Fig. 5.1
RoboSurgeon system. Three dimensional (3D)

Fig. 5.2
Single port and three-dimensional head-mounted display that all surgeons wear
Fig. 5.3
Fundamental concept of gasless single-port RoboSurgeon surgery
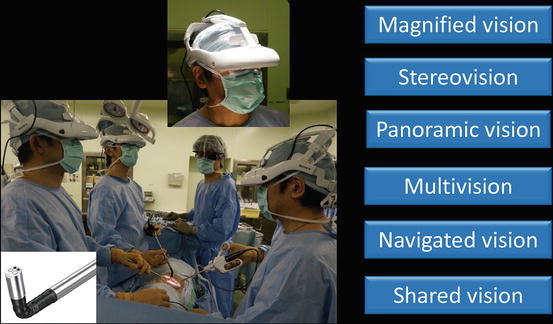
Fig. 5.4
3D-HMD provides six fields of vision in front of the eyes regardless of head position
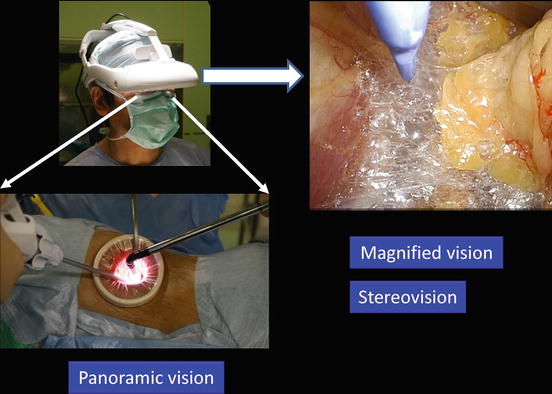
Fig. 5.5
Magnified vision, stereovision, and panoramic vision are obtained. A wide panoramic view can be seen by moving the angle of sight downward
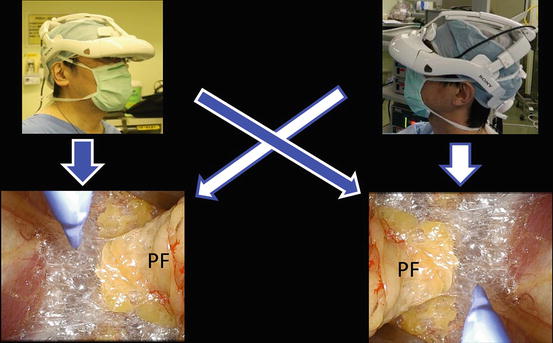
Fig. 5.6
Each surgeon can change the direction of the images on the display according to his or her position. Perinephric fat (PF)
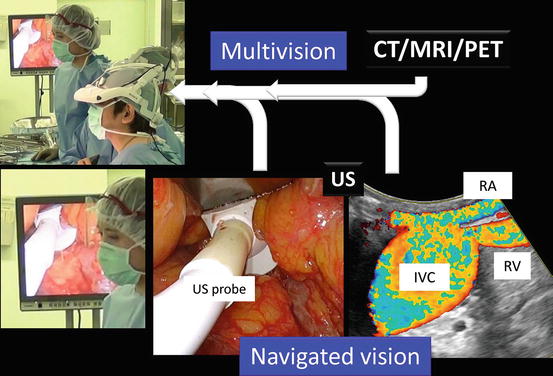
Fig. 5.7
Multivision and navigated vision using ultrasonography via the port. Computed tomography (CT), magnetic resonance imaging (MRI), positron emission tomography (PET), renal artery (RA), renal vein (RV), ultrasound (US), inferior vena cava (IVC)
Fig. 5.8
Working space created through a single port
The RoboSurgeon system consists of three components: a three-dimensional (3D) head-mounted display (3D-HMD), handheld robot-like devices, and an endoscope manipulation robot that works using air pressure (Aerovision® [initial version], EMARO® [second version], Riverfield, Inc.) (Fig. 5.1). Depending on the patient, part or all of this system is used, but the 3D-HMD, which provides six fields of vision (to be hereinafter described), is always used by surgeons. Gasless single-port RoboSurgeon retroperitoneoscopic adrenalectomy achieves four key “no’s”: no high costs, no CO2, no multiple ports, and no intraperitoneal injury. The adjustable size of the port provides safety and makes it easy to learn the procedure (Fig. 5.3). Prophylactic antimicrobial agents are unnecessary in the perioperative period [7–10]. If a RoboSurgeon system is not available, gasless single-port-like adrenalectomy, in which the port size is somewhat larger, can be performed by following the procedures presented herein and using a system with an ordinary two-dimensional endoscope and display [11, 12].
This surgery may help the surgeon overcome some of the disadvantages of current minimally invasive surgeries while retaining their major benefits and adding some unique advantages [13].
5.2 General Concept
In this RoboSurgeon retroperitoneoscopic adrenalectomy, all procedures are carried out extraperitoneally through a coin-sized single port [14–16]. The peritoneal cavity remains intact. Surgeons obtain an operating field large enough for manipulations deep in the wound by identifying proper planes for cleavage without gas insufflation. The endoscopic view allows surgeons and assistants to identify the fine structures of the adrenal gland and surrounding tissues and guides surgical maneuvers throughout the entire operation. For more details, see Chap. 1, Fundamentals of Gasless Single-Port RoboSurgeon Surgery.
In cases with large pheochromocytoma, however, transperitoneal adrenalectomy that preserves muscles can be selected.
5.3 Preoperative Preparation and Choice of Surgical Approaches
Preoperative endocrinological functions are fully examined, and tumor localization is assessed using computed tomography or magnetic resonance imaging. Various types of adrenal tumors can be removed using a retroperitoneal approach, including primary aldosteronism, Cushing’s syndrome, pheochromocytoma, non-functioning cortical adenoma, adrenocortical cancer, and tumor metastatic to the adrenal gland. A transperitoneal approach is preferable for large pheochromocytomas and malignant tumors suspected of invasion to the surrounding tissue.
Patients are provided with sufficient information, including the potential need to extend the port size in the event of difficulties, when obtaining informed consent.
5.4 Instruments
This operation can be performed with reusable and affordable devices. Disposable devices (a vessel-sealing device and an ultrasonic coagulator) are usually used but can be replaced with ligation and scissors. The endoscope manipulation robot that works with air pressure (Aerovision® [initial version], EMARO® [second version], Riverfield, Inc.) can also be replaced by an endoscopist. See Chap. 1 for details.
5.5 Surgical Techniques
5.5.1 Fundamental Procedures
All surgeons wear the 3D-HMD and obtain images in the following manner. During the operation, the 3D-HMD provides the following six fields of vision in front of the eyes regardless of head position: magnified vision, stereovision, panoramic vision (direct vision), multivision, navigated vision, and shared vision (Fig. 5.4). Using the direct vision obtained by moving the angle of sight downwards, surgeons can receive instruments from the scrub nurse and can also observe the operative field to improve safety. Through a single port, the surgeon initially inserts all instruments, including the endoscope, using direct vision and then follows them on the 3D-HMD (Fig. 5.5). Each surgeon can change the direction of the images on the 3D-HMD according to his or her position, which makes it possible to share a common direction (Fig. 5.6). Multivision, including navigated vision using ultrasonography via the port, can be employed if necessary (Fig. 5.7).
A wide extraperitoneal working space is made by dissecting along the steric connective tissue between the perinephric fat and the quadratus lumborum muscle posteriorly and between the perinephric fat and the peritoneum anteriorly (Fig. 5.8). In the wide working space developed in the retroperitoneum, the following procedures are performed. Representative images of extraction of the adrenal gland through the single port, which permits narrow extraction of the specimen, are presented in Fig. 5.9.
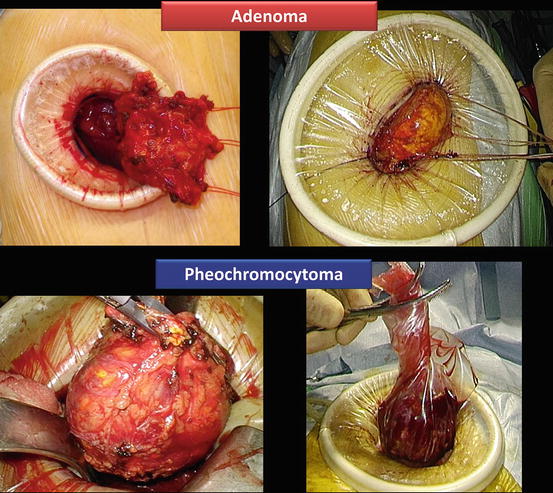
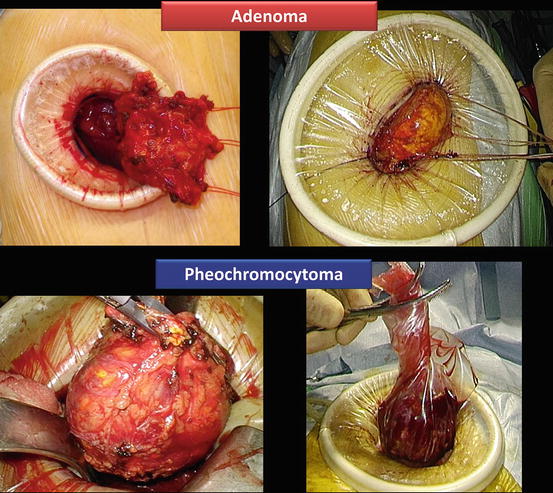
Fig. 5.9
Extraction of adrenal gland through a single port
5.5.2 Flowchart of the Procedures in Retroperitoneoscopic Adrenalectomy
A flowchart of the procedures is shown in Fig. 5.10.
Fig. 5.10
Flowchart of gasless single-port RoboSurgeon retroperitoneoscopic adrenalectomy
5.5.3 Patient Positioning and Preparation
After the provision of general anesthesia, the patient is placed in the flank position over the break of the operating table and a pillow. An axillary roll is placed so as to prevent brachial plexus injury. The patient is held in position using padding and tape at the dorsum, buttocks, and pubis (Fig. 5.11).
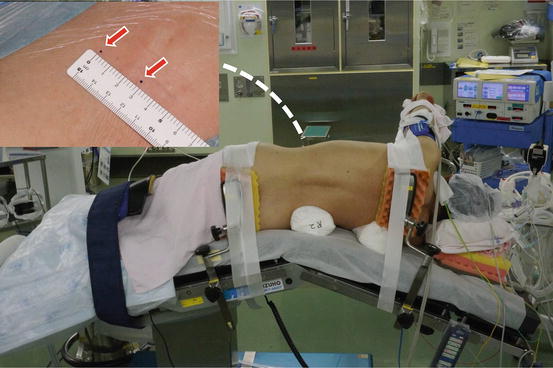
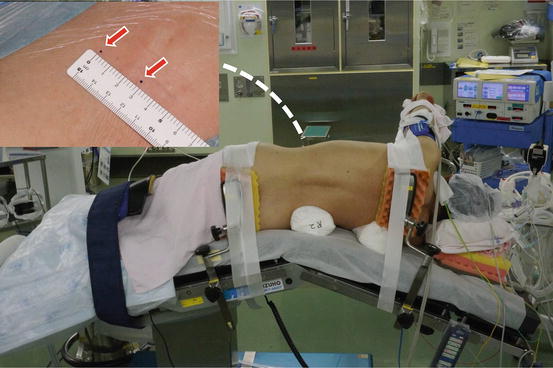
Fig. 5.11
Patient position and skin incision site
Each surgeon puts on the 3D-HMD. The lead surgeon operates from the dorsal side of the patient, and the first assistant is placed at the abdominal side. An endoscope manipulation robot or an endoscopist is placed caudally to the lead surgeon or the first assistant (Fig. 5.12). Surgical team members facing the endoscopist use reversed images of the endoscope on their 3D-HMDs.
Fig. 5.12
Positioning of surgical team members and site of single port in retroperitoneoscopic right adrenalectomy. An endoscope is held by an endoscope manipulation robot or an endoscopist. The second assistant is not indispensable. Lead surgeon (LS), first assistant (A 1 ), endoscopist or endoscope (E), second assistant or resident (A 2 ), nurse (N), PLES retractor® (Pr), PLES spatula® (Ps)
5.5.4 Access to the Retroperitoneal Space
A skin incision of 3–4 cm in length is made in the flank, running obliquely on the distal end of the 12th rib (Fig. 5.13a). The size of the incision depends on the size of the tumor. The tip of the 12th rib is dissected off its bed and slightly shaved if needed (Fig. 5.13b). After the oblique muscles are split, the retroperitoneal space is opened by incising the transversus abdominis aponeurosis, transversal fascia, flank pad, and lateroconal fascia (Fig. 5.13c, d).
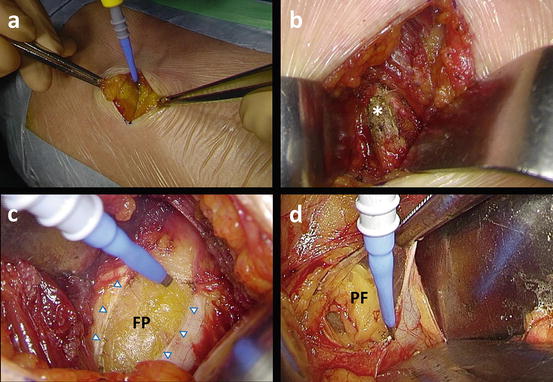
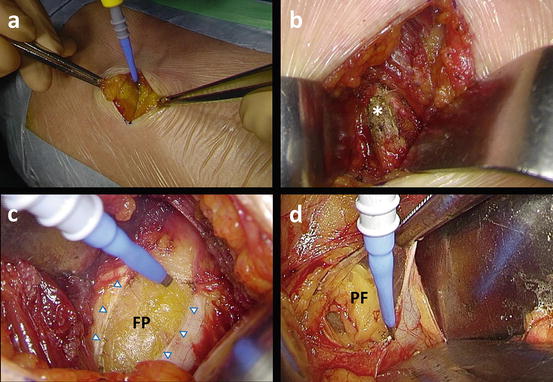
Fig. 5.13
Access to the right retroperitoneal space. (a) Skin incision is made in the flank. (b) The tip of the 12th rib (*) is slightly shaved if needed. (c) Incision of transversus abdominis aponeurosis (arrowheads). (d) Incision of lateroconal fascia. Flank pad (FP), perinephric fat (PF)
5.5.5 Dissection Along Gerota’s Fascia and Port Placement
The posterior aspect of Gerota’s fascia is dissected off the quadratus lumborum muscle (Fig. 5.14a). The anterior aspect of Gerota’s fascia is then released from the peritoneum (Fig. 5.14b). The first assistant helps the lead surgeon to produce countertraction at the dissection plane (Fig. 5.14c). The working space is maintained using long retractors (PLES retractor®, Innomedics Medical Instruments, Inc.). A single port, around 3 cm in diameter, is then prepared along Gerota’s fascia through placement of a wound retractor (Alexis wound retractor®, Applied Medical Resources, Corp.) (Fig. 5.14d).
