, Mark Thomas1 and David Milford2
(1)
Department of Renal Medicine, Birmingham Heartlands Hospital, Birmingham, UK
(2)
Birmingham Children’s Hospital, Birmingham, UK
Abstract
In this chapter we explain:
How to assess fluid balance
The importance of examining the abdomen
Common signs of a vasculitic illness
This chapter is placed after the chapters on history, height, weight, blood pressure and urine testing because the physical examination should be tailored according to these results. The blood pressure and urinalysis may have been tested before you see the patient. If not, include them as part of your examination.
Fluid Balance
How Salt and Water Is Distributed in the Body
Salt and water are distributed in three functionally separate compartments – inside the cells (intracellular fluid), around the cells (interstitial fluid) and in blood vessels (plasma).
Before trying to judge a patient’s salt and water balance from the physical examination, first take a history. For example, if someone has had diarrhoea and vomiting for a week and has lost weight they will be salt and water depleted. The examination is then used to judge the severity of the salt and water depletion and whether it is affecting plasma volume as well as interstitial fluid.
In children, the percentage change in body weight is used to guide the route and volume of fluid replacement. Weight loss of more than 10 % of body weight indicates reduced plasma volume and requires intravenous fluid replacement. In adults, low blood pressure and a rise in pulse rate of >20 bpm from sitting to standing or >30 bpm from supine to standing indicate reduced plasma volume.
Traditional signs of reduced interstitial fluid volume such as reduced skin turgor are not reliable in the elderly [1].
Oedema indicates excess interstitial fluid. Interstitial fluid is formed at the arterial end of the capillary bed by hydrostatic pressure forcing fluid across the capillary wall. It is removed at the venous end by osmotic force drawing it back into the capillary lumen, and also by the lymphatic system (Fig. 12.1).
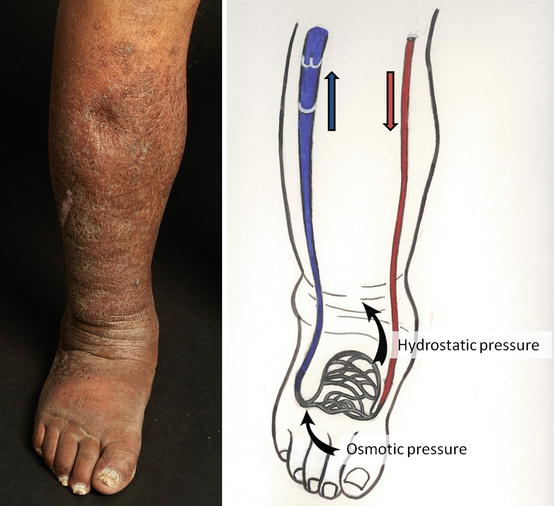
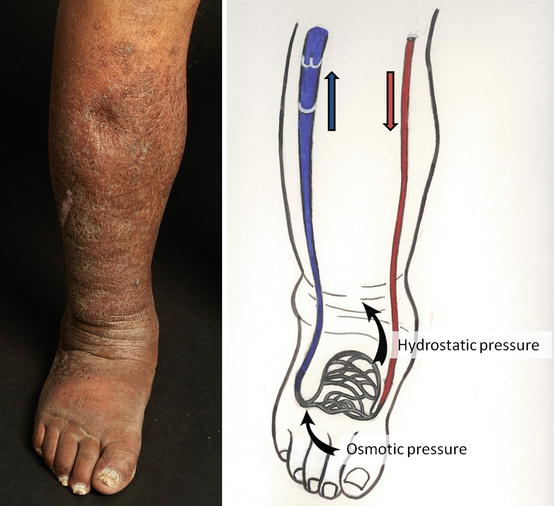
Fig. 12.1
The formation of oedema. Fluid is forced from the capillary bed at the arterial end by hydrostatic pressure and returns at the venous end by osmotic pressure
Salt and water overload leads to increased hydrostatic pressure and oedema. A little puffiness at the ankles indicates a kilogram or two of excess fluid. Oedema to the knees may indicate five kilograms; oedema up to the abdomen may mean more than 20 kg of fluid overload. Fluid may also accumulate in spaces that are normally dry, for example as pleural effusions and ascites.
Older people develop oedema more readily than younger people. It can be hard to detect fluid overload in younger patients as they become hypertensive but do not show oedema. Patients with low serum albumin tend to form oedema more easily due to the reduced capillary osmotic pressure.
Interstitial fluid can flow within subcutaneous tissue. This allows oedema to form a pit when it is compressed by your thumb over the tibia (Fig. 12.2). Lymphoedema is non-pitting because the fluid is in lymphatic vessels and cannot move.


Fig. 12.2
This man has had nephrotic syndrome for a few weeks. The oedema is soft and pits easily with gentle pressure. An imprint of the fingers on the tibia is seen above the gloved hand
How Excess Salt and Water Can Be Removed
For oedema to be removed, salt excretion must exceed salt intake. As most drinks are hypotonic, imposing a limit on fluid intake – fluid restriction – is effectively water deprivation. This is either pointless, as the kidneys will counteract by concentrating the urine, or dangerous as it will eventually cause hypernatraemia.
Restricting salt intake may reduce oedema in chronic heart failure [2], although this is controversial [3], and helps to lower blood pressure and slow the decline in GFR in CKD [4].
The principal treatment of fluid overload is to increase salt excretion by the kidneys with diuretic drugs . The kidneys can only excrete salt and water that is in the plasma; interstitial fluid has to re-enter the plasma volume before it can be excreted. Ideally the rate of excretion from the plasma is in equilibrium with the rate of refilling of plasma from the interstitial fluid. Refilling from pleural effusions and ascites is slower than from the interstitial fluid.
In patients with nephrotic syndrome, hypoalbuminaemia lowers the low plasma osmotic pressure and slows the reabsorption of interstitial fluid. Plasma volume is more likely to fall when diuretics are given.
When salt and water are excreted faster than plasma volume is refilled, plasma volume is reduced and the reabsorption of glomerular filtrate by the tubules is increased. The flow of filtrate along the tubules is slowed, allowing more urea to diffuse out of the tubule into the plasma. This can be detected by an increase in the urea-to-creatinine ratio (see Sect. “Serum urea and creatinine – different measures of kidney function” in page 26).
Leg swelling typically increases during the day because venous pressure is increased by gravity. When the legs are raised to the level of the heart in bed at night, the oedema is reabsorbed, leading to nocturia.
Elderly people with heart failure may sleep in a chair rather than a bed because they get breathless if they lie flat. The venous return from their legs is continually exposed to gravity and fluid cannot leave the tissues. This can lead to chronic oedema and venous ulceration.
Similarly, in patients with high venous pressure due to right heart failure – cor pulmonale – oedema is harder to remove with diuretics and the urea-to-creatinine ratio is more likely to increase.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








