Fig. 9.1
RoboSurgeon system. Three dimensional (3D)

Fig. 9.2
Single port and the 3D head-mounted display that all surgeons wear
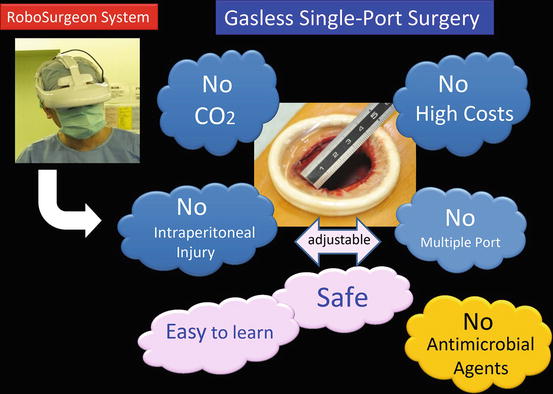
Fig. 9.3
Fundamental concept of gasless single-port RoboSurgeon surgery
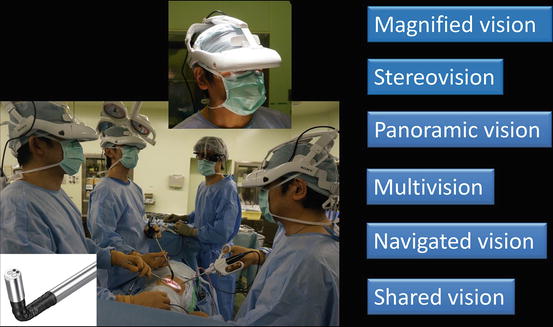
Fig. 9.4
The 3D-HMD provides six fields of vision in front of the eyes regardless of head position
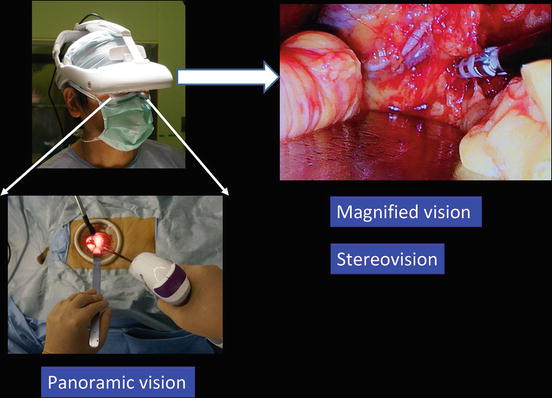
Fig. 9.5
Magnified vision, stereovision, and panoramic vision are obtained. A wide panoramic view can be seen by moving the angle of sight downward
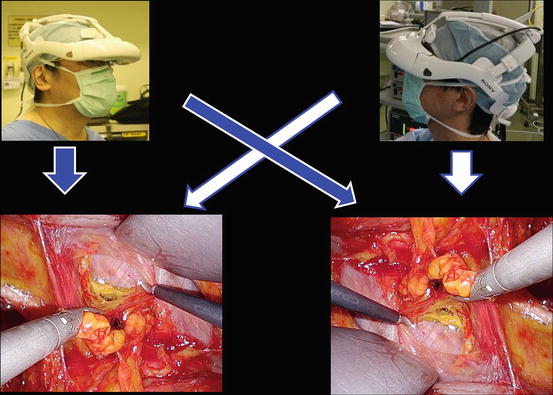
Fig. 9.6
Each surgeon can change the direction of the images on the display according to his or her position
This surgery achieves four key “no’s”: no high costs, no CO2, no multiple ports, and no intraperitoneal injury (Fig. 9.3). The adjustable size of the port ensures safety and makes it easy to learn this procedure [5]. In this chapter, the surgical techniques of pelvic lymph node dissection and inguinal hernia prevention are described. These procedures can be performed similarly through a somewhat larger port without the RoboSurgeon system.
