Fig. 7.1
RoboSurgeon system. Three-dimensional (3D)

Fig. 7.2
Single port and the three-dimensional head-mounted display that all surgeons wear
The RoboSurgeon system consists of three components: a three-dimensional head-mounted display (3D-HMD), handheld robot-like devices, and an endoscope manipulation robot (Fig. 7.1). Part or all of this system is used depending on the situation, but the 3D-HMD, which provides six fields of vision (magnified vision, stereovision, panoramic vision [direct vision], multivision, navigated vision, and shared vision), is always used by surgeons (see Chap. 1).
Gasless single-port RoboSurgeon surgery generally achieves four key “nos”: no high costs, no CO2, no multiple ports, and no intraperitoneal injury. However, as little as possible of the peritoneum is removed in total cystectomy. The adjustable size of the port and direct vision ensure safety and make it easy to learn this procedure (Fig. 7.3) [7]. Prophylactic antimicrobial agents are minimally required in the perioperative period [8–11].
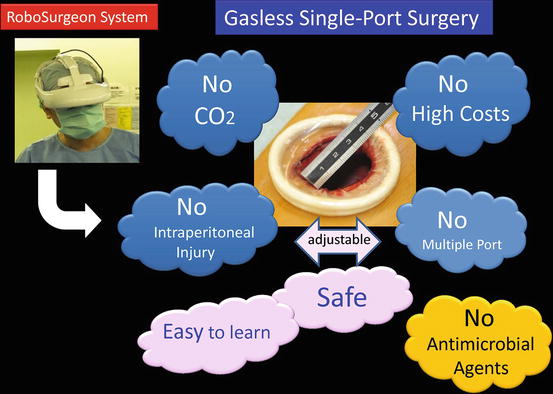
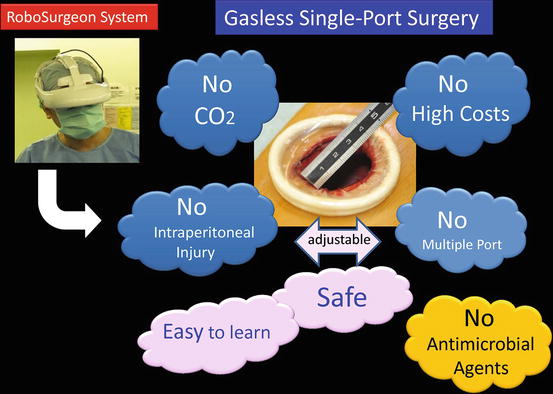
Fig. 7.3
Fundamental concept of gasless single-port RoboSurgeon surgery
If the RoboSurgeon system is not available, gasless single-port-like surgery, in which the port size is somewhat larger, can be performed following the procedures presented here by using a system with an ordinary two-dimensional endoscope and display. The surgical procedures can also be applied to open surgery that utilizes a smaller incision.
This surgery may contribute to overcoming some of the disadvantages of existing laparoscopic as well as robot-assisted minimally invasive surgeries while retaining their major benefits and possibly providing some unique advantages.
7.2 General Concept
In this surgery, most of the procedures are carried out in a wide retroperitoneal working space made along the anatomical plane through a single port, without gas insufflation, and assisted by the RoboSurgeon system, which consists of wearable or head movement-controlled devices. See Chap. 1 for more details.
7.3 Preoperative Preparation
Patients are provided with sufficient information, including the potential need to extend the port size in the event of difficulties, when obtaining informed consent. Prior abdominal surgery, pelvic surgery, or preoperative radiotherapy has not been shown to be contraindicative [12, 13]. Patients receive minimal prophylactic antimicrobial agents in the perioperative period.
7.4 Instruments
This operation is performed mainly using reusable and affordable devices. Disposable devices, a vessel-sealing device and an ultrasonic coagulator, are usually used but can be replaced with ligation and scissors. A catcher to extract the specimen is the only disposable (but affordable) device that is not replaceable. The endoscope manipulation robot that works with air pressure (Aerovision® [initial version], EMARO® [second version], Riverfield, Inc.) can also be replaced by an endoscopist. See Chap. 1 for details.
