Protack
Absorbatack
Permasorb
Sorbafix/Permafix
Ethicon Securestrap™
Company
Covidien
Covidien
Bard/Davol
Bard Davol
Ethicon
Construct





Total length
3.3 mm
5.1 mm
6.08 mm
6.7 mm
7.2 mm
Profile
~.4 mm
1 mm
~.3 mm
~.85 mm
.5 mm
Material
Titanium
PGLA
PDLLA
PDLLA
PLG blend
Delivery
5 mm
5 mm
5 mm
5 mm
5 mm
Method of delivery
Spiral
Spiral
Needle introducer
Spiral needle introducer
Expulsion
# of tacks
30
10, 20
5, 12
15, 30
25
We are going to focus on the fixation type that is most commonly used today. See Fig. 11.1a–d for devices for mechanical fixation [6–8].
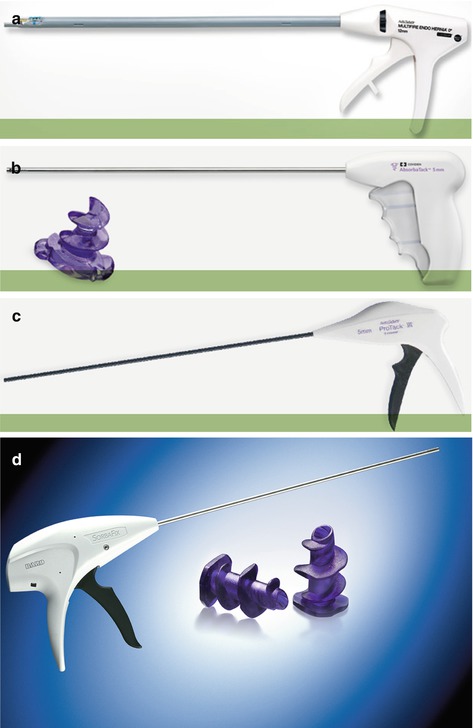
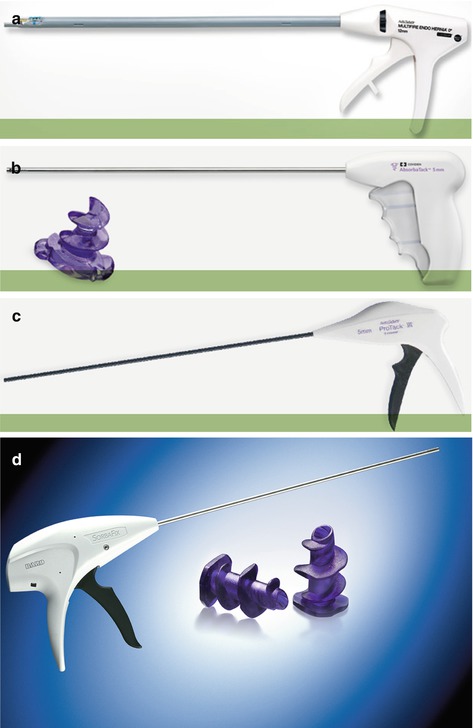
Fig. 11.1
(a–d) Devices for mechanical fixation. (a) Multi Fire Endo Hernia™ Stapler; (b) AbsorbaTack™; (c) ProTack™; (d) SorbaFix™ (a–c: Courtesy of Covidien, Dublin, Ireland; d: Courtesy of Davol, Warwick, RI, USA)
Nonabsorbable Tackers
Nonabsorbable tackers are suture materials made of titanium, allowing the attachment of the prosthetic material and the approximation of tissues in laparoscopic repair of the hernia defect. The closure can be either omega shaped or helical (Fig. 11.2). The omega shaped are the most frequently used today because they generate a single point of entry, thereby minimizing the risk of nerve entrapment.
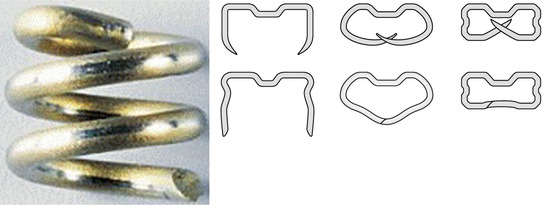
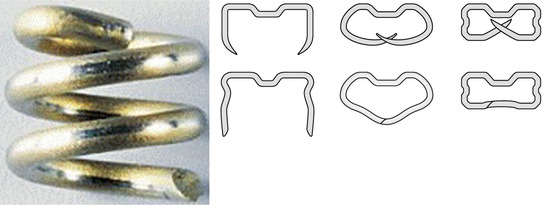
Fig. 11.2
Tacker and staples (Courtesy of Covidien, Dublin, Ireland)
Absorbable Tackers
Absorbable tackers are composed of polyglycolic acid-polylactic acid, a polymer that is reabsorbed through hydrolysis 3–5 months after surgery, with complete reabsorption in a year, thereby allowing safe and temporary fixation without any foreign body over time. This material penetrates all types of meshes and seems to be related to a reduction in chronic pain as well as a reduced risk of adhesions [1, 9].
