Hepatobiliary Cystic Disease
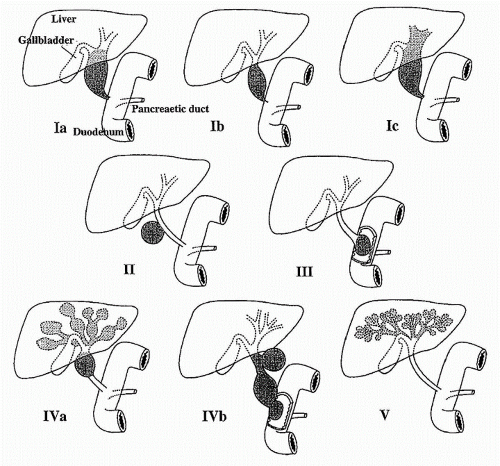
BILE DUCT CYSTS: major classes and subtypes
Ia: choledochal cyst
Ib: segmental choledochal dilation
Ic: diffuse or cylindrical duct dilation
II: extrahepatic duct diverticula
III: choledochocele
IVa: multiple intra- and extrahepatic duct cysts
IVb: multiple extrahepatic duct cysts
V: intrahepatic duct cysts
 Reprinted with permission from McNally P. GI/Liver Secrets. 3rd ed. New York: Elsevier/Mosby, 2006:310. |
Female predominance
Most bile duct cysts are diagnosed in childhood via U/S; Incidence of cancer with bile duct cysts is 2-15% (i.e. not a benign process!)
Triad of abdominal pain, jaundice, and abdominal mass; Typically, only one or two present at any one time; Fever is common
Cholangiopancreatography: percutaneously, endoscopically, interoperatively: critical for planning excision
Caution with Caroli’s due to increased risk of recurrent cholangitis and sepsis
MRCP may be the preferred imaging modality, but most found via U/S
Preferred treatment is complete surgical resection of the cyst, rather than internal drainage
Complications 8%: stricture, recurrent jaundice, cholangitis; Corresponding complications with internal drainage: 50%
Risk of bile duct cancer is reduced, but not eliminated with surgery (i.e. can develop in other parts of biliary tree)
Recurrent symptoms may be candidates for transplant if no evidence of cholangiocarcinoma
CAROLI’S: congenital dilations of intrahepatic bile ducts; Usually symptomatic as children with abdominal pain and HSM
Caroli’s Disease: have cystic dilations limited to the larger intrahepatic bile ducts, predisposing to recurrent calculi and cholangitis
Caroli’s Syndrome: cystic dilations along portal tract, believed to result from a ductal plate malformation that affects bile ducts at all levels
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




