Hematology and Medical Oncology
Question 1
A 19-year-old African American man presents to the emergency department with severe abdominal pain and jaundice. His past medical history is unremarkable, although his mother reports “growing pains” as a child. Further questioning reveals that the patient is adopted. He is febrile and tachycardic. The abdomen is diffusely tender. No rebound is present, and bowel sounds are present throughout. A small skin ulcer is noted on his left lower extremity. Complete blood cell count shows white blood cells at 17 K/µL, hemoglobin at 6.3 g/dL, and mean corpuscular volume at 89 µm3. Aspartate transaminase and alanine transaminase values are normal. Indirect bilirubin is 3.6 mg/dL. A peripheral smear was performed and displays crescent-shaped RBCs. Which of the following statements regarding this patient’s condition is true?
a) Sepsis is the most common cause of death in adults.
b) In the United States, few patients survive beyond the fifth decade.
c) A selective advantage against Plasmodium vivax malaria is present.
d) Transmission is autosomal dominant with variable penetrance.
e) Symptoms do not develop until the patient is older than 6 months.
View Answer
Answer and Discussion
The answer is e.
Objective: Identify important epidemiologic and prognostic facts in sickle cell anemia.
This patient has sickle cell anemia (SSA), the most common heritable hematologic disease affecting humans. Inheritance is autosomal recessive, and among African American adults, SSA has a prevalence of 1 in 500, with 10% being carriers of the sickle trait. Patients have an electrophoretically abnormal hemoglobin (HgbS) that differs from HgbA by substitution of valine for glutamic acid at the sixth position of the β chain. On deoxygenation, HgbS begins to polymerize and changes the RBC from a biconcave disk to an elongated sickle shape. Patients with SSA have a selective advantage against Plasmodium falciparum malaria, with preferential sickling of parasitized cells. The rate of polymerization depends on the concentration of HgbS and the extent of deoxygenation. The sickling may be irreversible if enough cell damage occurs. Fetal hemoglobin (HgbF) is protective against polymerization and varies in its distribution among RBCs in patients with SSA. Signs and symptoms of the disease do not usually appear until the sixth month of life, at which time most HgbF has been replaced by HgbS. The most common cause of death in adult patients with SSA is from acute chest syndrome. Worldwide, approximately 120,000 babies with SSA are born each year, but <2% survive to the age of 5 years. In the United States and other developed countries, SSA patients often survive into their fifth or sixth decade.
Question 2
The patient proves to have squamous cell carcinoma of the lung and receives a course of mediastinal radiation therapy. The patient does quite well, noting rapid improvement in both the symptoms and signs of her superior vena cava obstruction. A staging workup subsequently demonstrates evidence of asymptomatic bone metastases in rib, femur, and multiple vertebral bodies. Because the patient is feeling well, she declines any discussion of chemotherapy and is followed in your office. Four months later, the patient calls you with the complaint of a 2-week history of increasing mid-back pain. The patient is fully ambulatory, but the pain is causing difficulty sleeping. The patient specifically denies any weakness in the lower extremities, radicular pain, or incontinence. You would do which of the following?
a) Suggest a course of acetaminophen with codeine
b) Order an elective bone scan
c) Refer the patient for radiation therapy to the spine
d) Order an MRI of the entire spine
View Answer
Answer and Discussion
The answer is d.
Objective: Recognize symptoms of cord compression.
Spinal metastases have already been demonstrated in this patient. The new development of pain suggests the possibility of spinal cord compression and mandates the performance of a whole spine MRI. While it is important to identify focal neurologic complaints and serial neurologic examinations are necessary, they are not essential to the diagnosis of cord compression. Cord compression is an oncologic emergency, and symptomatic relief without further workup is not recommended. The imaging modality of choice is an MRI of the whole spine. While a nuclear medicine bone scan may identify lytic lesions in the spine, it does not have adequate
sensitivity or specificity to identify cord compression. The treatment of choice depends on the MRI, and depending on the severity, may require urgent neurosurgical evaluation.
sensitivity or specificity to identify cord compression. The treatment of choice depends on the MRI, and depending on the severity, may require urgent neurosurgical evaluation.
Question 3
In the office, you perform a 1-L thoracentesis for slightly bloody fluid, which on analysis proves exudative. Cultures are negative, and cytologies are not diagnostic. The patient feels immediately better after the thoracentesis but returns to the office 3 days later with increasing dyspnea and recurrence of this effusion. Your next step is which of the following?
a) Repeat the thoracentesis with cytology
b) Repeat the thoracentesis with cytology and perform a closed pleural biopsy
c) Refer the patient for thoracoscopy
d) Refer the patient for chest tube drainage and pleural sclerosis
View Answer
Answer and Discussion
The answer is d.
Objective: Identify therapeutic strategies for likely recurrent malignant effusion.
In a patient with a diagnosed malignancy and recurrent pleural effusions, the pre-test probability of a malignant effusion is fairly high. Attempts to confirm the diagnosis may be difficult due to the low sensitivity of pleural fluid cytology. In a patient this sick with recurrent symptomatic effusions, it may be most prudent to forego further aggressive attempts to confirm the likely diagnosis of a malignant pleural effusion and to proceed directly to appropriate management. Repeat thoracentesis will provide temporary symptomatic relief, but will need to be repeated frequently. Thoracoscopy is a diagnostic maneuver and will offer no significant therapeutic benefit. Chest tube drainage followed by pleural sclerosis is the most likely definitive management for this patient’s recurrent effusions.