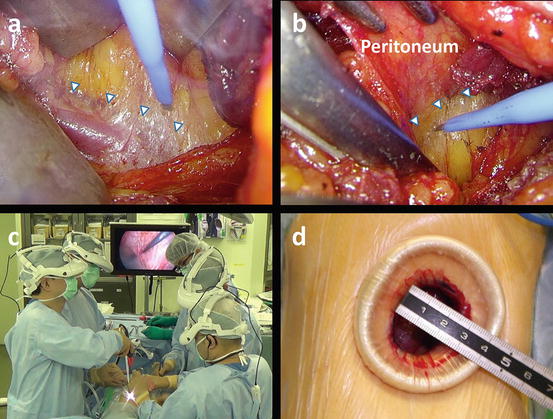
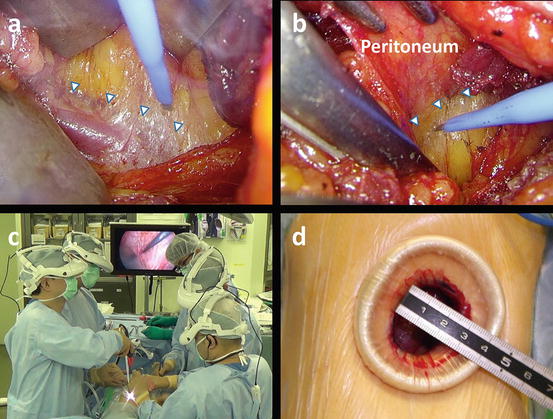
Fig. 5.14
Dissection along Gerota’s fascia and port placement. (a) Dissection along the posterior aspect of Gerota’s fascia (arrowheads). (b) Dissection along the anterior aspect of Gerota’s fascia (arrowheads). (c) External appearance in the dissection process along Gerota’s fascia. (d) A single port (2 × 3 cm)
Tip Precise plane dissection along the anatomical plane is essential to create and maintain a working space in the retroperitoneal space without CO2 insufflation.
5.5.6 Procedures for Right Adrenalectomy
A scheme of surgical procedures around the right adrenal gland is shown in Figs. 5.15 and 5.16.
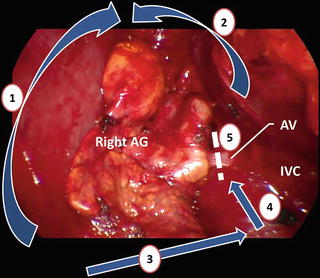
Fig. 5.15
Schematic presentation of procedures for right adrenalectomy. Step 1: dissect the posterior and cranial aspects of Gerota’s fascia off the diaphragm. Step 2: release the anterior aspect of Gerota’s fascia from the peritoneum. Step 3: transect the perinephric fat along the undersurface of the adrenal gland (AG). Step 4: dissect upward along the inferior vena cava (IVC) to identify the adrenal vein (AV). Step 5: transect the AV. Renal vein (RV)
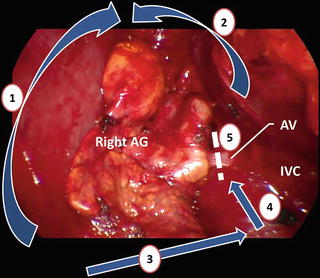
Fig. 5.16
Procedures in the operative field around the right adrenal gland (AG) as shown in Fig. 5.15. Adrenal vein (AV), inferior vena cava (IVC)
5.5.6.1 Dissection Around the Right Adrenal Gland
The right adrenal gland is dissected off the surrounding structures along Gerota’s fascia to create a large working space in the retroperitoneal cavity. The posterior and cranial aspects of Gerota’s fascia are dissected off the diaphragm. The anterior aspect of Gerota’s fascia is then released from the peritoneum and the liver (Fig. 5.17). The peritoneum covering the liver occasionally adheres to the surface of the right adrenal gland.
Fig. 5.17
Separation of the right adrenal gland (AG) from the peritoneum covering the liver
5.5.6.2 Transection of the Perinephric Fat Between the Adrenal Gland and the Kidney
The upper pole of the kidney is identified, and the perinephric fat is transected between the adrenal gland and the kidney (Fig. 5.18). The kidney is brought down caudally using a PLES retractor®or PLES spatula® (Innomedics Medical Instruments, Inc.), providing a working space that is broad enough for subsequent procedures. The inferior vena cava is identified medially in this process.




Fig. 5.18
Transection of the perinephric fat between right adrenal gland (AG) and kidney
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








