A hepatotrophic virus; the liver is the primary site of infection, replication and cellular damage
Chronic hepatitis: presence of clinical, biochemical, and serologic abnormalities for up to 6 months
350 million cases worldwide; 1.25 million in US; most cases in Asia and Africa; causes 30% of acute and 15% of chronic hepatitis in the US
10th leading cause of death in the world, 5th leading infectious disease cause of death in the world
Chronicity of HBV acquired during infancy: 90%; acquired during adulthood: 5%
In general, when a patient gets acute HBV: 95% recovery, 5% chronically infected, Fulminant hepatic failure (very rare)
Transmission: sexual (most common), percutaneous, perinatal
Household/intimate contacts need to be vaccinated since they are at most risk
Incubation: 1-6 months
Pregnant women/Vertical Transmission/Breastfeeding: Lamivudine for treatment; prophylaxis is available; See also Liver- Pregnancy Pearls (Chapter 4.25)
Hep B: Transmission 1st Trimester (10%), 3rd Trimester (90%); All women tested in 3rd trimester
Virus: DNA, circular gene shape, envelope, 42 nm in size; Replicates at 1011 virions/day
8 genotypes identified: A-H; The future may tell us that certain genotypes are better treated with either Nucleosides analogues or PEG-INF
Spilled blood contaminated with HBV can be infectious for up to one week (i.e. DNA viruses resist degradation)
Natural History: anorexia, nausea, vomiting, fatigue, abdominal pain, mild fever, jaundice, dark urine, light colored stools
Acute: 70% subclinical, 30% jaundice, <1% fulminant hepatitis (100 cases/year)
Chronic: <5% (adult-acquired), >90% (perinatally-acquired); females are more likely to be chronic carriers
Extra-hepatic: Polyarteritis Nodosa (<1%), Membranoproliferative Glomerulonephritis
Transaminitis (↑ ALT/AST); See also Liver- LFTs (Chapter 4.20)
Serologic & Virologic:
Surface: “Far & Away” (i.e. Ag & Ab separated by window)
-HBsAg: appears before symptoms; used to screen blood donor; Neg = viral clearance
-anti-HBs: indicates resolution of acute disease & immunity (sole marker after vaccination)
Core: “In the middle” (i.e. Ab in the window)
-HBcAg not found in blood tests
-IgM anti-HBc: first Ab to appear; indicates acute infection
Window Period = HBsAg become −, anti-HBs not yet +, anti-HBc only clue to infection
Therefore, workup for suspected acute symptomatic HBV is HBsAg & IgM anti-HBc
-IgG anti-HBc: indicates previous (HBsAg−) or chronic (HBsAg+) HBV infection ‘Total core tests’ are both IgM and IgG and most labs use this as a screening; be careful!
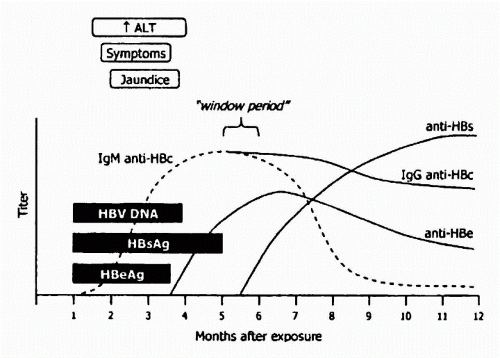
Reprinted with permission from Sabatine S: Pocket Medicine 2nd ed. Baltimore: Lippincott Williams & Wilkins, 2004:3-16.
E Particles: “Together” (i.e. Ag & Ab overlap)
-HBeAg: by product (evidence) of viral replication and defines ↑ infectivity/acute infection
Precore Variant: eAg not generated with +DNA, but anti-HBe can develop due to cross-reactivity with cAg
If HBeAg +, then HBV DNA must be +; If HBeAg −, then either Precore Variant (VL >100K), or Inactive Carrier (VL <100K)
-anti-HBe: indicates waning viral replication, ↓ infectivity/replication
DNA:
Biopsy: degree of inflammation (grade) & amount of fibrosis (stage); no other test makes this determination accurately
Stages (Fibrosis): 1. portal fibrosis, 2. periportal fibrosis, 3. septal fibrosis, 4. cirrhosis
Grade (Inflammation): 1. minimal lobular, 2. mild portal, 3. moderate piecemeal necrosis, 4. severe portal with piecemeal necrosis
Surface: | Core: | E Particles: | ||||
|---|---|---|---|---|---|---|
HBsAg | anti-HBs | anti-HBc | HBeAg | anti-HBe | DNA/ALT/Course of Action: | |
-Acute hepatitis: | + | − | IgM | + | − | + DNA, Observe, resolution likely 90% to 95% of adults |
-Window period: | − | − | IgM | ± | ± | +DNA |
-Recovery (prior exposure): | − | IgG | − | ± | −DNA (protected from further infection) | |
-Immunization: | − | − | − | − | −DNA (protected from further infection) | |
-Chronic (Replicative EAg+): | + | − | IgG | + | − | + DNA, ↑ ALT: EAg+/Wild Type, Initiate tx w/goal » Inactive Carrier |
Chronic (Immune Tolerant): | + | − | IgG | + | − | + DNA, nl ALT: Immune Tolerant, <5% respond to IFN, better with NA |
Chronic (Non-Replicative): | + | − | IgG | − | + | − or ↓ DNA, nl ALT: Chronic Inactive Carrier, Observe |
Chronic (Precore Variant): | + | − | IgG | − | ± | + DNA, ↑ ALT: EAg-/Precore Variant, Initiate tx (likely lifelong) |
-Isolated Core: | − | − | IgG | − | + | No significance, unless transplant patient* |
a Notice only options with + anti-HBs | ||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree