in which the neoplastic cells lining the cores are small with scant cytoplasm, and type 2, in which the cells are of higher nuclear grade with prominent nucleoli and have eosinophilic cytoplasm. The molecular pathway, different from that of clear cell type, also differs between types 1 and 2. In type 1, mutations of the MET oncogene (on chromosome 7) result in activation of the intracytoplasmic tyrosine kinase domains, which activate the hepatocyte growth factor pathway. The molecular pathway of type 2 is still to be fully elucidated but is suggested to be similar to that of the familial syndrome of hereditary leiomyomatosis and renal cell carcinoma, with a mutation in the fumarate hydratase gene (on chromosome 1). This results in upregulation of hypoxia-inducible factors (proangiogenic and growth factors).
Chromophobe RCC
Chromophobe RCC accounts for approximately 5% of surgically removed renal epithelial tumors, and typically has a pale tan appearance ( Fig. 3 ). Thoenes and colleagues first described this entity in 1985, showing a 4.6% incidence in a series of 697 RCC cases. Microscopically, it is characterized by a solid pattern of large polygonal cells with transparent reticulated cytoplasm, prominent cell membranes, wrinkled nuclei, and perinuclear halos. In the series to date, most tumors have been confined to the kidney; however, a small number (<5%) may present with metastasis or show sarcomatoid transformation. Insight on the molecular pathway driving these tumors is suggested from study of the Birt-Hogg-Dube syndrome, a hereditary form of this tumor in which there are frequently multifocal and bilateral tumors. The Birt-Hogg-Dube gene (on chromosome 17) produces a protein folliculin, which functions as a tumor suppressor and may activate the mTOR pathway.
Collecting Duct Carcinoma
Collecting duct carcinoma is a rare subtype of RCC, accounting for less than 2% of RCC (range, 0.4%–1.8%). Based on limited earlier evidence in the literature (case reports and small case series), these tumors are recognized to be highly aggressive, often presenting at advanced stage and resulting in a poor prognosis. They have been described as occurring in a wide patient age range, with a male predominance of approximately 2:1. These tumors are usually large when diagnosed and have a firm white to gray appearance, with irregular borders and areas of necrosis. The histologic features show an infiltrative tubular or tubulopapillary pattern, associated with a desmoplastic stromal reaction, and frequent high nuclear grade ( Fig. 4 ). The molecular pathway underlying CDC is poorly understood. Cytogenetic abnormailities include monosomy of chromosomes 1, 6, 14, 15 and 22 with allelic loss on chromosomal arms 1q, 6p, 8p, 13q, and 21q. A minimal deletion located at 1q32.1–32.2 was mapped in up to two thirds of CDC suggesting a tumor suppressor gene in this region.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