Question 4
You are following a 65-year-old man with a recently diagnosed acute myeloid leukemia initiated on induction chemotherapy. The patient has onset of heart palpitations, numbness and tingling in his hands and feet, and severe pain in his right big toe. You are concerned about tumor lysis syndrome. Tumor lysis syndrome is associated with all the following, except
a) Hypercalcemia
b) Hyperkalemia
c) Hyperphosphatemia
d) Hyperuricemia
View Answer
Answer and Discussion
The answer is a.
Objective: Identify lab abnormalities in tumor lysis syndrome.
Tumor lysis syndrome (TLS) is a known and often profound complication of any malignancy, but is most often seen in acute hematologic malignancies after initiation of cytotoxic chemotherapy. Some of the other risk factors associated with TLS are high tumor cell proliferation rate, large tumor burden, and chemosensitivity of the malignancy. Laboratory abnormalities of TLS center around release of intracellular products, leading to hyperuricemia, hyperkalemia, and hyperphosphatemia among others. Hyperphosphatemia can then lead to a secondary hypocalcemia with precipitation of calcium phosphate, which can lead to deposition in renal tubules leading to rapidly progressive renal failure. Symptoms of TLS center around these electrolyte abnormalities, and lead to a very heterogeneous presentation.
Question 5
A 24-year-old woman presents for an annual gynecologic examination. She has never had a Papanicolaou (Pap) smear and has been sexually active since age 19 years with five lifetime partners to date. She has not had any pregnancies or sexually transmitted diseases. What do you recommend regarding her gynecologic screening and care?
a) No screening currently necessary
b) Pap smear alone
c) Pap smear and human papillomavirus (HPV) testing
d) Pap smear and HPV vaccine
e) None of the above
View Answer
Answer and Discussion
The answer is d.
Objective: Identify indications for cervical cancer screening and HPV vaccination.
According to the United States Preventative Services Task Force (USPSTF) update in 2012, cervical cancer screening should begin at age 21 years for all patients with Papanicolaou (Pap) smear screening. The recommendation for screening women between 21 and 65 years of age for cervical cancer is cytology testing every 3 years with reflexive HPV testing. In women older than 30 years, concurrent Pap and HPV testing every 5 years can replace cytology testing with Pap smear alone every 3 years. By the age of 30, most transient HPV infections have cleared. However, current recommendations are to vaccinate all women aged 11 to 12 years, catch up vaccination for women aged 13 to 26 years, and consideration for vaccination of girls aged 9 to 10 years.
Question 6
A 56-year-old woman had a recent diagnosis of breast cancer. She underwent breast lumpectomy with negative lymph nodes and negative margins, breast irradiation, and is now on tamoxifen. Due to the increased risk of endometrial cancer with tamoxifen use, you recommend
a) Hysterectomy ± bilateral salpingo-oophorectomy
b) An endometrial biopsy at least every 6 months while on tamoxifen therapy
c) Annual ultrasound screening while on tamoxifen
d) Evaluation only if symptoms arise
e) Oral progesterone therapy
View Answer
Answer and Discussion
The answer is d.
Objective: Identify risk of endometrial cancer and recommended screening in women taking tamoxifen.
Tamoxifen is associated with an increased risk of endometrial cancer (estimated ˜1 in 500). However, studies have not shown any benefit to screening women taking tamoxifen with either ultrasound or biopsy. Symptoms should drive any additional workup for identifying potential endometrial cancer in women taking tamoxifen. Common symptoms include vaginal bleeding or discharge. Evaluation should include ultrasound measurement of endometrial thickness and hysteroscopy with biopsy.
Question 7
A 74-year-old obese white woman presents with vaginal bleeding. You do an endometrial biopsy and find a grade 1 endometrial carcinoma. She asks about her primary mode for therapy, and you tell her
a) Whole pelvic radiation is the primary treatment modality in women older than 70 years
b) Hysterectomy, oophorectomy, and staging are the best initial approaches
c) A trial of progesterone and repeat biopsy in 3 months would have high cure rates
d) Concomitant chemoradiation has been shown to improve survival in locally advanced endometrial cancer
e) None of the above
View Answer
Answer and Discussion
The answer is b.
Objective: Identify treatment modality for endometrial cancer.
Current standard of care for women with endometrial cancer is surgical staging with hysterectomy, salpingo-oophorectomy, and staging lymph node sampling. Radiation can be used as primary therapy in medically inoperable patients, and hormonal therapy can be used cautiously in young women who want to preserve their fertility. There are currently no data to support chemoradiation in endometrial cancer.
Question 8
A healthy 42-year-old female patient asks about screening for ovarian cancer. She has no symptoms suggestive of the disease, and the results of her physical examination are normal. You should
a) Ask about her family history of ovarian and breast cancers
b) Strongly recommend yearly screening until at least age 70 years
c) Recommend a CA-125 blood test and transvaginal ultrasonography
d) Recommend consultation for prophylactic oophorectomy
e) None of the above
View Answer
Answer and Discussion
The answer is a.
Objective: Identify screening strategies for ovarian cancer.
Currently, no evidence suggests that screening for ovarian cancer reduces mortality from this malignancy. If there are multiple women with breast or ovarian cancer, particularly at young ages, these women should be referred for genetic counseling and testing. High-risk patients can then be offered screening. However, it can certainly be argued that screening at least has the potential for detecting the disease at an earlier point in time when therapy may be more effective. A woman undergoing such screening must be informed of the limited data supporting this therapeutic strategy.