9.2 Instruments
Reusable and affordable devices are mainly used. The endoscope manipulation robot can be replaced by an endoscopist. See Chap. 1 for details.
9.3 Pelvic Lymph Node Dissection
9.3.1 Principle
General indications for pelvic lymph node dissection in routine urologic practices include intermediate- and high-risk prostate cancer patients undergoing radical prostatectomy and bladder cancer patients undergoing partial/radical cystectomy [6]. The primary role of pelvic lymph node dissection for prostate and bladder cancers is in the staging procedure that provides information on prognosis (e.g., the number of lymph nodes involved). Besides this staging procedure, a number of studies support its therapeutic role; pelvic lymph node dissection can be curative in a subset of patients with limited lymph node metastases for both prostate and bladder cancers [7–11]. Extents of pelvic lymph node dissection in our practice include obturator, external, and internal iliac regions for intermediate- and high-risk prostate cancer and obturator, external, internal, and distal common iliac and presacral regions for muscle-invasive bladder cancer.
9.3.2 Preoperative Preparation and Patient Positioning
This procedure is usually performed at the time of radical prostatectomy and radical/partial cystectomy. Preoperative preparation and patient positioning of pelvic lymph node dissection conforms to those of radical prostatectomy (see Chap. 6), radical cystectomy (see Chap. 7), and partial cystectomy (see Chap. 8).
9.3.3 Surgical Techniques
