Equipment, Operating Room Setup, and Patient Positioning
KEY POINTS
Monitor placement for viewing by entire operating room team.
Access to supply of CO2.
Electric bed with stirrups.
Access to electrocautery instruments.
Digital recording equipment to document procedures for training and education.
ADDITIONAL ADVICE
If individual CO2 tanks are used, ensure that the connected tank is full and an additional full tank is present in the room to avoid unnecessary delays.
The operating surgeon should be familiar with basic equipment setup and troubleshooting to avoid unnecessary delays or conversion to open procedures in case of equipment failure.
Personalize both open and laparoscopic instrument trays for individual preferences for each procedure.
GENERAL OPERATING ROOM REQUIREMENTS
Many procedures have adopted specific setup and form, but a generic layout should be familiar to most surgeons. The key issues that must be considered are positioning of monitors for viewing by the entire operating room (OR) team, easy access to carbon dioxide for insufflation, and proximity to generators for cautery or other energy instruments. An electric operating bed with stirrups for the legs is ideal so the patient can be easily airplaned during the case for the different positions required for access.
Monitors are best placed on booms to allow a full range of motion for optimal visualization by the operating team. It is possible to use carts for the same purpose; however, they occupy more floor space and limit mobility in the room.
Carbon dioxide (CO2) may be supplied from a central location and piped into the room. This approach is superior because it diminishes issues related to temperature
differences for the gas that may promote fogging. The majority of surgeons use individual tanks, which carry the risk of running out of gas.
differences for the gas that may promote fogging. The majority of surgeons use individual tanks, which carry the risk of running out of gas.
There are a variety of energy modalities which may be used in laparoscopic surgery. These include monopolar and bipolar cautery, harmonic scalpels, and sealing devices such as the LigaSure. Each of these requires a generator that must be located close enough to allow the cords to reach onto the field. Once again, placing these devices on a single boom is the most efficient means of providing access to the field and to the circulating nurse. Carts can be used in a similar fashion, but again occupy more floor space and limit mobility in the room.
A final point to consider is the ability to take advantage of video technology to allow for digital capture of the procedure. DVD technology is readily available and a recorder can be placed on the cart or boom with a light source to allow the surgeon to capture the entire procedure on video. Alternatively, high-resolution printers can be used to capture still pictures of portions of the surgical procedure.
High-definition monitors offer exceptional resolution and definition of the operative field. The high-definition monitors were initially introduced with robotic technology, but have expanded to laparoscopy at a fraction of the price.
PATIENT POSITIONING
The patient is placed supine on the operating table on a bean bag with pneumatic compression devices. The OR table needs the ability to remove the leg section, which is then placed aside. General anesthesia is induced, and insertion of an orogastric tube and Foley catheter is performed.
Ideally, both arms are tucked at the patient’s side. For patients that the anesthesiologist requires access or morbidly obese patients where the OR table cannot accommodate the full body, an arm may be kept out on the same side of the colon being removed. The arm should not be kept out on the side opposite the colon being removed because the assistant will need space to stand beside the primary surgeon for the majority of the case.
The legs are placed in Dan-Allen or Yellofins® stirrups. The legs are kept in position with the knees slightly flexed, and the hips straight or even slightly extended (see Fig. 2.1). The patient’s perineum needs to be flush with the lower end of the bed to provide access for stapler insertion and anastomosis. The bean bag is now aspirated, fixing the patient in position. In our practice, shoulder straps are not routinely used to reduce the risk of brachial plexus injury. Chest strapping with adhesive tape may be used in morbidly obese patients.
The abdomen is prepared with antiseptic solution and draped routinely. We use disposable drapes with pockets, which allow the cords to be controlled and positioned out of the operating team’s way.
EQUIPMENT POSITIONING
Cables for CO2, light, cautery, and other energy sources are dependent on the layout of individual ORs. Generally, it is best to have them run off at the cephalad end, so the surgeon and assistant are not trapped beside the patient.
Monitor positions are described in each individual chapter for the respective type of colectomy. Generally, the primary monitor is placed on the side of the colectomy at the level of the patient’s hip. The secondary monitor is placed on the opposite side at the level of the patient’s shoulder and is mainly for the assistant during the early phase of the operation and port insertion (see Fig. 2.2).
The scrub nurse’s instrument table is placed between the patient’s legs and is mobile to permit the surgeon to move between the patient’s legs for total colectomies, or the taking down of the splenic flexure. There should be sufficient space to allow the operator to move from either side of the patient and between the patient’s legs as necessary.
UMBILICAL PORT INSERTION
The umbilical port is inserted using a modified Hassan approach. A vertical, 1-cm subumbilical incision is made. This is developed down to the linea alba, which is then grasped on each side of the midline using Kocher clamps. A no. 15 blade is used to open the fascia between the Kocher clamps and Kelly forceps are used to bluntly
open the peritoneum. It is important to keep this opening small (<1 cm) to minimize air leaks.
open the peritoneum. It is important to keep this opening small (<1 cm) to minimize air leaks.
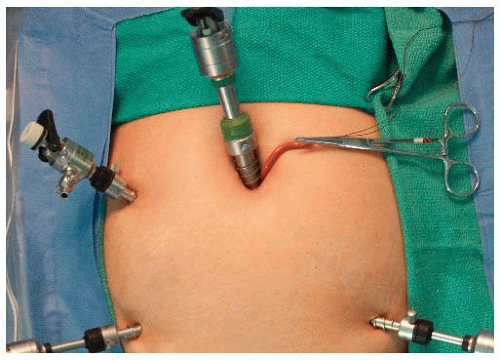
Having confirmed entry into the peritoneal cavity, a purse string of 0 polyglycolic acid is placed around the subumbilical fascial defect (umbilical port site) and a Rommel tourniquet applied (see Fig. 2.3). A 10-mm reusable port is inserted through this port site, allowing the abdomen to be insufflated with CO2 to a pressure of 12 mmHg. The camera is inserted into the abdomen and initial laparoscopy performed to carefully evaluate the liver, small bowel, adhesions, and peritoneal surfaces. Remaining ports are placed as necessary.
BASIC LAPAROSCOPIC INSTRUMENTS
It should be noted that nearly all the instruments that are described are currently available both in reusable format and as a disposable model. The rationale for using a disposable version of a reusable instrument may be related to operator preference, hospital and operative economics, and particularly case load volume for each surgical practice.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree