Fig. 6.1
RoboSurgeon system. Three-dimensional (3D)

Fig. 6.2
Single-port and 3D head-mounted display that all surgeons wear
Fig. 6.3
Fundamental concept of gasless single-port RoboSurgeon surgery
Fig. 6.4
3D-HMD provides six fields of vision in front of the eyes regardless of head position
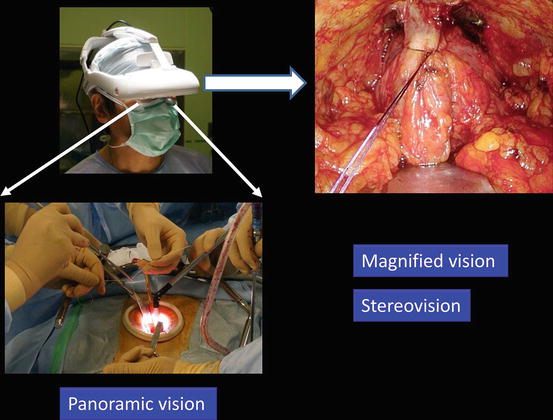
Fig. 6.5
Magnified vision, stereovision, and panoramic vision are obtained. A wide panoramic view is seen by moving the angle of sight downwards
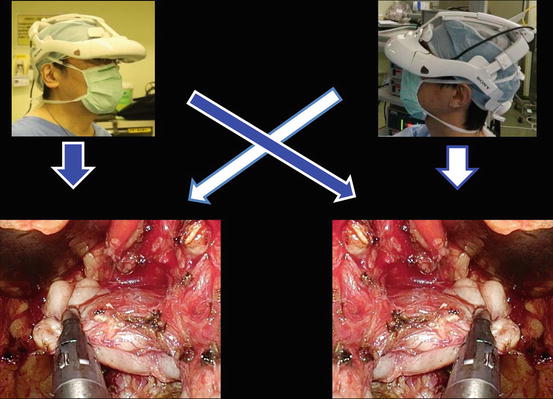
Fig. 6.6
Each surgeon can change the direction of the images on the display according to his or her position
Fig. 6.7
Navigated vision using transrectal ultrasonography for intrapelvic-organ surgeries. Ultrasonography (US)
Fig. 6.8
Working space for intrapelvic operations
In the gasless single-port RoboSurgeon radical prostatectomy, all procedures are carried out extraperitoneally through a single port of around 4 cm in diameter [8]. An extraperitoneal approach avoids the potential disadvantages associated with a transperitoneal approach. Since the peritoneal cavity remains intact, intraperitoneal injury such as intestinal injury, intraperitoneal bleeding, or postoperative intestinal obstruction is almost nonexistent.
The RoboSurgeon system consists of three components: a three-dimensional (3D) head-mounted display (HMD), handheld robot-like devices, and an endoscope manipulation robot (Fig. 6.1). Part or all of this system is used depending on the situation, but the 3D-HMD, which provides six fields of vision (magnified vision, stereovision, panoramic vision, multivision, navigated vision, and shared vision), is always used by surgeons (Fig. 6.2). All of the members of the surgical team can see the magnified and clear operative field of view, which allows the surgeon to carry out complicated maneuvers around the prostate throughout the entire operation.
This surgery leads to four key “no’s”; no high costs, no CO2, no multiple ports, and no intraperitoneal injury. The adjustable size of the port ensures safety and makes it easy to learn the procedure (Fig. 6.3) [9, 10]. The requirement of prophylactic antimicrobial agents is minimal, one single dose orally, in the perioperative period [11–14].
If the RoboSurgeon system is not available, gasless single-port-like surgery, in which the port size is somewhat larger, can be performed following the procedures presented here using a system with an ordinary two-dimensional endoscope and display [9, 10].
This surgery may help surgeons overcome some of the disadvantages of existing laparoscopic and robotic minimally invasive surgeries while retaining their major benefits and may add some unique advantages.
6.2 General Concept
A wide extraperitoneal working space is made along the anatomical plane in the pelvis without gas insufflation (Fig. 6.8), and the surgeon is assisted by the RoboSurgeon system that consists of wearable or head movement-controlled devices. For more details, see Chap. 1, Fundamentals of Gasless Single-Port RoboSurgeon Surgery.
6.3 Preoperative Preparation
Sufficient informed consent of the patient is necessary, including the potential need to extend the incision. Preoperative risk assessment of prostate cancer is essential for patient-tailored radical prostatectomy. Whether to carry out pelvic lymph node dissection and/or nerve sparing is decided before the operation. Prediction of extraprostatic extension and lymph node metastasis based on preoperative clinical variables is useful in the decision-making process [15, 16].
6.4 Instruments
This operation can be performed with reusable and affordable devices. Disposable devices, such as a vessel-sealing device, are usually used but can be replaced with ligation and scissors. The endoscope manipulation robot working with air pressure (Aerovision® [initial version], EMARO® [second version], Riverfield, Inc.) can also be replaced by an endoscopist. See Chap. 1 for details.
6.5 Surgical Techniques
6.5.1 Fundamental Procedures
All of the surgeons wear the 3D-HMD (Fig. 6.2). During the operation, the 3D-HMD provides six fields of vision in front of the eyes regardless of head position: magnified vision, stereovision, panoramic vision (direct vision), multivision, navigated vision, and shared vision (Fig. 6.4). Using the direct vision obtained by moving the angle of sight downward, the surgeons receive instruments from the scrub nurse as well as observe the operative field to ensure safety (Fig. 6.5). Each surgeon can change the direction of the images on the display according to his or her position, which makes it possible to share a common direction (Fig. 6.6). Multivision, including navigated vision using transrectal ultrasonography, can be employed if necessary (Figs. 6.6 and 6.7).
Through a single port, the surgeon initially inserts all instruments, including the endoscope, using direct vision and then follows them on the 3D-HMD.
The working space for the intrapelvic operations is created by dissecting along the steric connective tissue covering the perivesical fatty tissue (Fig. 6.8).
6.5.2 Flowchart of the Procedure
A flowchart of the procedure is shown in Fig. 6.9. A view showing a frame format of the procedure is shown in Fig. 6.10.
Fig. 6.9
Flowchart of procedures
Fig. 6.10
A view showing a frame format of procedures: (1) isolation from the levator ani, (2) freeing from the dorsal vein complex, (3) separation from the bladder neck, (4) isolation from the rectum, (5) separation from the urethra, and (6) anastomosis between the urethra and the bladder neck. Dorsal vein complex (DVC); seminal vesicle (SV)
6.5.3 Patient Positioning
The patient is placed in the supine position with the lower limbs not arranged in an abducted position. The operation is performed in a 20° Trendelenburg position with extension of the lumbar. The upper limbs are positioned alongside the body to avoid risk of stretch injuries to the brachial plexus and to allow for free movements of the operating team. Shoulder support is provided for the Trendelenburg position. Both arms are positioned closely against the body and fixed by evacuating the appropriately adjusted vacuum mattress (Fig. 6.11). A Foley catheter is introduced after the placement of the sterile drapes. The lead surgeon operates from the patient’s left side, and the first assistant and the endoscopist are placed opposite the lead surgeon. If there is a second assistant (a fourth participant in the surgery), he or she is placed at the lead surgeon’s side. Each surgical team member wears a 3D-HMD (Fig. 6.12). Participants facing the endoscopist use the reversed images of the endoscope on their 3D-HMDs.


Fig. 6.11
(a) Patient position. (b) Shoulder support
Fig. 6.12
Surgeon’s position. Endoscope is held by an endoscopist or a robot
Tip In patients for whom the Trendelenburg position is unsuitable, such as patients with glaucoma or cerebral vascular disease, the operation is performed in the supine position. Flexibility in the operative position is one of the advantages of this operation.
Tip If transrectal ultrasound is used for monitoring the operative field, the lithotomy position is preferable.
6.5.4 Skin Incision-Port Placement
A minimum incision (around 4–5 cm) near the size of the prostate is made in the midline of the lower abdomen, and the rectus muscles are split in the midline. The transversal fascia is incised, and a wide working space in the pelvis is provided by mobilizing the bladder medially and the peritoneum cranially using a PLES retractor® or PLES spatula® (Innomedics Medical Instruments, Inc.). This mobilization is carried out until the external iliac vein and spermatic cord with the vas deferens (adjacent to the inguinal ring) are observed. After bilateral working spaces are created in the pelvis, a single port is prepared through the positioning of a wound retractor (S- or M-sized ALEXIS® wound retractor, Applied Medical Resources, Corp.) (Fig. 6.13).
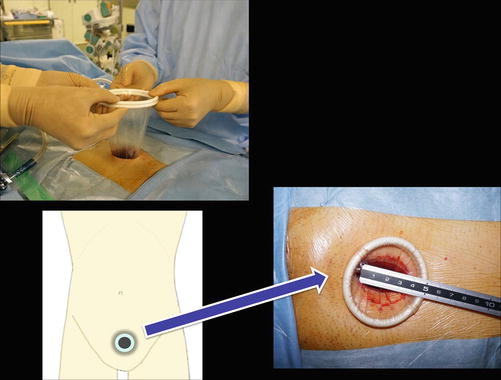
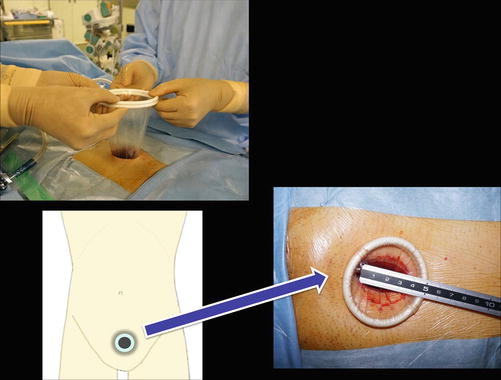
Fig. 6.13
Preparation of a single port
Pelvic lymph node dissection (PLND) is usually carried out for intermediate- or high-risk prostate cancer after port placement (see Chap. 9). A hernia prevention procedure is considered for patients who wish to prevent postoperative indirect hernias (see Chap. 9).
Tip A transverse lower abdominal incision whose postoperative scar is unnoticeable is also an option.
6.5.5 Isolation of the Lateral Prostatic Fascia
The fatty tissue around the prostate is removed to better see the anatomical planes. To preserve the lateral aspects of the prostatic fascia, the fusion line between the fascia on the prostate side and the fascia on the levator ani side after opening the thin fascia (the so-called endopelvic fascia) is carefully observed at the level of the bladder neck (Fig. 6.14), and the above two fasciae are gently separated from the level of the bladder neck to the periurethral muscle. In most cases, a portion of the levator ani is attached or fused to the fascia on the prostate side near the prostate apex. Some investigators call this portion of the levator ani “the pubococcygeus muscle” (Fig. 6.15a). The pubococcygeus muscle is cut using a vessel-sealing device such as LigaSure® (Covidien Ltd.) or Thunderbeat® (Olympus, Ltd.) (Fig. 6.15b). After this procedure, the entire puboprostatic ligament usually comes into focus. The puboprostatic ligament is usually spared by cutting it at its attachment to the prostatic apex. For surgical maneuvers around the prostate, a flexible 3D endoscope is usually positioned at the caudal edge of the single port and used with its endpiece flexed (Fig. 6.15c). The 3D-HMD system displays multiple forms of information as integrated, sharp, high-contrast images using a four-split or two-split screen or a picture-in-picture feature both seamlessly and synchronously. Using this function, simultaneous monitoring of the operative field along with transrectal ultrasonography is possible (Figs. 6.16 and 6.17).
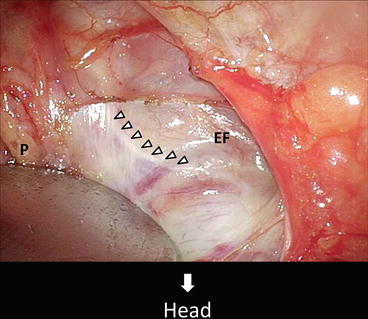
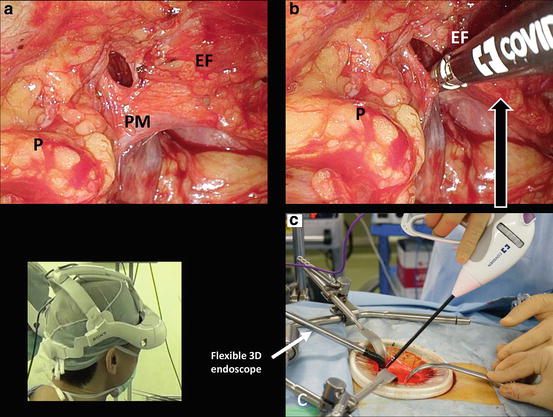
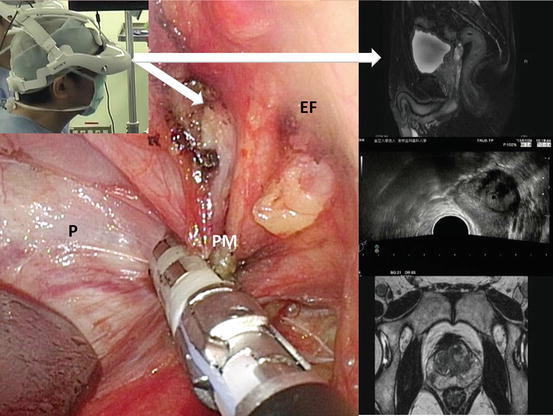




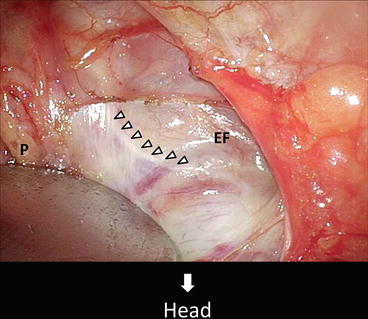
Fig. 6.14
Fusion line between the fascia on the prostate side and the fascia on the levator ani side. Endopelvic fascia (EF); prostate (P)
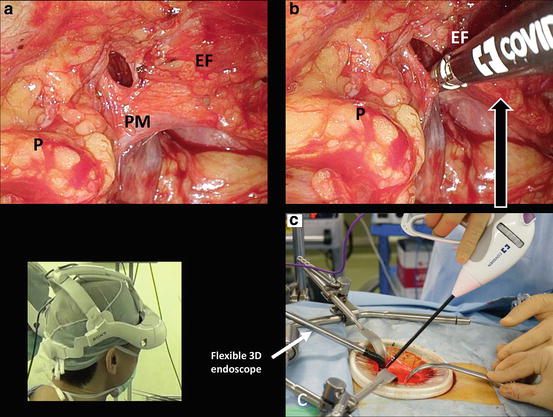
Fig. 6.15
(a) Pubococcygeus muscle (PM). (b) Vessel-sealing device is useful for resection of the PM. (c) Flexible 3D endoscope can be positioned at the caudal edge of the single port and used with its endpiece flexed. Prostate (P); endopelvic fascia (EF)
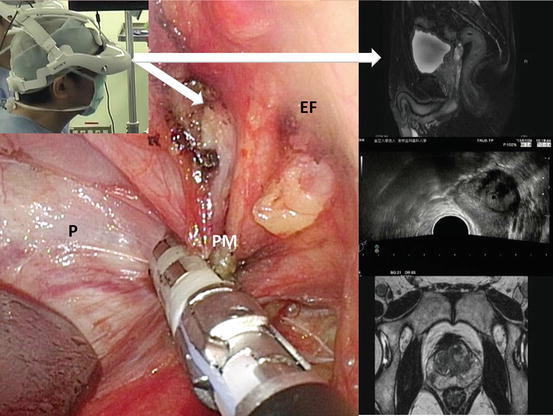
Fig. 6.16
Resection of the pubococcygeus muscle (PM). A four-split screen displayed on HMD. Prostate (P); endopelvic fascia (EF)
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