The surgical field for pelvic lymph node dissection is fixed using the Omni-Tract self-retractor system to displace the peritoneum upward and the bladder medially and to maintain the round shape of the single port (Figs. 9.7 and 9.8). All of the surgical procedures are performed under magnified stereovision on the 3D-HMD by all participants (Fig. 9.9). For right pelvic lymph node dissection, a right-handed lead surgeon stands on the left side of the patient and an assistant and an endoscopist stand on the opposite side (Fig. 9.9). When an endoscope is inserted from the opposite side of the lead surgeon, the surgeon rotates the images on the 3D-HMD 180° to obtain the orthoscopic images.
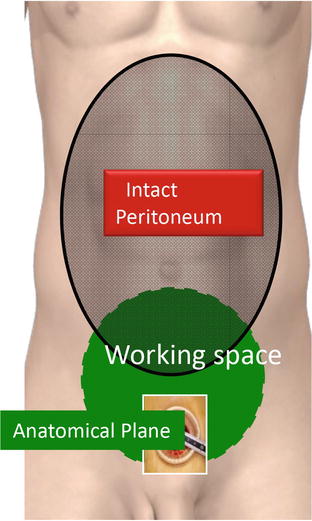
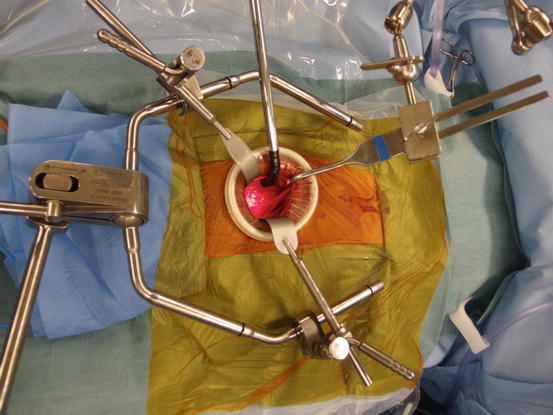
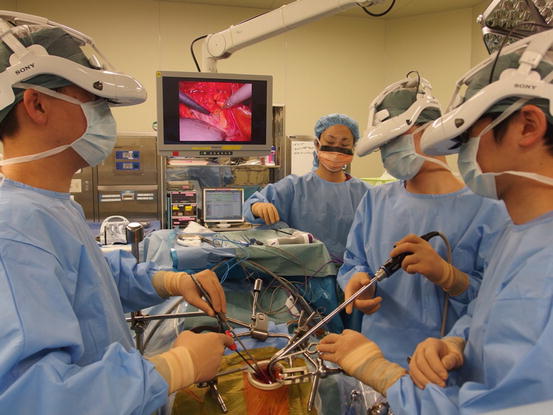
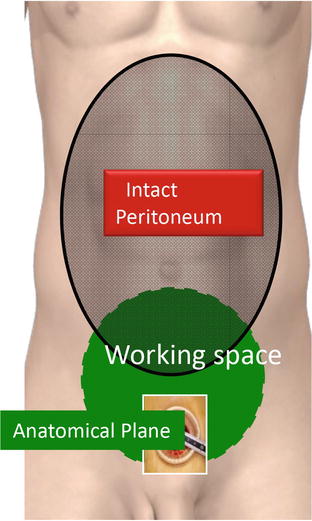
Fig. 9.7
Working space created through a single port
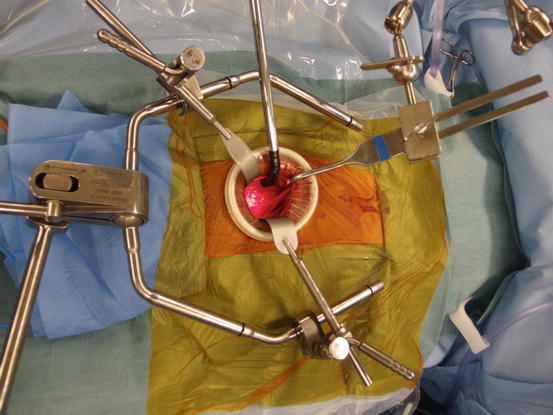
Fig. 9.8
Panoramic view of the single port
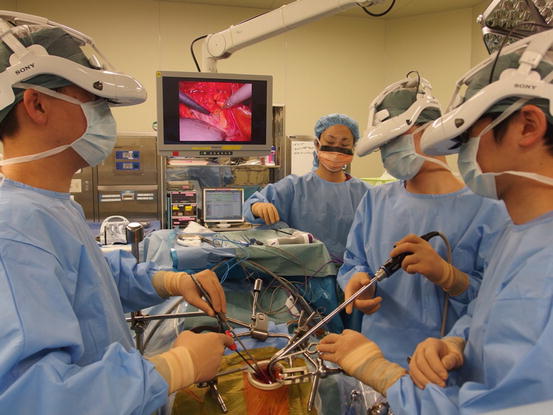
Fig. 9.9
View of the RoboSurgeon gasless single-port pelvic lymph node dissection
9.3.4 Single Port in the Lower Abdomen
The size of the single port necessary for pelvic lymph node dissection is 2–3 cm in diameter. However, this procedure is usually performed simultaneously with radical prostatectomy and radical/partial cystectomy. In our practice, the diameters of the single ports for radical prostatectomy, partial cystectomy, and radical cystectomy are usually 4 cm, 3–4 cm, and 5–6 cm, respectively. To create a single port, a lower abdominal vertical skin incision of corresponding length (e.g., 4.5 cm for radical prostatectomy) is made. The Retzius space is opened by dissecting the peritoneum upward using a long retractor (PLES retractor®, Innomedics Medical Instruments, Inc.). Once the Retzius space is opened bilaterally, a wound retractor (Alexis wound retractor®, Applied Medical Resources, Corp.) is positioned so as to make a single port (Fig. 9.8).
