Fig. 32.1
Sagittal MRI indentifying tumour and length of endocervical canal, with distance from isthmus
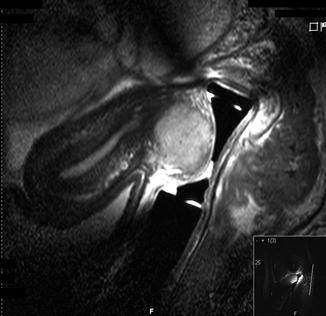
Fig. 32.2
Endovaginal coil MRI scan identifying tumour
32.4 Staging
The traditional method of staging is by clinical examination under anesthesia (staging EUA). Applying FIGO staging [11] (Table 32.1) enables a decision to be made as to the best form of treatment. Stages IAI and IAII may be adequately treated by cone biopsy ensuring that an adequate margin of clearance is obtained. Risk of lymph node involvement for a stage IAI tumour is 1 % increasing up to 7–8 % in stage IAII [12]. With lympho-vascular space invasion (LVSI), a pelvic node dissection is required and the incidence of this in stages IAI and IAII is between 3 and 4 %. The incidence of lymph node involvement, with metastases increases to 16–18 % with stage IB tumours. These lesions require a thorough pelvic node dissection with a Wertheim’s radical hysterectomy.
TNM | FIGO | Surgical-pathologic findings |
|---|---|---|
Categories | Stages | |
TX | Primary tumour cannot be assessed | |
T0 | No evidence of primary tumour | |
Tis | Carcinoma in situ (pre-invasive carcinoma) | |
T1 | I | Cervical carcinoma confined to the cervix (disregard extension to the corpus) |
T1a | IA | Invasive carcinoma diagnosed only by microscopy; stromal invasion with a maximum depth of 5.0 mm measured from the base of the epithelium and a horizontal spread of 7.0 mm or less; vascular space involvement, venous or lymphatic, does not affect classification |
T1a1 | IA1 | Measured stromal invasion ≤3.0 mm in depth and ≤7.0 mm in horizontal spread |
T1a2 | IA2 | Measured stromal invasion >3.0 mm and ≤5.0 mm with a horizontal spread ≤7.0 mm |
T1b | IB | Clinically visible lesion confined to the cervix or microscopic lesion greater than T1a/IA2 |
T1b1 | IB1 | Clinically visible lesion ≤4.0 cm in greatest dimension |
T1b2 | IB2 | Clinically visible lesion >4.0 cm in greatest dimension |
T2 | II | Cervical carcinoma invades beyond uterus but not to pelvic wall or to lower third of vagina |
T2a | IIA | Tumour without parametrial invasion |
T2a1 | IIA1 | Clinically visible lesion ≤4.0 cm in greatest dimension |
T2a2 | IIA2 | Clinically visible lesion >4.0 cm in greatest dimension |
T2b | IIB | Tumour with parametrial invasion |
T3 | III | Tumour extends to pelvic wall and/or involves lower third of vagina and/or causes hydronephrosis or nonfunctional kidney |
T3a | IIIA | Tumour involves lower third of vagina, no extension to pelvic wall |
T3b | IIIB | Tumour extends to pelvic wall and/or causes hydronephrosis or nonfunctional kidney |
T4 | IV | Tumour invades mucosa of bladder or rectum and/or extends beyond true pelvis (bullous oedema is not sufficient to classify a tumour as T4) |
T4a | IVA | Tumour invades mucosa of bladder or rectum (bullous oedema is not sufficient to classify a tumour as T4) |
T4b | IVB | Tumour extends beyond true pelvis |
Regional lymph nodes (N) | ||
NX | Regional lymph nodes cannot be assessed | |
N0 | No regional lymph node metastasis | |
N1 | Regional lymph node metastasis | |
Distant metastasis (M) | ||
M0 | No distant metastasis | |
M1 | Distant metastasis (including peritoneal spread; involvement of supraclavicular, mediastinal, or para-aortic lymph nodes; and lung, liver, or bone) | |
Pelvic node dissection may be carried out by laparoscopy with or without robotic assistance. This is part of the overall staging procedure but whether the removal of microscopically negative lymph nodes as an en bloc dissection is therapeutic, is debatable. Improving imaging perhaps with PET scanning or sentinel node assessment may change this.
32.5 Radical Trachelectomy: Selection of Method
There is debate as to which surgical approach should be undertaken; vaginal or abdominal. Abdominal surgery may be open, laparoscopic or with robotic assistance. Careful patient selection will result in low morbidity with low recurrence rates and acceptably high pregnancy rates. The risk of significant prematurity may be decreased if it is possible to conserve a small portion of the upper (proximal) cervix at the isthmus depending on the exact position of the tumour and the ability to obtain an adequate, clear margin.