7.5 Surgical Techniques
7.5.1 Principle
In RoboSurgeon surgery, each surgical team member wears the 3D-HMD (Fig. 7.2). During the operation, the 3D-HMD provides six fields of vision in front of the eyes regardless of head position: magnified vision, stereovision, panoramic vision (direct vision), multivision, navigated vision, and shared vision (see Chap. 1) (Figs. 7.4, 7.5, 7.6, and 7.7). All procedures are carried out through a single port, 4–5 cm in diameter. The port size of TC is fundamentally the largest among our gasless single-port surgeries. A wide pelvic extraperitoneal working space is created by identifying proper planes for cleavage and maintained using long retractors (PLES retractor®, Innomedics Medical Instruments, Inc.) (Fig. 7.8). The use of Thunderbeat® (Olympus Corp.) or LigaSure® (Covidien) facilitates the dissection and reduces intraoperative blood loss. Soft coagulation (VIO300D; Erbe Elektromedizin GmbH) is applied in order to stop bleeding caused by protein degeneration due to Joule heat. This mechanism enables soft coagulation to generate hemostasis securely without vessel wall damage, and it prevents fistula formation.

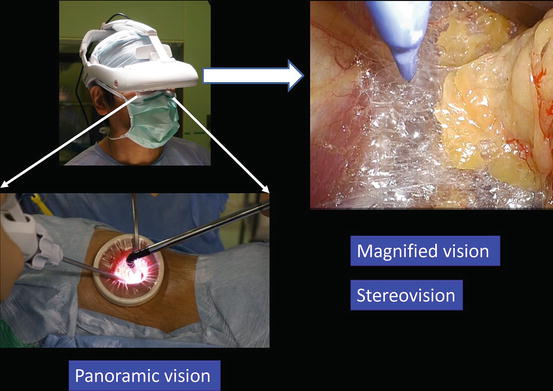
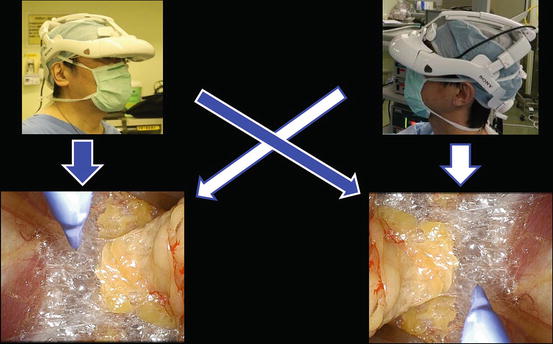
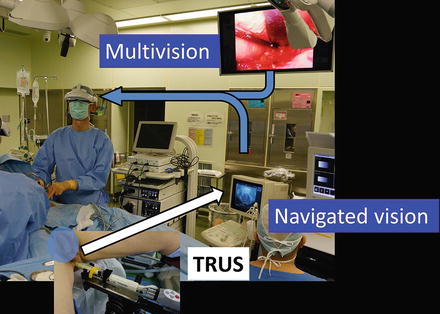

Fig. 7.4
3D-HMD provides six fields of vision in front of the eyes regardless of head position
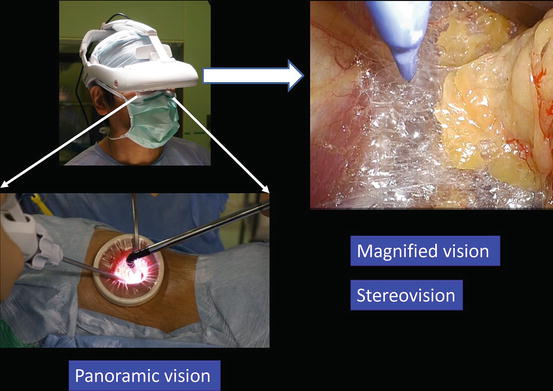
Fig. 7.5
Magnified vision, stereovision, and panoramic vision are obtained. A wide panoramic view can be seen by moving the angle of sight downward
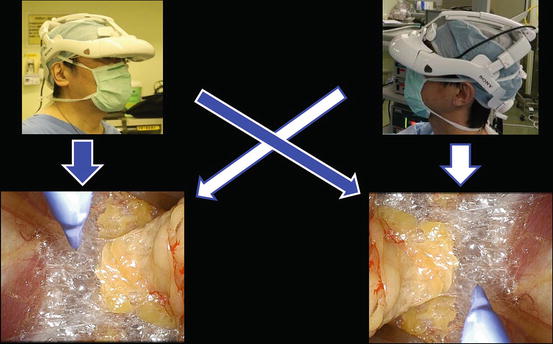
Fig. 7.6
Each surgeon can change the direction of the images on the display according to his or her position
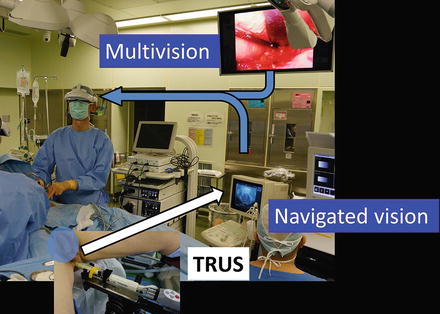
Fig. 7.7
Multivision and navigated vision from transrectal ultrasonography (TRUS)