Question 9
A 53-year-old female patient with abdominal bloating and a large pelvic mass, carcinomatosis, and CA-125 of 1,340 U/mL presents to discuss paracentesis results showing adenocarcinoma. She asks for your recommendation regarding treatment. Which one of the following would be the best recommendation in this setting?
a) Refer for colonoscopy and esophagogastroduodenoscopy
b) Begin neoadjuvant chemotherapy while awaiting surgical consultation
c) Give six cycles of cisplatin or carboplatin plus paclitaxel, and then repeat abdominal imaging to assess response
d) Referral for surgical tumor resection followed by cisplatin or carboplatin plus A taxane
e) None of the above
View Answer
Answer and Discussion
The answer is d.
Objective: Identify appropriate therapy for metastatic ovarian cancer.
The standard treatment for advanced ovarian cancer is surgical debulking, followed by cisplatin or carboplatin, plus paclitaxel chemotherapy regimen. No evidence suggests that neoadjuvant chemotherapy or chemotherapy alone is more beneficial than the surgery plus chemotherapy. Given the overwhelming evidence for a primary ovarian cancer, additional diagnostic testing for another primary malignancy, including colonoscopy and esophagogastroduodenoscopy, would not be appropriate.
Question 10
A 67-year-old man, 4 years status post prostatectomy presents with low back pain and tenderness. His prostate-specific antigen is 185, and a bone scan is positive in multiple areas. The most appropriate treatment is
a) Orchiectomy
b) Radiation therapy to the prostate bed followed by orchiectomy
c) Chemotherapy with docetaxel
d) Bicalutamide (Casodex) followed by goserelin (Zoladex) subcutaneously every 3 months
e) a or d
View Answer
Answer and Discussion
The answer is e.
Objective: Identify appropriate therapeutic strategy for recurrent, metastatic prostate cancer.
Orchiectomy (a) or bicalutamide followed by goserelin (d) represents appropriate initial hormone therapy for patients with systemic disease from metastatic prostate cancer. Bicalutamide is given before goserelin for approximately 10 days to prevent the stimulation of prostate cancer growth that accompanies the transient surge in testosterone production that occurs shortly after the initiation of luteinizing hormone-releasing hormone agonists (goserelin or leuprolide). The great majority of men have rapid systematic relief, with a radiographic response as well. Radiation to the prostate bed (b) has no role for a patient with metastatic cancer and, therefore, would be performed prior to orchiectomy. Chemotherapy (c) is appropriate for the patient whose disease progresses on hormone therapy.
Question 11
A 28-year-old male baseball star presents with a painless left testicular mass. Physical examination is otherwise normal. α-Fetoprotein is >400. The most appropriate next step is
a) Testicular ultrasound
b) Ultrasound-guided transscrotal testicular biopsy
c) Inguinal orchiectomy
d) Trial of antibiotics
e) Whole body positron emission tomography scan
View Answer
Answer and Discussion
The answer is a.
Objective: Identify diagnostic strategy for suspected testicular cancer.
Testicular ultrasound (a) is the initial diagnostic test of choice for any patient who presents with a testicular mass. Although one might argue that an α-fetoprotein level of 400 in a young man with a testicular mass is essentially diagnostic of testicular cancer, an ultrasound is still an important first step followed by radical inguinal orchiectomy (c). A transscrotal testicular biopsy (b) is contraindicated due to the violation of tissue planes, which allows alternate lymphatic avenues of metastasis. A trial of antibiotics (d) is not warranted in a patient who has a painless left testicular mass and no testicular tenderness to suggest epididymitis or some other infectious etiology. A whole body positron emission tomography scan (e) is not a staging procedure at the initial diagnosis of testicular cancer. CT scanning of the chest, abdomen, and pelvis is the standard staging workup, but would not be pursued before a diagnosis has been confirmed.
Question 12
A 22-year-old man with testicular cancer comes back to your office 5 months after a radical inguinal orchiectomy and chemotherapy for nonseminomatous germ cell tumor. The patient feels well and has no complaints. His markers (α-fetoprotein, β-HCG, and LDH) normalized with treatment and remain normal. A mass is palpated in the left midabdomen. This mass is most likely
a) A mature teratoma, best treated with surgical resection
b) Recurrent testicular cancer, best treated with high-dose chemotherapy and autologous stem cell rescue
c) Seminoma, best treated with radiation therapy
d) Chemotherapy-induced chloroma (solid tumor manifestation of acute leukemia), best treated with radiation and chemotherapy
View Answer
Answer and Discussion
The answer is a.
Objective: Diagnose and treat a mature teratoma after therapy for nonseminomatous germ cell tumor.
Mature teratoma (a) is a well-known phenomenon that can occur after the successful treatment of nonseminomas, particularly those that contain a component of teratoma. Such a mass is generally curable with surgical resection. Left untreated, these masses can degenerate into malignant teratomas that are not curable. Recurrent testicular cancer (b) can certainly occur but is an unusual phenomenon and, in the setting of tumor markers that remain normal, would be highly unlikely. Seminoma (c) would similarly be extremely unusual after chemotherapy for a nonseminoma. Chemotherapy-induced acute leukemia (d) is a welldescribed complication of chemotherapy but occurs with a latency of 2 to 9 years. In addition, a patient with acute leukemia and tumor bulk consisting of a chloroma would not generally be asymptomatic.
