Fig. 8.1
RoboSurgeon system. Three dimensional (3D)

Fig. 8.2
Single port and the 3D head-mounted display that all surgeons wear
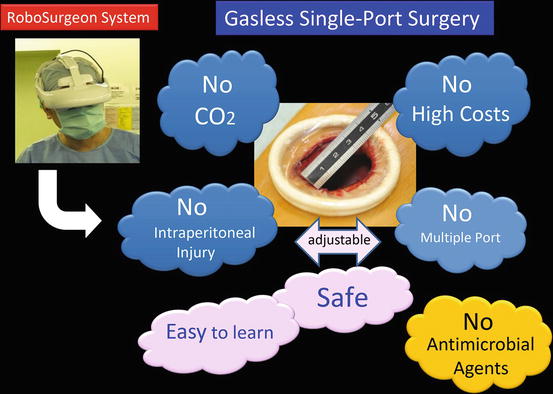
Fig. 8.3
Fundamental concept of gasless single-port RoboSurgeon surgery

Fig. 8.4
3D-HMD provides six fields of vision in front of the eyes regardless of head position
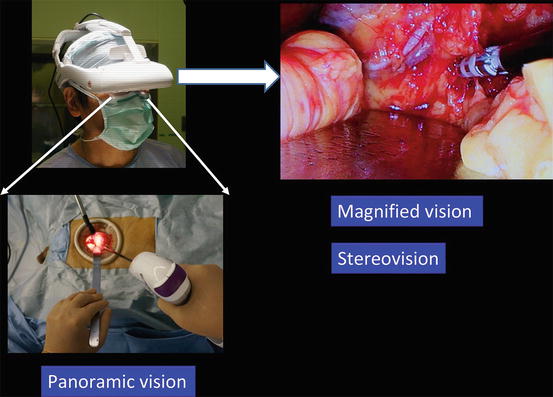
Fig. 8.5
Magnified vision, stereovision, and panoramic vision are obtained. A wide panoramic view can be seen by moving the angle of sight downward
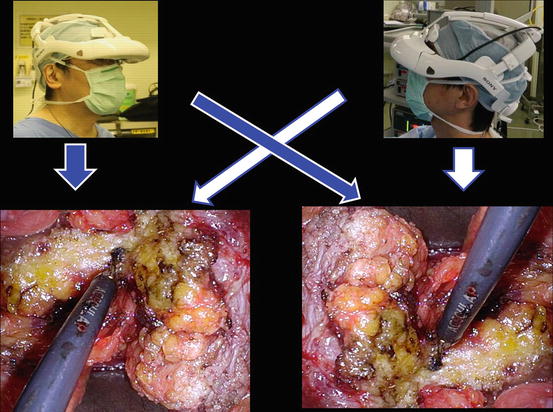
Fig. 8.6
Each surgeon can change the direction of the images on the display according to his or her position
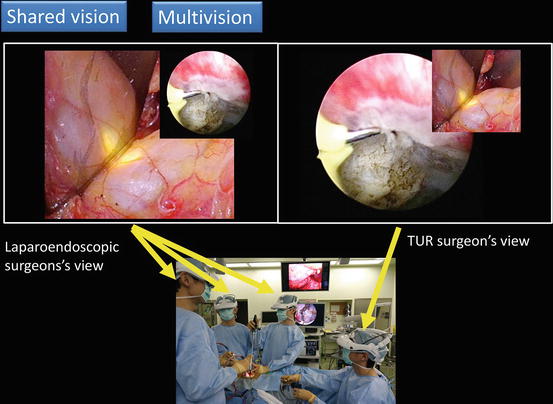
Fig. 8.7
Using multivision and the shared vision function, each surgeon can continuously and simultaneously view the laparoendoscopic and cystoscopic images in an ergonomically natural position
This surgery achieves four key “no’s”: no high costs, no CO2, no multiple ports, and no intraperitoneal injury (Fig. 8.3). The adjustable size of the port ensures safety and makes it easy to learn the procedure [16]. Prophylactic antimicrobial agents are fundamentally unnecessary in the perioperative period in clean operations, which include most of the gasless single-port surgeries [17–20]. In clean-contaminated operations including partial cystectomy, patients receive prophylactic antimicrobial agents once during surgery.
Without the RoboSurgeon system, gasless single-port-like surgery, in which the port size is somewhat larger, can be performed following the procedures presented here using a system with an ordinary two-dimensional endoscope and display [21, 22].
This surgery may help overcome some of the disadvantages of current laparoscopic and robot-assisted minimally invasive surgeries while retaining their major benefits and adding some unique advantages [23].
8.2 Hybrid Technique
Our gasless single-port RoboSurgeon partial cystectomy uses a novel hybrid technique combining an intravesical approach through a natural orifice, the external urethral orifice, and an extravesical approach through a coin-sized single port (Figs. 8.8, 8.9, and 8.10) [24]. This technique offers several advantages. First, overdissection of the bladder is prevented because the site of the tumor can be easily recognized from outside of the bladder by the transmitted light of the cystoscope passing through the bladder wall (Fig. 8.7). Second, and most important, the margin can accurately be identified under cystoscopy. The 3D-HMD system displays multiple forms of information as integrated, sharp, high-contrast images using a four-split or two-split screen or a picture-in-picture feature both seamlessly and synchronously (Fig. 8.7). Therefore, each surgeon can continuously and simultaneously see the laparoendoscopic and cystoscopic images in an ergonomically natural position (Fig. 8.7). The bladder wall is first intravesically cut deeply along the margin line while extravesically observing the bladder to confirm that there is no inadvertent injury to the surrounding tissues. This is also an advantage of the hybrid technique. After the intravesical deep incision, extravesical excision of the remaining tissue can easily be performed along the intravesically created margin line, which is yet another advantage of the hybrid technique.
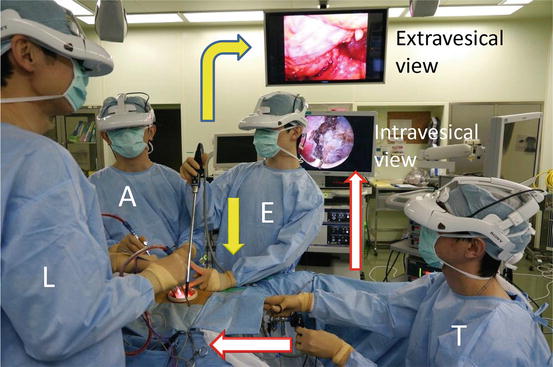
Fig. 8.8
Working space created through a single port
Fig. 8.9
Concept of gasless single-port RoboSurgeon partial cystectomy using both an intravesical approach through a natural orifice, the external urethral orifice, and an extravesical approach through a single port
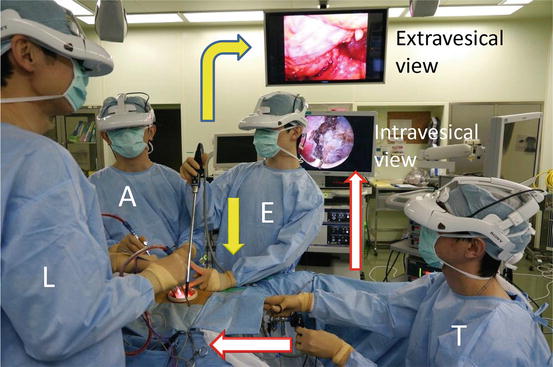
Fig. 8.10
Photograph of gasless single-port RoboSurgeon partial cystectomy. Each surgeon sees both the intravesical and extravesical view simultaneously. Lead surgeon (L); first assistant (A); endoscopist (E); TUR surgeon (T)
8.3 Preoperative Preparation
Patients are provided with sufficient information, including the potential need to extend the port size in the event of difficulties, when obtaining informed consent. Patients receive prophylactic antimicrobial agents once during the operation.
8.4 Instruments
This operation is performed using mainly reusable and affordable devices. The endoscope manipulation robot can be replaced by an endoscopist. See Chap. 1 for details.
8.5 Patient Selection
A number of benign bladder conditions, such as leiomyoma, pheochromocytoma, bladder diverticulum, cavernous hemangioma, and endometriosis, are subject to this surgery. In addition, some malignant diseases, including bladder diverticulum cancer and carefully selected cases of MIBC, can be considered for partial cystectomy. Appropriate patient selection is essential for safe and effective bladder preservation in bladder cancer. In our bladder preservation protocol, only MIBC patients who desire bladder preservation and who meet all of the criteria selectively undergo partial cystectomy with curative intent. The criteria include the following: (1) intravesically unifocal tumors (<25 % of the bladder in area), (2) no involvement of the bladder neck, and (3) no or only a small amount of residual tumor in the original MIBC site at restaging TURBT after low-dose chemoradiotherapy [7–11].