Fig. 7.8
Working space created through a single port
Representative scenes of extraction of the bladder with prostate and urethra en bloc through the single port, which permits narrow extraction of the specimen, are presented in Fig. 7.9.
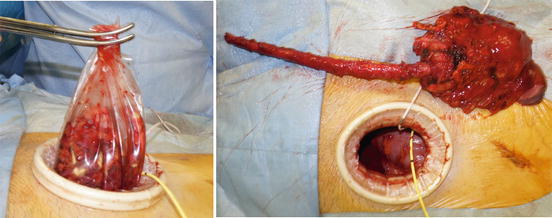
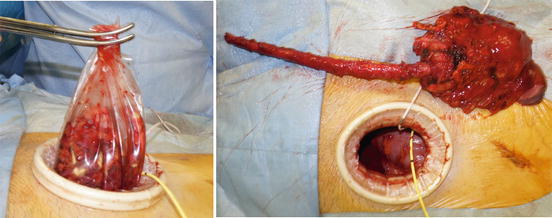
Fig. 7.9
Extraction of the bladder with the prostate and the urethra through a single port
7.5.2 Flowchart of the Procedure
A flowchart of the procedure in male total cystectomy is shown in Fig. 7.10.
Fig. 7.10
Flowchart of the procedure
7.5.3 Patient Positioning
The surgery is performed under general anesthesia. The patient is placed in a supine and lower lithotomy position to allow simultaneous urethrectomy. The upper limbs are positioned alongside the body to avoid the risk of stretch injuries to the brachial plexus.
The operating table is tilted head down, and the patient is placed in an extended Trendelenburg position. A nasogastric catheter is positioned by the anesthesiologist, and the stomach is decompressed. An 18 Fr Foley catheter with 10 ml in the balloon is introduced after the placement of the sterile drapes (Fig. 7.11).


Fig. 7.11
Patient position and single port
The assistant is located opposite the lead surgeon. The endoscope manipulation robot or an endoscopist is positioned between the legs or opposite the lead surgeon (Fig. 7.12). The lead surgeon facing the endoscopist uses the reversed image of the endoscope on his or her HMD. The multiple-imaging information, which includes an endoscopic view and a transrectal ultrasound image, can be simultaneously displayed on the HMD as a composite image using a four-split or two-split screen or a picture-in-picture feature. If needed, the HMD wearer can use this integrated information through the HMD (Figs. 7.13 and 7.14).