Question 13
A 35-year-old woman presents to the emergency room with 24 hours of fever and chills. In addition, she complains of increasing fatigue, dyspnea on exertion, and spontaneous bruising.
On physical examination, she appears ill; her vitals are temperature 39.5°C, blood pressure 80/40 mmHg, pulse 140 beats/minute, respiration rate 22 breaths/minute, petechiae on soft palate, no lymphadenopathy, clear lungs, tachycardia, I/VI systolic ejection murmur, no abdominal mass or hepatosplenomegaly, and scattered petechiae, especially on lower extremities.
Her laboratory values are hemoglobin, 8.7; platelets, 14,000; white blood cells, 3,000, with 2% neutrophils, 45% lymphocytes, and 53% blasts; international normalized ratio, 1.1; partial thromboplastin time, 23; and fibrinogen, 345.
Her peripheral blood smear shows normochromic, normocytic anemia; thrombocytopenia; rare neutrophils; and many blasts.
The best course of action is to immediately
a) Withhold antibiotics until the source of infection is identified
b) Fluid resuscitate and start piperacillin and gentamicin
c) Fluid resuscitate and give granulocyte transfusion
d) Perform bone marrow aspirate and biopsy
View Answer
Answer and Discussion
The answer is b.
Objective: Treat life-threatening sepsis in a neutropenic patient.
This patient has life-threatening sepsis and must be admitted for fluid resuscitation; a quick evaluation including blood cultures; and the administration of empiric, broad-spectrum intravenous antibiotics. Broad-spectrum antibiotics should specifically target gram-negative bacilli, as this is the predominant group of pathogens involved in neutropenic patients. Empiric coverage of gram-positive agents in this patient would not be inappropriate, but should not supersede coverage of gram-negative agents. While every attempt to obtain cultures prior to initiation of antibiotics should be made, antibiotics should not be withheld to identify a source, as time to antibiotic initiation has been shown to directly correlate with mortality. She is anemic, thrombocytopenic, has spontaneous bruising, and is at risk for life-threatening hemorrhage. She will likely need transfusion with RBCs and platelets. However, there is no clear role for granulocyte transfusions. Bone marrow aspirate and biopsy may be needed in the future to diagnose etiology of her neutropenia, but are not indicated at this time.
Question 14
A 25-year-old man presents to the emergency room complaining of dyspnea on exertion for several days. Recently, he has noted frequent nasal congestion and occasional epistaxis. He denies fevers, night sweats, and weight loss, and has noted a rash on his legs. He denies any hospitalizations or history of transfusions.
On physical examination, you find a well-developed man in no acute distress; temperature 36.8°C, blood pressure 126/74 mmHg, respiration rate 20 breaths/minute; his oral mucosa has a few petechial hemorrhages, the skin of the pretibial area is covered with petechial hemorrhages, and no palpable lymphadenopathy or splenomegaly is present; he is otherwise normal.
His laboratory values are hemoglobin, 8.3; platelets, 32,000; white blood cells, 1,100, with 1% neutrophils, 73% lymphocytes, 13% monocytes, and 13% blasts; prothrombin time, 20; international normalized ratio (INR), 2.1; partial thromboplastin time, 40; and fibrinogen, 90.
His peripheral smear shows pancytopenia, circulating blasts with Auer rods, and occasional schistocytes. A bone marrow aspirate and biopsy is hypercellular with 85% blasts and immature granulocytes.
The most important next step is to
a) Confirm the diagnosis with cytogenetic analysis
b) Start piperacillin and gentamicin
c) Transfuse platelets and fresh-frozen plasma
d) Start chemotherapy
View Answer
Answer and Discussion
The answer is d.
Objective: Diagnose and treat acute promyelocytic leukemia.
This patient probably has acute promyelocytic leukemia, given the obvious Auer rods and evidence of a significant coagulopathy, likely disseminated intravascular coagulopathy (DIC) as evidenced by anemia, thrombocytopenia, elevated INR, and low fibrinogen. Both plasma and platelets are needed to reduce the incidence of fatal hemorrhage. In the absence of fever or other signs of infection, antibiotics are not recommended for neutropenia. Prophylactic antibiotics are controversial but have not consistently been shown to improve survival. Urgent therapy is needed, but chemotherapy may precipitate a worsening of the coagulopathy. All-trans retinoic acid is usually started before chemotherapy in order to reduce the incidence of severe bleeding.
Question 15
A 29-year-old woman presents to your office for a Papanicolaou smear. She is asymptomatic and has a normal physical examination except for a moderately enlarged spleen.
Her laboratory values are hemoglobin, 11.9; platelets, 671,000; and white blood cells, 227,000, with 55% neutrophils, 7% metamyelocytes, 19% myelocytes, 2% promyelocytes, 2% blasts, 1% eosinophils, 7% basophils, and 3% lymphocytes. A bone marrow chromosome analysis shows 46,XX, t(9;22).
The most important next step is to
a) Immediately hospitalize
b) Start chemotherapy
c) Tissue-type the patient and her siblings to consider bone marrow transplantation
d) Start imatinib
View Answer
Answer and Discussion
The answer is d.
Objective: Diagnose and treat chronic myelogenous leukemia (CML).