Most authorities agree that the upper limit in size for suitability is 2 cm in diameter. However the overall volume needs to be taken into account. Radical vaginal trachelectomy involves the first or bottom part of a Schauta radical hysterectomy. This can be challenging to perform, hence some oncological surgeons have opted for the abdominal approach. Practice with the vaginal technique allows adequate vaginal and para-cervical resection which may be tailored to the needs of the tumour. The difficulty that some may have is in mobilizing the ureter which they may feel more comfortable dealing with abdominally. Whilst potential complications maybe the same, there is a reduced hospital stay and less inconvenience to the patient, making the vagina the favoured approach to the authors.
32.6 Pelvic Node Dissection
This is carried out laparoscopically either at the time of the staging EUA or in conjunction with the vaginal trachelectomy. The advantage of the former is that patients with positive lymph node metastases are identified before definitive surgery to the cervix is undertaken. A four portal approach is employed using a Hasson direct entry technique. The abdominal and pelvic cavity is thoroughly inspected not only to look for possible metastatic disease especially involving the pelvic peritoneum and Pouch of Douglas but also to look for other pathology such as endometriosis or chronic pelvic inflammation.
The pelvic side walls are exposed with a T shaped incision into the peritoneum overlying the external iliac vessels, just proximal to the round ligaments. The infundibulo-pelvic ligament is identified and separated from the ureter. The nodes are removed from the lower common iliac, internal and external iliac and obturator regions. The obturator nerve is exposed and conserved. The paravesical space is identified and opened. Care is taken to avoid aberrant obturator vessels.
The procedure is repeated on the contralateral side resulting in a harvest of approximately 30–40 lymph nodes.
32.7 Radical Vaginal Trachelectomy (RVT)
An extended lithotomy position is used to expose the cervix which is infiltrated with 0.25 % Bupivacaine and 1 in 200,000 adrenaline. The technique is well described by Shepherd [13] utilizing a circumcervical incision including a 2 cm cuff of vagina with cutting diathermy. Sharp dissection mobilizes the bladder anteriorly, identifying the bladder pillars by opening the paravesical space on either side. Posteriorly the uterosacral ligaments and rectovaginal septum are identified. The harmonic scalpel (ultracision Eithicon endoscopy LLC) is used for dissection and haemostasis. The bladder pillar is transected and the descending branch of the uterine artery supplying the cervix is isolated and divided after cauterization. The ureteric tunnel is identified and the ureter reflected cranially and laterally. The dissection continues laterally dividing the lateral (cardinal) ligaments the utero-sacral ligaments posterolaterally. As much paracervical and paravaginal tissue as necessary depending on the size of the tumour, should be resected (Fig. 32.3). To give an adequate 1–2 cm clearance of tumour-free tissue. The rectovaginal septum is incised and the tissue posteriorly pushed by blunt dissection cranially. It is not necessary to open the Pouch of Douglas and by keeping this closed possible sepsis spreading to the pelvis is avoided. If the peritoneal cavity is opened, this may be easily closed with absorbable sutures. The dissection is performed on both sides thus mobilizing the central cervix including a 2 cm cuff of vagina. A no. 6 Hegar dilator is placed into the endocervical canal which may then be transected using cutting diathermy (Fig. 32.4). The isthmus is easily identified by visualizing where the peritoneum is reflected anteriorly, above the uteroversical ligament and posteriorally at the reflection of the Pouch of Douglas. An individual decision is taken as to whether a complete trachelectomy removing all the cervix is required or whether it is possible to conserve a small cuff of proximal upper cervix depending on the exact location of the tumour.
Fig. 32.3
Tissue to be resected
Fig. 32.4
Transecting isthmus with cutting diathermy
32.8 Isthmic Cerclage
An isthmic cerclage using monofilament, non-absorbable material, such as No 1 nylon or prolene, is inserted with four large bites around the isthmus, through the stroma of the cervix. Care is taken not to occlude the isthmic os by keeping the Hegar dilator in situ during this procedure. The knot is tied anteriorly around this dilator. This will allow normal menstruation to occur and passage of a cannula for any future necessary procedures.
32.9 Vagino-Isthmic Anastomosis
Holding the cerclage suture for identification and traction, the vaginal margins are grasped and anastomosed to the isthmus using four interrupted mattress sutures with no 1 Vicryl (Polyglactin, Ethicon). Care is taken to avoid closing the isthmic and endocervical canal by leaving the Hegar 6 dilator in situ whilst inserting the sutures. Two or three further mattress sutures are placed on either side to close the angles of the lateral fornices (Fig. 32.5).