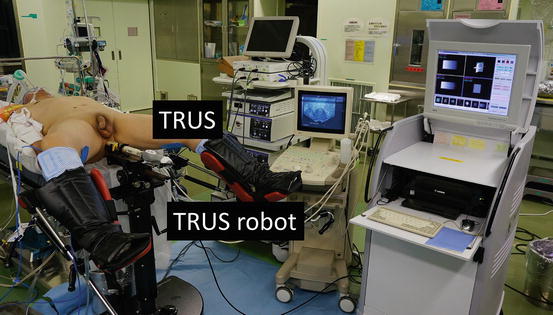
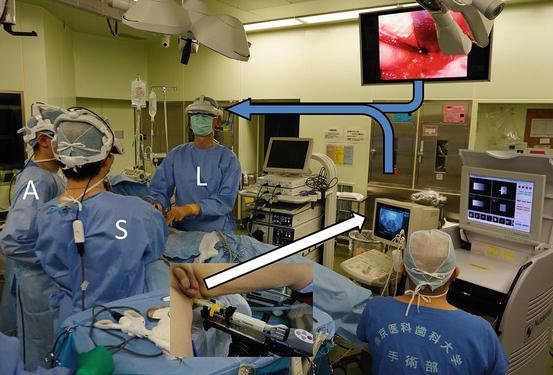
Fig. 7.12
Surgical hand washing and surgeon’s position. The endoscope is held by a robot or endoscopist
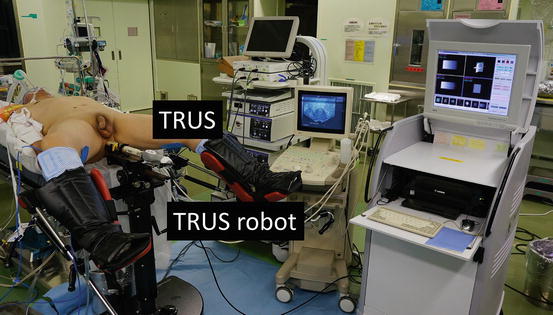
Fig. 7.13
Patient position and transrectal ultrasonography (TRUS) controlled by a robot
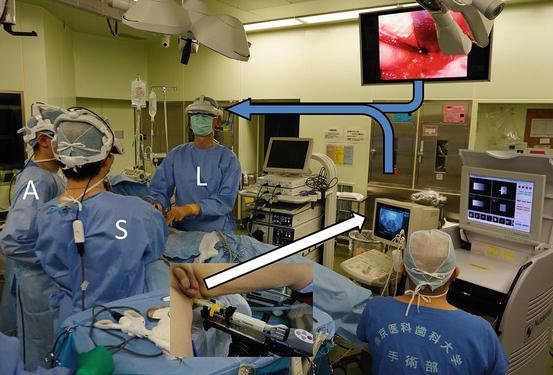
Fig. 7.14
Endoscope and transrectal ultrasound images displayed for each surgeon in a three-dimensional head-mounted display utilizing a picture-in-picture format. Lead surgeon (L); assistant (A); endoscopist (S)
7.5.4 Port Placement
A skin incision of approximately 5 cm in length is made in the midline of the lower abdomen. The retroperitoneal space is opened by incising the transversal fascia covering the fatty tissue. The exposed spermatic cord and vas deferens are dissected (Fig. 7.15). After widely opening the pelvic spaces bilaterally alongside the bladder, a single port of around 4–5 cm is made using a wound retractor (Alexis wound retractor®, Applied Medical Resources, Corp.) (Fig. 7.11).
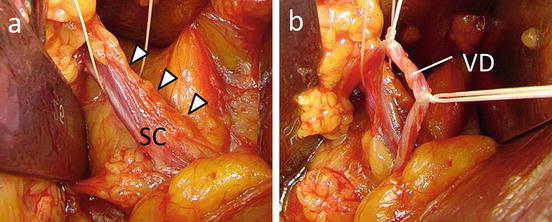
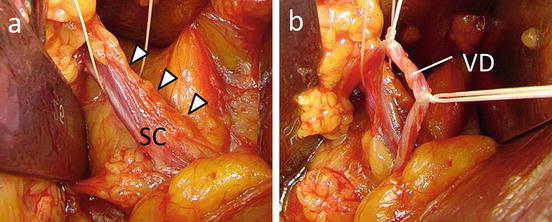
Fig. 7.15
(a) Exposing the spermatic cord (SC). (b) Vas deferens (VD)
Tip Plane dissection is essential for creating and maintaining a working space in the retroperitoneal space without CO2 insufflation. The vas deferens is held for the later dissection between the bladder and the peritoneum.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