This patient’s signs, symptoms, complete blood count, and bone marrow are characteristic of CML. The t(9;22) is the Philadelphia chromosome, which secures the diagnosis. The high white blood cell count requires neither leukapheresis nor hospitalization. Unlike a high blast count, a high neutrophil count does not increase the risk of leukostasis and hyperviscosity syndrome. Hydroxyurea, and other chemotherapeutic agents, will not prevent the progression of CML to blast crisis. The only known curative therapy is bone marrow transplant,
but this procedure carries a significant risk of early mortality. Because imatinib induces long-lasting remissions in the majority of patients, transplant is usually deferred until the time imatinib and other tyrosine kinase inhibitors fail.
but this procedure carries a significant risk of early mortality. Because imatinib induces long-lasting remissions in the majority of patients, transplant is usually deferred until the time imatinib and other tyrosine kinase inhibitors fail.
Question 16
A 35-year-old man with acute myelogenous leukemia has been severely neutropenic for 10 days and has been febrile with temperatures >38.5°C for the past 5 days. He has been on piperacillin, gentamicin, and vancomycin for 8 days. No localizing signs of infection are present on examination, and all cultures are negative to date. The most appropriate course of action would be to
a) Continue current antibiotics
b) Change antibiotics to imipenem
c) Add voriconazole
d) Draw fungal cultures and continue current antibiotics
View Answer
Answer and Discussion
The answer is c.
Objective: Identify risk of fungal infections in a neutropenic patient.
As the duration of neutropenia increases, the risk of fungal infection increases. This is particularly true in the setting of broad-spectrum antibacterials. This patient is at high risk for fungal infection. The current antibiotics are failing; thus continuing them with no other changes is inappropriate. A change to imipenem might cover additional bacterial pathogens, but does not address the risk of fungal infection. Fungal infections are difficult to isolate. Clinical studies have clearly demonstrated the importance of empiric antifungal therapy. Thus, voriconazole is the correct choice.
Question 17
A 75-year-old man with a 5-year history of untreated, chronic lymphocytic leukemia presents with fatigue and a peculiar craving for ice. Examination reveals generalized, but small peripheral lymphadenopathy and a barely palpable spleen tip. His laboratory values are white blood cells, 34,000; hemoglobin, 5.2; and platelets, 133,000; reticulocytes 2%; direct Coombs’ test negative; and lactate dehydrogenase and bilirubin normal. The peripheral blood smear demonstrates normocytic red cells and no polychromasia. The most likely cause of anemia in this patient is
a) Pure red cell aplasia
b) Autoimmune hemolytic anemia
c) Bone marrow infiltration with leukemia
d) Gastrointestinal bleeding
View Answer
Answer and Discussion
The answer is d.
Objective: Identify causes of anemia in patients with chronic lymphocytic leukemia (CLL).
CLL is a fairly common lymphoproliferative disorder in the older patient population. Although CLL may be the direct cause of anemia in some patients, it is important to remember that these patients are also at risk for other problems as well. This particular patient has pica, a very specific symptom of iron deficiency anemia. Even though the red cells are not microcytic, iron deficiency anemia is still possible, especially if the onset is relatively rapid. Pure red cell aplasia is another possibility, but less likely given the indolent nature of the patient’s leukemia and the presence of pica. Similarly, infiltration of the marrow with leukemia in an untreated patient would not likely be enough to induce this degree of anemia given the nonbulky lymph nodes, modest splenomegaly, and modest leukocytosis. The absence of microspherocytes, reticulocytosis, and a negative Coombs’ test make autoimmune hemolytic anemia (AIHA) the least likely cause of anemia in this patient, but AIHA is a common cause of anemia in patients with CLL.
Question 18
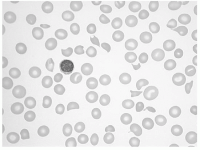
At 2:00 AM, a young woman presents to the emergency department of a small rural community hospital complaining of headache and fever. Except for some pallor, mild scleral icterus, and sleepiness, the physical examination is normal. The complete blood count report comes back with “low platelets” and a hematocrit of 28%. The prothrombin time/activated partial thromboplastin time and electrolytes are normal. The lab sends down the peripheral smear, which you examine under the microscope.
|
The next best step is
a) Immediate broad-spectrum antibiotics for probable meningococcal sepsis
b) Platelet transfusions to control a probable intracerebral bleed
c) High-dose steroids for probable autoimmune thrombocytopenia with autoimmune hemolytic anemia (Evan’s syndrome)
d) Immediate transfusions of fresh-frozen plasma
View Answer
Answer and Discussion
The answer is d.
Objective: Diagnose and treat thrombotic thrombocytopenic purpura (TTP).
The diagnosis of TTP is easily made given the clear evidence of microangiopathic hemolysis (arrows show schistocytes on blood smear) associated with thrombocytopenia, fever, and neurologic signs/symptoms. With this degree of thrombocytopenia and hemolysis, a normal prothrombin time/activated partial thromboplastin time effectively rules out disseminated intravascular coagulation, thus making sepsis unlikely. Autoimmune hemolytic anemia does not produce schistocytes, but rather produces spherocytes. Platelet transfusions are relatively contraindicated in TTP because of their potential to aggravate thrombosis. Ideally, the patient should receive plasmapheresis with fresh-frozen plasma (FFP) replacement; however, in the emergency setting in a rural emergency department, the first available treatment is transfusion with large volumes of FFP while making arrangements for transfer to an institution that can perform apheresis.