It is vital that the fixation generated by any of the methods used is strong enough to withstand abdominal forces and friction until the mesh has been completely integrated. For many years, the permanent titanium tack was the only available option for tack fixation and therefore the gold standard [10]. However, at both short- and long-term evaluation, significant problems have been reported, such as postoperative pain, erosion, intestinal fistula, adhesion formation, and even tack hernias [11]. Due to this, in an attempt to minimize these problems, absorbable fixation methods have been developed [8]. Both Hollinsky and Gőbl [12] and Duffy et al. [13] highlighted that tensile strength was comparable to nonabsorbable fixation devices, a factor related to the possibility of recurrence [14]. Hollinksy and Gőbl [12] showed significantly higher adhesion scores with titanium tacks compared to reabsorbable devices because the tip of the permanent helical tack often does not completely penetrate the abdominal wall and small parts remain uncovered by the peritoneum; small foreign materials which are in direct contact with viscera result in adhesions to both the omentum and small bowel, and the sharp point is more harmful to the peritoneum, with local ischemia and local tissue injury resulting in more intense adhesion formation [15–17].
Transmural Sutures
Another type of traumatic attachment that should be mentioned is transmural sutures, either with reabsorbable suture material or not. However, the use of these alone has failed to become a standard technique as it requires longer operative time and requires great technical ability without providing any superior results compared to the rest [10].
After this, we can say that there are different techniques of fixation, either with single-use tackers (double crown or a crown), transfascial sutures, or a combination of both. Currently, the two most widely accepted techniques are, first, double crown of tackers (this prevents dead spaces, allowing a reduction of seroma between the mesh and the hernia sac, ensuring adequate fixation of the mesh when placing a crown of internal fixation at the level of the fibrotic ring, and preventing recurrence by default enlargement [7]) and, second, a combination of tackers and transfascial sutures [1]. See Fig. 11.3a–d for devices for transmural sutures.
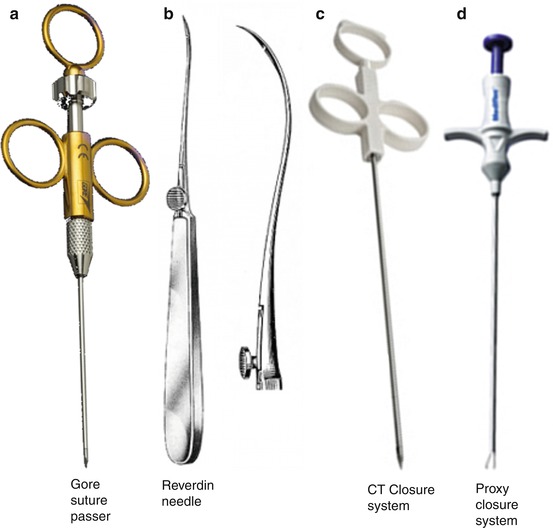
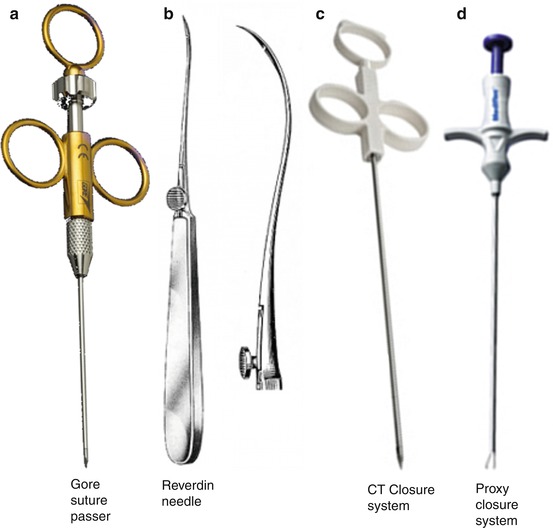
Fig. 11.3
(a–d) Devices for transmural sutures. (a) GORE™ suture passer (Courtesy of L. Gore and Associates, Newark, DE, USA); (b) Reverdin needle. (c) CT Closure System® (Courtesy of Cooper Surgical, Trumbull, CT, USA). (d) Proxy closure system (Courtesy of Ranfac Corp, Avon, MA, USA)
One of the most controversial issues in the majority of existing literature, even given greater consideration than that of recurrence, is postoperative pain in this type of patient. Traditionally, most authors thought that the pain was caused by the transmural sutures, because pain after LVHR is frequently associated with movement and a pulling sensation at the site of transmural sutures placement [11]. However, more and more published work finds that there is no difference and that both transfascial sutures and the use of tackers are responsible for prolonged postoperative pain. Carbajo et al. [18] reported a 7.4 % rate of persistent postoperative pain using the double crown technique. Bageacu et al. [19] observed the persistence of severe pain in patients who only had tackers. Recently, a randomized study comparing commonly used fixation techniques (double crown, tackers and nonabsorbable sutures, and tackers and absorbable sutures) with respect to postoperative pain and quality of life has been published. In this study, they also included a group of patients in whom absorbable transmural sutures were employed to affix the mesh, speculating that if postoperative pain is due to the presence of a permanent mesh-fixation device, the potential for such pain might decrease over time in patients in whom an absorbable material is used instead. However, after obtaining their results, the authors concluded that there are no differences in terms of postoperative pain and quality of life with respect to any of the three techniques [8], and they suggest that none of the techniques is superior to another in terms of pain reduction. Therefore, it is necessary to develop new methods of fixing mesh to treat postoperative pain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