8.6 Surgical Techniques
8.6.1 Principles
All surgeons wear the 3D-HMD and obtain the following images (Figs. 8.4, 8.5, 8.6, and 8.7). During the operation, the 3D-HMD provides the following six fields of vision in front of the eyes regardless of head position: magnified vision, stereovision, panoramic vision (direct vision), multivision, navigated vision, and shared vision (Fig. 8.4). Using the direct vision obtained by moving the angle of sight downward, surgeons can receive instruments from the scrub nurse and can also observe the operative field to ensure safety. Through a single port, the surgeon initially inserts all instruments, including the endoscope, using direct vision and then follows them on the 3D-HMD. Each surgeon can change the direction of the images on the 3D-HMD according to his or her position, which makes it possible to share a common direction (Fig. 8.6). Navigated vision using transrectal ultrasonography can be employed if necessary. In partial cystectomy, each surgeon simultaneously views both laparoendoscopic and cystoscopic images using the multivision function (Fig. 8.7). A wide extraperitoneal working space is made by dissecting the Retzius space (Fig. 8.8). The working space is maintained using long retractors (PLES retractor®, Innomedics Medical Instruments, Inc.). Surgeons obtain an operative field that is large enough for manipulations deep in the wound by identifying proper planes for cleavage. The peritoneal cavity is typically preserved intact, which is unlikely to be associated with bowel complications.
8.6.2 Flowchart of the Procedure
A flowchart of the procedure is shown in Fig. 8.11. Cases of gasless single-port RoboSurgeon partial cystectomy in MIBC are presented as examples underneath.
Fig. 8.11
Flowchart of the procedure
8.6.3 Patient Positioning
After administering general anesthesia, the patient is placed in the lithotomy position (Fig. 8.12). Surgeons wear the 3D-HMD and stand by the table as shown in Fig. 8.13. The lead surgeon typically stands on the left side of the patient and sometimes at the opposite side of the tumor. The endoscopist (or the endoscope manipulation robot) and the assistant are positioned opposite the lead surgeon. The direction of the images on the lead surgeon’s 3D-HMD is reversed from those of the endoscopist/robot (Figs. 8.6 and 8.13). Therefore, each surgical team member can operate the endoscope along his or her axis of vision. The TUR surgeon is placed between the patient’s legs.
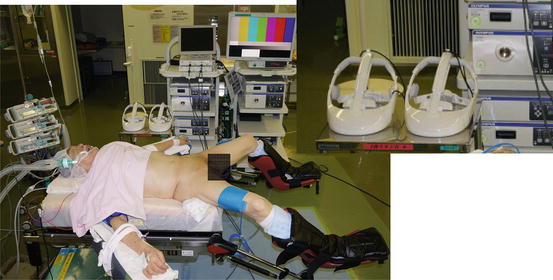
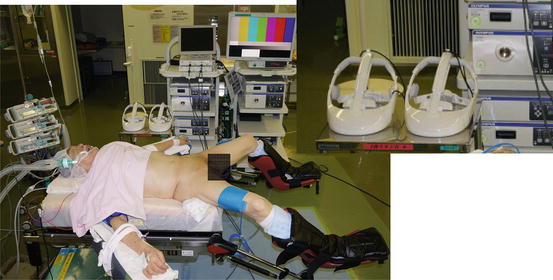
Fig. 8.12
Lithotomy position in this surgery
Fig. 8.13
Position of the surgeon. The endoscope is held by an endoscopist or a robot. The direction of the images on the lead surgeon’s 3D-HMD is reversed from those of the robot/endoscopist. Therefore, each surgical team member can operate the endoscope along his or her axis of vision
8.6.4 Preparation of a Single Port, and Dissection of the Retzius Space
A lower abdominal midline incision of around 3–4 cm in length is made (Fig. 8.14a, b), the Retzius space is dissected to the lateral umbilical ligaments (Fig. 8.14c), and a single port, usually around 3 cm in diameter, is prepared by placement of a wound retractor (Alexis wound retractor®, Applied Medical Resources, Corp.) (Fig. 8.14d). The working space is maintained using long retractors (PLES retractor®, Innomedics Medical Instruments, Inc.).
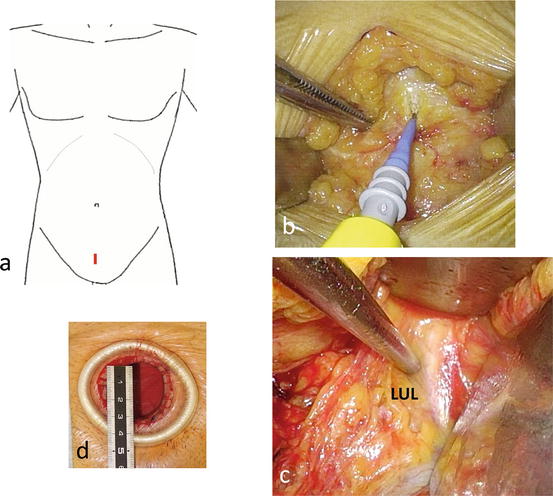
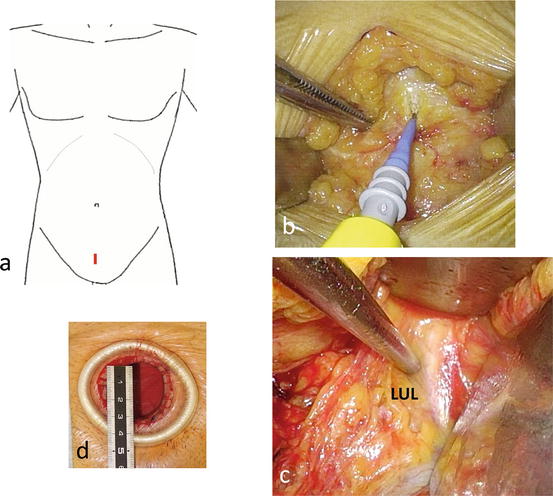
Fig. 8.14
(a–d) Preparation of a single port, and dissection of the Retzius space. Lateral umbilical ligaments (LUL).
8.6.5 Pelvic Lymph Node Dissection
Pelvic lymph node dissection can be carried out without difficulty through this port. The template for pelvic lymph node dissection includes the external iliac artery and the internal obturator muscle laterally, the internal iliac artery medially, the bifurcation of the common iliac artery cranially, and the origin of the epigastric vessels caudally. See Chap. 9 for details.
8.6.6 Extravesically Freeing a Portion of the Bladder Together with Intravesical Observation
After dissection of the Retzius space and exposure of the anterior surface of the bladder, the Iglesias resectoscope is placed into the urethra, and cystopanendoscopy is performed. On cystoscopy, the original MIBC site typically appears like a scar because these patients must meet the partial cystectomy criteria that there is no or only a small amount of residual cancer in the original MIBC site after low-dose chemoradiotherapy. Then, under laparoendoscopy, a portion of the bladder with surrounding fatty tissue is freed necessarily and sufficiently beyond the site of the tumor, which can easily be recognized from outside of the bladder by the transmitted light of the cystoscope passing through the bladder wall (Fig. 8.15).
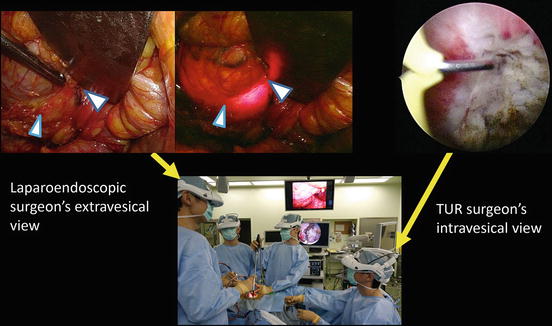




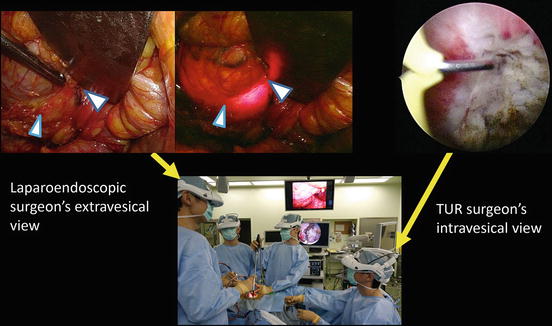
Fig. 8.15
Extravesically freeing the bladder beyond the site of the tumor while intravesically observing the original MIBC site
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