9.3.5 Dissection of the External Iliac and Obturator Lymph Node Packet
The sheath of the external iliac vein is incised along the vein from the femoral canal to the bifurcation of the common iliac artery (Fig. 9.10). The external iliac vein is then lifted up with a vessel retractor to facilitate the incision of the connective tissue covering the obturator internus muscle (Fig. 9.11). The connective tissue is dissected from the fascia of the obturator internus muscle to the bottom of the obturator fossa to create the lateral border of the obturator lymph node packet (Fig. 9.12). Following identification of the obturator nerve, a right-angle clamp is passed through the obturator lymph node packet just above the obturator nerve, and the lymph node packet is ligated with a 1–0 silk to facilitate the obturator lymph node dissection (Fig. 9.13). The obturator lymph node packet is dissected distally to the femoral canal to doubly clip and divide the distal end of the lymphatic chain with a sealing device (Fig. 9.14). The obturator lymph node packet is dissected cranially along the obturator nerve (Fig. 9.15) to the internal iliac artery (Fig. 9.16) and vein (Fig. 9.17) near its cranial border. Finally, the cranial end of the lymphatic chain is dissected and divided dorsally to the common iliac vein using a sealing device (Fig. 9.18).

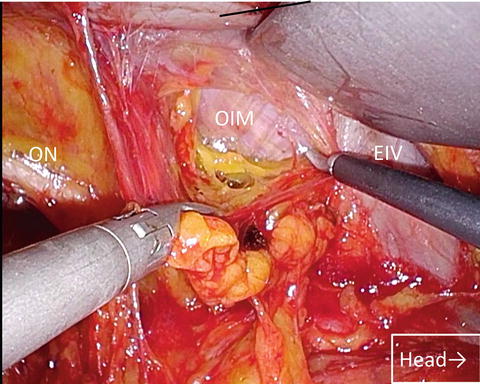
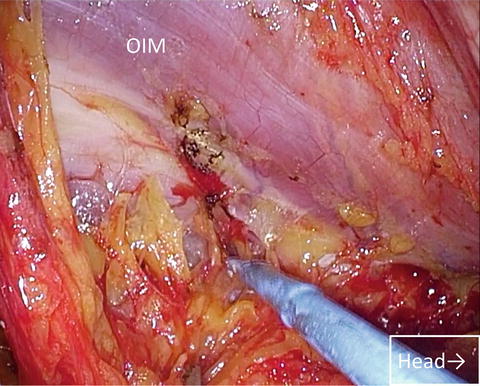
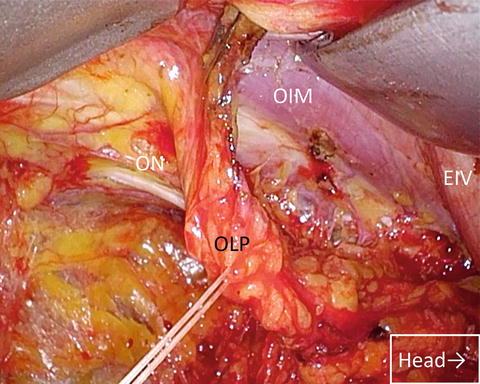
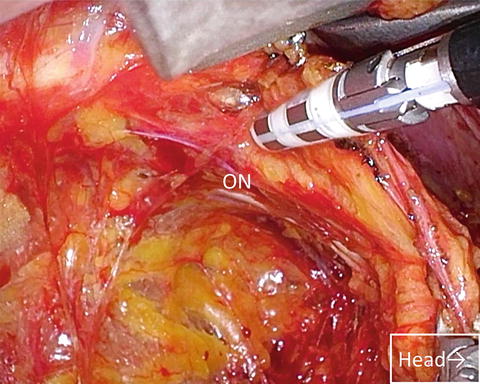
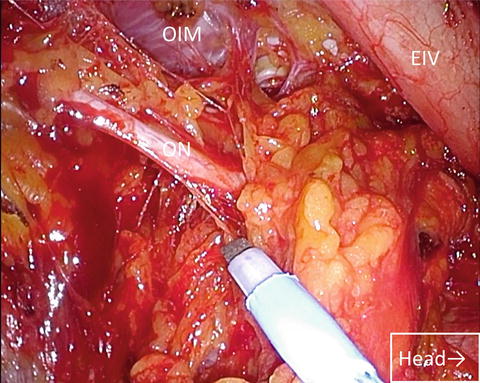





Fig. 9.10
Incision of the sheath of right external iliac vein. External iliac vein (EIV); external iliac artery (EIA)
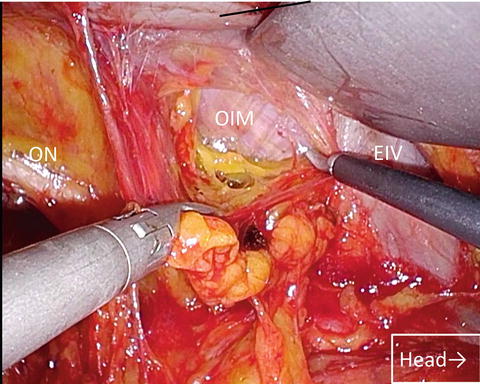
Fig. 9.11
Exposure of the fascia of the obturator internus muscle. Obturator internus muscle (OIM); obturator nerve (ON)
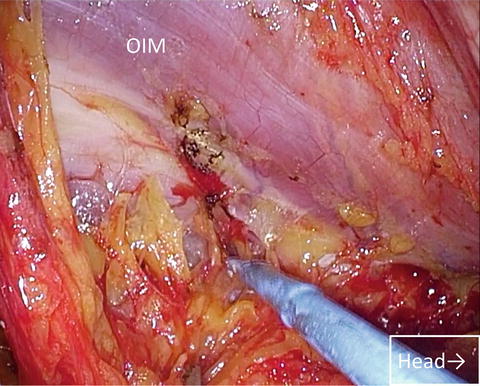
Fig. 9.12
Outer dissection of the obturator lymph node packet down to the bottom of the obturator fossa
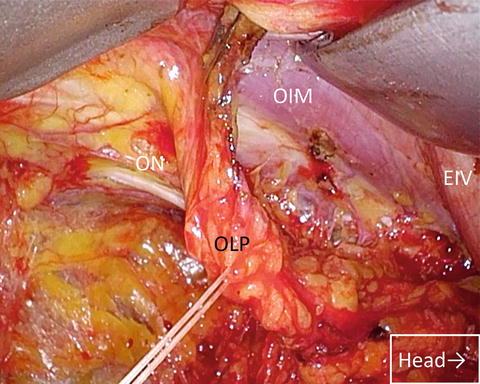
Fig. 9.13
Ligation of the obturator lymphatic packet to facilitate its dissection. Obturator lymph node packet (OLP)
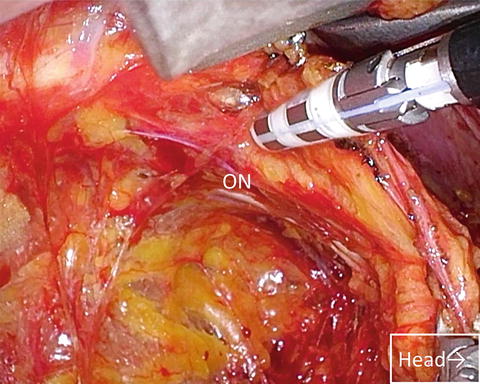
Fig. 9.14
Dividing the distal lymphatic vessels of the obturator lymph node packet using the sealing device after double clipping
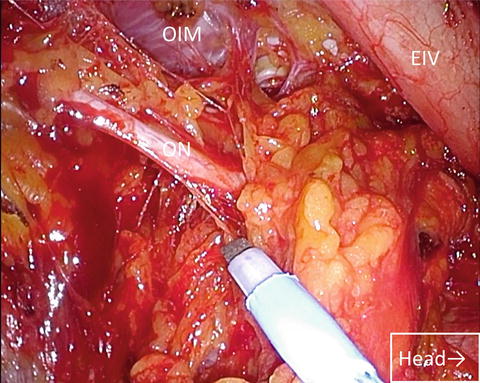
Fig. 9.15
Cranial dissection of the obturator lymph node packet along the obturator nerve
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