Question 19
An asymptomatic 59-year-old woman was referred to you for preoperative clearance for a planned open colectomy. The routine laboratory examinations were all normal except for an elevated activated partial thromboplastin time (aPTT) of 57 seconds. She denied any history of excess bleeding or bruising. The lab calls you the next day to inform you that when they mixed her plasma 1:1 with pooled normal plasma, the aPTT was 43 seconds, normal being <31 seconds. Which of the following is most likely true?
a) The story is most consistent with mild von Willebrand disease, and the patient should be treated preoperatively with DDAVP (desmopressin).
b) The most likely diagnosis is “lupus anticoagulant,” and the patient needs to receive perioperative thromboprophylactic therapy because of the increased risk of venous thromboembolism.
c) The woman likely has congenital factor XI deficiency and needs to have fresh-frozen plasma administered prior to surgery.
d) The woman most likely has an acquired, autoimmune factor VIII inhibitor and needs aggressive immune suppressive therapy prior to surgery.
View Answer
Answer and Discussion
The answer is b.
Objective: Identify causes of elevated coagulation studies.
The aPTT would correct to normal if the patient had von Willebrand disease or congenital factor XI deficiency because the aPTT prolongs only if factor levels drop below ˜40% of normal. Acquired factor VIII inhibitors are almost always associated with severe bleeding and bruising. Thus, the likely scenario here is lupus anticoagulant, a finding seen with the antiphospholipid syndrome. This is a significant risk factor for thrombosis, and the additional prothrombotic stress of general surgery mandates thromboprophylaxis.
Question 20
Mr. Jones is a 77-year-old retired steel worker who is widowed and lives alone in a two-story house. He was brought to the emergency room (ER) by his daughter because of an extremely painful, swollen, red right leg. He believed that maybe he twisted his knee while walking down the stairs in his home, but when the pain and swelling did not improve after 24 hours and the swelling extended up into his thigh, he called his daughter who immediately brought him to the ER. A physical examination revealed normal vital signs; mild degenerative joint disease; and a swollen, erythematous right leg. A duplex Doppler was performed and revealed a large occlusive thrombus extending from the popliteal vein to the iliofemoral system. Chest x-ray and ECG were normal, and the physician in the infirmary gave him a prescription for enoxaparin and warfarin and referred him to your office. You saw him 3 days later, at which time his international normalized ratio was 2.8. You take a detailed history and discover that he has been feeling “poorly” for about 2 months. He notices a definite loss of energy, decreased appetite, and constipation. Physical examination reveals a rather frail elderly man with muscle wasting in the temporal region. Prostate is 3+ enlarged but without nodules. Stool is negative for occult blood. The remainder of the examination is negative except for the right leg, which is still swollen and tender, although no longer red. The most appropriate course of action at this point is to
a) Obtain colonoscopy
b) Stop the enoxaparin because his international normalized ratio is now therapeutic
c) Obtain thrombophilia panel, including factor V Leiden assay, to guide decision on duration of anticoagulation
d) Obtain plasma anti-Xa assay to assess enoxaparin dosing because his leg is still swollen and tender
View Answer
Answer and Discussion
The answer is a.
Objective: Identify deep venous thrombosis as a potential complication of malignancy.
An underlying malignancy is the most likely etiology of his thrombophilia, and the presence of an inherited or other acquired thrombophilia is not likely to influence therapeutic decisions. Randomized trials showed that heparin therapy should always be extended for at least 5 days in patients with venous thromboembolism, even if the international normalized ratio (INR) is therapeutic. In fact, newer studies suggest that low molecular weight heparins are more effective than warfarin in long-term treatment of cancer-associated venous thrombosis. In this case, the rapid INR response is probably due to underlying vitamin K deficiency from malnutrition. Resolution of symptoms from severe deep vein thrombosis
can take many days; persistent swelling at day 3 is not an indication of inadequate heparin effect.
can take many days; persistent swelling at day 3 is not an indication of inadequate heparin effect.
Question 21
Which of the following bleeding disorders can be present despite normal screening coagulation studies (PT, aPTT, and PFA-100)?
a) Mild von Willebrand disease
b) Mild hemophilia
c) Factor XIII deficiency
d) α-Antiplasmin deficiency
e) All of the above
View Answer
Answer and Discussion
The answer is e.
Objective: Identify role of coagulation studies in bleeding disorders.
Mild coagulation factor deficiencies can be difficult to diagnosis because the screening assays are sensitive only to levels below 30% to 40% of normal. Disorders of clot stability, including fibrinolysis defects (e.g., 2-antiplasmin deficiency) and abnormal fibrin clot cross-linking (factor XIII deficiency), will not affect prothrombin time or activated partial thromboplastin time. von Willebrand factor levels fluctuate greatly and are sensitive to estrogen levels and acute inflammation so that platelet screening tests can be normal in patients with mild von Willebrand disease.
Question 22
A 56-year-old man has an uneventful mitral valve replacement surgery. Heparin was given during the procedure and continued postoperatively. On the eighth postoperative day, he develops a painful, cold, pulseless leg. His activated partial thromboplastin time is subtherapeutic at 39 seconds. His platelet count is 55,000/µL (112,000 on postop day 1). The most important next step in his management is to
a) Obtain a vascular surgery consultation for revascularization
b) Increase the dose of heparin to obtain a therapeutic-activated partial thromboplastin time
c) Perform platelet transfusion to increase count to >100,000/µL
d) Discontinue all heparin immediately
e) Begin warfarin and order anti-PF4 antibody test so that heparin can be safely stopped if the test is positive
View Answer
Answer and Discussion
The answer is d.
Objective: Identify appropriate therapeutic strategy for presumed heparin-induced thrombocytopenia (HIT).
If HIT is suspected, as it should be in this case of acute thrombosis in the setting of a 50% drop in platelet count, then it is critical to stop all heparin (including catheter flushes immediately) and initiate therapy with a direct thrombin inhibitor. Giving more heparin or infusing platelets are associated with worse outcomes. Vascular surgery may be helpful, but not before stopping the heparin. Warfarin has been associated with cutaneous thrombosis and necrosis in the setting of HIT and should not be used acutely.
Question 23
Which of the following is true of DDAVP (desmopressin)?
a) Is an analog of vasopressin and can cause hypernatremia
b) Should not be given chronically to prevent bleeding in patients with moderate von Willebrand disease (vWD)
c) Does not have efficacy in several mild platelet disorders, such as storage pool defect
d) Can be used in all causes of vWD
View Answer
Answer and Discussion
The answer is b.
Objective: Identify indications for DDAVP (desmopressin).
DDAVP is an analog of vasopressin and therefore can cause hyponatremia by increasing the activity of the ADH axis. It also has been shown to stimulate the release of von Willebrand factor from endothelial cells. However, tachyphylaxis occurs with this drug so that efficacy typically disappears after two or three sequential doses. Thus, it cannot be given chronically. Type IIB vWD is associated with a gain-of-function mutation such that when von Willebrand factor binds to glycoprotein 1, it leads to increased clearance of platelets. DDAVP, which stimulates release of von Willebrand factor, can cause thrombosis and/or severe thrombocytopenia in patients with type IIB vWD and, thus, should not be used in that setting.
Question 24
A 22-year-old sexually active female college student is referred to you from the Student Health Service because of a low platelet count (18,000/µL) that was discovered when a complete blood count (CBC) was obtained to evaluate a rash on her lower extremities. She has been feeling otherwise well, but has noted some gum bleeding when she brushes her teeth over the past few days. She takes no medications other than a multivitamin. She had a normal CBC at the time of her college physical. The following would be an appropriate next step:
a) Immediately obtain bone marrow aspirate
b) Begin therapy with intravenous immunoglobulin G because her platelet count is so low
c) Send out tests for hepatitis C and HIV
d) Send out tests to rule out systemic lupus erythematosus
View Answer
Answer and Discussion
The answer is c.
Objective: Identify risk factors for ITP.
The most likely diagnosis is idiopathic/immune-mediated thrombocytopenic purpura (ITP), and in a young woman
with no other likely cause of thrombocytopenia, a bone marrow aspirate is not necessary. Intravenous immunoglobulin is not considered first-line therapy in the absence of major bleeding; rather, prednisone at 1 mg/kg/day would be the preferred medical therapy. Although lupus is associated with ITP, finding a positive ANA or anti-DNA would not change management. HIV and hepatitis C are not uncommon causes of ITP in young, sexually active patients and should always be ruled out.
with no other likely cause of thrombocytopenia, a bone marrow aspirate is not necessary. Intravenous immunoglobulin is not considered first-line therapy in the absence of major bleeding; rather, prednisone at 1 mg/kg/day would be the preferred medical therapy. Although lupus is associated with ITP, finding a positive ANA or anti-DNA would not change management. HIV and hepatitis C are not uncommon causes of ITP in young, sexually active patients and should always be ruled out.
Question 25
You are called to the surgical intensive care unit to consult on a case of a 60-year-old 75 kg male chronic alcoholic who was admitted with a severe gastrointestinal bleed. After resuscitation with 4 units of packed RBCs, he was noted to have a hemoglobin of 11 g/dL, an activated partial thromboplastin time (aPTT) of 90 seconds, a prothrombin time (PT) of 24 seconds, a platelet count of 90,000, and a bilirubin of 12.
The lab reported that a 50:50 mix of his plasma with pooled normal plasma corrected both the aPTT and PT to normal. Appropriate therapeutic interventions include
a) Transfuse 2 units of fresh-frozen plasma now and repeat every 8 hours
b) Administer low-dose heparin to stop the DIC process
c) Administer high-dose steroids to raise the platelet count
d) None of the above
View Answer
Answer and Discussion
The answer is d.
Objective: Identify expected correction of coagulopathy with transfusion.
This patient has a profound coagulopathy, likely due to hepatic failure, although a component of vitamin K deficiency could also be present. There is no evidence to support disseminated intravascular coagulation. The modest thrombocytopenia is probably multifactorial in origin, including splenomegaly from portal hypertension and alcohol-related marrow toxicity; high-dose steroids are not likely to have a significant effect. The appropriate treatment is transfusion of fresh-frozen plasma, but he will need far more than 2 units to correct his severe factor deficiency, and dosing every 8 hours will not be adequate. While every patient responds differently to fresh-frozen plasma, current thought is that 10% increase in coagulation factors is the minimum required to see any clinical response. In an average 70 kg patient, 4 units of fresh frozen plasma would achieve ˜10% increase in coagulation factors.
