Fig. 1.1
Assessment of nadir upper esophageal sphincter relaxation pressure using high-resolution esophageal manometry isobaric contour tool. (a) depicts a patient with normal upper esophageal sphincter relaxation. (b) depicts a patient with abnormal upper esophageal sphincter relaxation with elevated residual pressure. (Adapted by permission from Nature Publishing Group: American Journal of Gastroenterology (Kwiatek MA, Mirza F, Kahrilas PJ, Pandolfino JE. Hyperdynamic upper esophageal sphincter pressure: a manometric observation in patients reporting globus sensation. Am J Gastroenterol 2009; 104(2):289–98), copyright 2009)
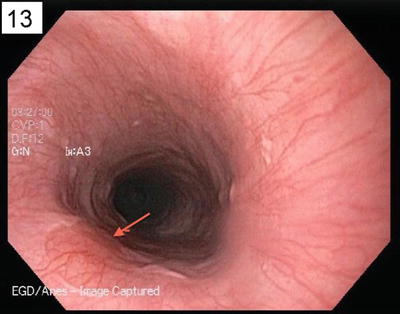
Fig. 1.2
Gastric inlet patch (see arrow) visualized during upper endoscopy which visually is salmon pink in color, reflecting columnar mucosa, with a smooth border and usually round or oval in shape
Several studies have found that patients with globus report an increase in stressful life events prior to the onset of symptoms. One study noted that nearly 96 % of globus patients reported an increase in their symptoms when experiencing strong emotion. This is a rationale for the use of tricyclic antidepressants in those with no structural or motility abnormalities who have not responded to an empiric trial of acid suppressive therapy.
Diagnosis and Evaluation
The Rome III diagnostic criteria for globus (see Table 1.1) require the presence of symptoms for the last 3 months with onset at least 6 months prior to diagnosis. It is important that conditions such as GERD, motility disorders of the esophagus, and structural lesions are ruled out. Table 1.2 highlights a broad differential diagnosis to consider in patients presenting with globus sensation.
Table 1.1
Rome III diagnostic criteria for globus
1. Persistent or intermittent, non-painful sensation of a lump or foreign body in the throat |
2. Occurrence of the sensation between meals |
3. Absence of dysphagia or odynophagia |
4. Absence of evidence that gastroesophageal reflux is the cause of the symptom |
5. Absence of histopathology-based esophageal motility disorders |
Table 1.2
Differential diagnosis in the evaluation of suspected globus
Gastrointestinal disorders | Non-gastrointestinal disorders |
|---|---|
Esophageal dysmotility | Head and neck (particularly tongue) cancer |
Achalasia | Cervical lymphadenopathy |
Gastric inlet patch | Goiter |
GERD | Hyperplastic tonsils |
Esophageal ring or obstructing esophageal lesions | Prior uvulopalatoplasty |
Hiatal hernia | Paraesophageal mass |
Hypertensive upper esophageal sphincter | Chronic tonsillitis or pharyngitis |
Ring or web of cervical esophagus or postcricoid region | Thyroid disease |
Zenker’s diverticulum | Cervical spondylosis/cervical osteophytes |
Stress < div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|




