Chapter 13 Hepatic encephalopathy
1 The key to the diagnosis of hepatic encephalopathy is recognition that significant liver disease is present.
2 The occurrence of any neuropsychiatric symptoms or signs in a patient with significant liver dysfunction should be considered hepatic encephalopathy until proven otherwise.
3 Patients with suspected overt hepatic encephalopathy are managed by a four-pronged strategy: general care of the unconscious patient, exclusion of other causes of encephalopathy, correction of precipitating factors, and initiation of empirical therapy.
4 Hepatic encephalopathy associated with acute liver failure (type A) is rare, and its clinical course and treatment are distinct from those in chronic liver disease.
5 Many hypotheses on the pathogenesis of hepatic encephalopathy exist; however, operationally the ammonia concept is perfectly suited to the clinician caring for patients with hepatic encephalopathy.
Definition and Classification
1. Overt hepatic encephalopathy (OHE): a wide spectrum of neurologic and neuropsychiatric abnormalities in patients with significant liver dysfunction
2. Covert/minimal hepatic encephalopathy (covert HE): a disorder in which patients with cirrhosis have normal mental and neurologic status on clinical examination but exhibit reversible and quantifiable neuropsychologic and/or neuropsychiatric abnormalities
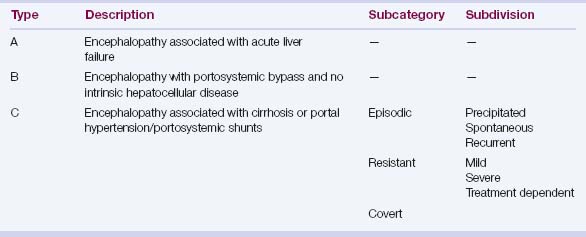
Table 13.1 depicts the Working Party classification of HE.
Pathophysiology
1. Failure of hepatic detoxification of neuroactive compounds arising from the gut; cross-circulation experiments in an animal model favor this theory.
2. Specific hypotheses of HE
 Ammonia: This compound is mainly derived from nitrogenous products in the diet, bacterial metabolism of urea, and deamination of glutamine by the enzyme glutaminase. Ammonia enters the portal circulation from the gut and is converted to urea in the liver. In the presence of significant portosystemic shunting, with or without hepatocellular dysfunction, ammonia concentration rises in blood and crosses the blood–brain barrier. Exposure to increased brain ammonia results in structural alterations in astrocytes that cause swelling and brain edema. Over a long period of exposure to high ammonia levels, astrocytes develop structural changes known as Alzheimer type II astrocytes.
Ammonia: This compound is mainly derived from nitrogenous products in the diet, bacterial metabolism of urea, and deamination of glutamine by the enzyme glutaminase. Ammonia enters the portal circulation from the gut and is converted to urea in the liver. In the presence of significant portosystemic shunting, with or without hepatocellular dysfunction, ammonia concentration rises in blood and crosses the blood–brain barrier. Exposure to increased brain ammonia results in structural alterations in astrocytes that cause swelling and brain edema. Over a long period of exposure to high ammonia levels, astrocytes develop structural changes known as Alzheimer type II astrocytes.
 Inflammation: It is now clearly evident that inflammatory mediators and cytokines play an important role along with hyperammonia in the pathogenesis of HE; possible mechanisms include cytokine-mediated changes in blood–brain barrier permeability, microglial activation and the subsequent production of neurosteroids, and altered activity of peripheral benzodiazepine binding sites.
Inflammation: It is now clearly evident that inflammatory mediators and cytokines play an important role along with hyperammonia in the pathogenesis of HE; possible mechanisms include cytokine-mediated changes in blood–brain barrier permeability, microglial activation and the subsequent production of neurosteroids, and altered activity of peripheral benzodiazepine binding sites.
 Accumulation of manganese in the basal ganglia: This is implicated in altered dopaminergic neurotransmission and extrapyramidal symptoms.
Accumulation of manganese in the basal ganglia: This is implicated in altered dopaminergic neurotransmission and extrapyramidal symptoms.
 Ammonia: This compound is mainly derived from nitrogenous products in the diet, bacterial metabolism of urea, and deamination of glutamine by the enzyme glutaminase. Ammonia enters the portal circulation from the gut and is converted to urea in the liver. In the presence of significant portosystemic shunting, with or without hepatocellular dysfunction, ammonia concentration rises in blood and crosses the blood–brain barrier. Exposure to increased brain ammonia results in structural alterations in astrocytes that cause swelling and brain edema. Over a long period of exposure to high ammonia levels, astrocytes develop structural changes known as Alzheimer type II astrocytes.
Ammonia: This compound is mainly derived from nitrogenous products in the diet, bacterial metabolism of urea, and deamination of glutamine by the enzyme glutaminase. Ammonia enters the portal circulation from the gut and is converted to urea in the liver. In the presence of significant portosystemic shunting, with or without hepatocellular dysfunction, ammonia concentration rises in blood and crosses the blood–brain barrier. Exposure to increased brain ammonia results in structural alterations in astrocytes that cause swelling and brain edema. Over a long period of exposure to high ammonia levels, astrocytes develop structural changes known as Alzheimer type II astrocytes. Inflammation: It is now clearly evident that inflammatory mediators and cytokines play an important role along with hyperammonia in the pathogenesis of HE; possible mechanisms include cytokine-mediated changes in blood–brain barrier permeability, microglial activation and the subsequent production of neurosteroids, and altered activity of peripheral benzodiazepine binding sites.
Inflammation: It is now clearly evident that inflammatory mediators and cytokines play an important role along with hyperammonia in the pathogenesis of HE; possible mechanisms include cytokine-mediated changes in blood–brain barrier permeability, microglial activation and the subsequent production of neurosteroids, and altered activity of peripheral benzodiazepine binding sites. Accumulation of manganese in the basal ganglia: This is implicated in altered dopaminergic neurotransmission and extrapyramidal symptoms.
Accumulation of manganese in the basal ganglia: This is implicated in altered dopaminergic neurotransmission and extrapyramidal symptoms.Clinical Features
2. Covert HE: patients with normal neurologic examination but abnormal neuropsychiatric test performance
Diagnosis
1. Consideration of the possibility of HE arises when significant liver dysfunction is known or suspected to be present. Clinical or laboratory evidence of liver failure and/or portal hypertension is usually obvious. However, in a minority of patients, evidence of significant liver dysfunction may be subtle, as in the following conditions:
The foregoing historical points, physical signs, and laboratory tests can individually or in combination indicate the presence of underlying liver dysfunction even when results of traditional tests of hepatic function, such as serum albumin and prothrombin times, are normal. Patients with well-preserved synthetic function of the liver do not commonly develop overt HE; a major precipitating factor is needed to induce an episode in such patients.
Covert Hepatic Encephalopathy
1. Covert HE is defined as abnormal performance on psychometric testing when a standard neurologic examination is completely normal.
3. It has a significant negative impact on quality of life and is associated with poor driving skills, impaired navigational skills, and increased traffic violations and accidents.
5. The International Society for Hepatic Encephalopathy recommends the Psychometric Hepatic Encephalopathy Score (PHES) as the gold standard for diagnosis of covert HE; impairment of greater than 2 SD in two or more tests in this battery is necessary for diagnosis of covert HE.
 LTT (Line Tracing Test): measures both speed and accuracy and has visuomotor and visuospatial components.
LTT (Line Tracing Test): measures both speed and accuracy and has visuomotor and visuospatial components.
 SDT (Serial Dotting Test): assesses psychomotor speed. It has failed to gain popularity because of the lack of availability of testing material and normative data for comparison in United States; the RBANS (Repeatable Battery for Assessment of Neuropsychologic Status) was developed in United States and is considered an equivalent test.
SDT (Serial Dotting Test): assesses psychomotor speed. It has failed to gain popularity because of the lack of availability of testing material and normative data for comparison in United States; the RBANS (Repeatable Battery for Assessment of Neuropsychologic Status) was developed in United States and is considered an equivalent test.
 LTT (Line Tracing Test): measures both speed and accuracy and has visuomotor and visuospatial components.
LTT (Line Tracing Test): measures both speed and accuracy and has visuomotor and visuospatial components. SDT (Serial Dotting Test): assesses psychomotor speed. It has failed to gain popularity because of the lack of availability of testing material and normative data for comparison in United States; the RBANS (Repeatable Battery for Assessment of Neuropsychologic Status) was developed in United States and is considered an equivalent test.
SDT (Serial Dotting Test): assesses psychomotor speed. It has failed to gain popularity because of the lack of availability of testing material and normative data for comparison in United States; the RBANS (Repeatable Battery for Assessment of Neuropsychologic Status) was developed in United States and is considered an equivalent test.