Question 26
Ms. Smith is an 82-year-old widow who lives alone and has been brought to your emergency department by her niece who notes that her aunt has been “failing” for the past 2 to 3 months. Other than long-standing hypertension, the medical history is noncontributory. Physical examination reveals a sleepy, thin elderly woman with pedal edema, blood pressure of 190/110 mmHg, and S3 gallop. Laboratory values are remarkable for hemoglobin of 7 g/dL, creatinine of 9.2, and blood urea nitrogen of 123. That evening, she develops a severe nose bleed that requires packing by the ear/nose/throat service and also notices bleeding external hemorrhoids. Which of the following can be used to improve her hemostasis?
a) Aggressive dialysis to resolve her uremic state
b) Packed RBC transfusion and erythropoietin to bring her hemoglobin to >10 g/dL
c) Intravenous desmopressin
d) High doses of estrogen
e) All of the above
View Answer
Answer and Discussion
The answer is e.
Objective: Identify therapeutic strategies for uremic platelet dysfunction.
Uremia is associated with a moderate to severe multifactorial bleeding diathesis that can be improved with dialysis and that responds partially to pharmacologic intervention with DDAVP (desmopressin) (can only be used acutely) or estrogen (can be used more chronically). One function of RBCs is to “push” platelets to the outer edge of the column of flowing blood, maximizing their interaction with the vascular wall. Thus, the bleeding time is negatively influenced by severe anemia and can be improved by treating the anemia.
Question 27
You are asked to see a 62-year-old man who is 4 days status post elective total hip replacement. He has been treated since the night before surgery with enoxaparin, 40 mg/day, but now has developed a symptomatic deep vein thrombosis on the same side as the surgery. Your plan is to increase the low molecular weight heparin dose and start warfarin until you recall that these drugs can adversely affect hypercoagulability testing. What tests do you order before beginning therapy?
a) Factor V Leiden, prothrombin gene mutation, and homocysteine level
b) Protein C, protein S, and antithrombin III levels
c) Lupus anticoagulant and anticardiolipin antibody levels
d) All of the above
e) None of the above
View Answer
Answer and Discussion
The answer is e.
Objective: Identify indications for hypercoagulability testing in a provoked DVT.
The patient has a “provoked” or “situational” venous thrombosis associated with the hip surgery. Even in the setting of adequate thromboprophylaxis, venous thrombosis occurs at a frequency of 1% to 4%. The results of testing are unlikely to impact clinical decisions regarding the duration, intensity, or type of anticoagulation therapy in this setting.
Question 28
A 31-year-old woman presents with complaints of fatigue, dyspnea on exertion, and tinnitus. The symptoms started 1 month ago. She had previously been in “perfect health.” She has had three normal pregnancies. Her physical examination is remarkable for pallor. The hemoglobin concentration is 7.5 g/dL, the white blood cell count is 6,200, and her platelet count is 550,000/µL. After her last pregnancy 2 years ago, her hemoglobin was normal. Which of the following tests is the most appropriate first test in the initial evaluation of this patient’s anemia?
a) Serum folate and vitamin B12 level
b) Review of the peripheral blood smear
c) Serum ferritin determination
d) Haptoglobin level
e) Coombs’ direct and indirect tests
View Answer
Answer and Discussion
The answer is b.
Objective: Identify initial workup of new anemia.
A review of the peripheral blood smear (PBS) is the single most valuable first step in evaluating an acute anemia. The morphology of the RBCs, the presence of polychromasia (reticulocytes), and platelet morphology can help focus the differential diagnosis and evaluation immediately. The differential diagnosis for this patient’s acute or subacute anemia is broad and includes both gastrointestinal blood loss and diverse causes of hemolysis. The iron studies, folate and B12 levels, haptoglobin, and Coombs’ test are premature and should be ordered according to results of the PBS review and reticulocyte count.
Question 29
A 24-year-old Lebanese male exchange student comes to the college infirmary with a 3-day history of upper respiratory infection symptoms, cough, purulent sputum, and a low-grade fever. His chest examination is clear, and he is given available trimethoprim-sulfamethoxazole (Bactrim) samples for clinical bronchitis. The following day, he returns with shortness of breath, severe abdominal pain, a high spiking fever, and dark urine. A complete blood count reveals a hemoglobin of 7 g/dL and a white blood cell count of 12,500. Peripheral blood smear has fragmented RBCs, and distinct “bite cells” are present. The chest radiograph is normal. The patient is admitted to the hospital. Which of the following statements is true?
a) The Coombs’ direct test will be positive
b) The haptoglobin will be undetectable
c) A sickle prep screen would be positive
d) All of the above
View Answer




Answer and Discussion
The answer is b.
Objective: Identify glucose-6-phosphate dehydrogenase (G6PD) deficiency as a cause of acute anemia.
This patient has clinical G6PD deficiency with acute hemolysis, as manifested by the acute drop in hemoglobin, dark urine, and fragmentation on the peripheral blood smear. People of Mediterranean descent are more susceptible to rapid severe hemolysis, in contrast to people of African descent. The “bite cells” on the smear are pathognomonic for this condition, which was triggered by the oxidative stress of the sulfa drugs. The precipitating hemoglobin results in RBC stromal damage and acute hemolysis. The haptoglobin level will be low if not undetectable because of its binding to free hemoglobin and removal by the liver. The Coombs’ tests, both direct and indirect, are negative because antibodies are not involved in this physical form of hemolysis. Although many antibiotics might produce immune hemolysis, the time course of acute onset within 24 hours goes against any immune process. The sickle preparation will be negative because the precipitation of hemoglobin results in inclusion bodies but not in polymerization with deformity of the RBC architecture. Sickle cells will not be seen unless this patient also has a hemoglobinopathy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree