, Liqing Yao1 and Xinyu Qin2
(1)
Endoscopy Center, Zhongshan Hospital Fudan University, Shanghai, People’s Republic of China
(2)
General surgery, Zhongshan Hospital Fudan University, Shanghai, People’s Republic of China
Abstract
Endoscopic submucosa resection (EMR) has revolutionized the diagnosis, staging and treatment of early stage mucosal neoplasm of gastrointestinal tract. As minimally invasive procedure, it offers endoscopic alternative to surgical resection that has higher morbidity, mortality and cost. The technique of EMR is continuously evolving. Standardization of this technique is important to optimize the outcome. In this chapter we will discuss snare polypectomy and EMR.
Endoscopic submucosa resection (EMR) has revolutionized the diagnosis, staging and treatment of early stage mucosal neoplasm of gastrointestinal tract. As minimally invasive procedure, it offers endoscopic alternative to surgical resection that has higher morbidity, mortality and cost. The technique of EMR is continuously evolving. Standardization of this technique is important to optimize the outcome. In this chapter we will discuss snare polypectomy and EMR.
3.1 Snare Polypectomy
3.1.1 Indications and Contraindications
3.1.1.1 Indications and Patients Selection
Appropriate patients are those in whom concern of malignancy is low and size and location of polyp is feasible for successful resection with low rate of complications. Snare polypectomy is suitable for most large pedunculated and sessile polyp <2.5 cm.
3.1.1.2 Contraindications
Contraindication are relative but generally polypectomy should be avoided if:
Sessile polyp base >2 cm in diameter. Performing a snare polypectomy on a sessile polyp >2 cm in size usually leads to higher rate of bleeding and perforation. Incomplete excision may result in local recurrence. As the prevalence of malignancy in non-granular sessile polyp >2 cm is high hence we prefer to remove these polyps with ESD technique to achieve Ro resection.
Multiple polyps of a large number and familial polyposis coli;
Suspicious of malignancy (Paris type 0-11 + c)
Patients with bleeding tendency.
However, the contraindications mentioned above are not absolute. For elderly patients who cannot tolerate laparotomy, snare polypectomy is still an option to treat sessile polyps >2 cm in size. Multiple polyps can also be resected by snare polypectomy in batches. Even for familial polyposis coli patients, endoscopists can adopt polypectomy to remove large polyps with a regular follow-up before choosing pancolectomy. Suspected malignant pedunculated polyps may also be removed with polypectomy followed by a microscopic examination, and if the pedicle of the polyp is confirmed free of tumor, further treatment may not be necessary.
As mentioned above, the indications and contraindications should be individualized depending on the overall status of patients, types of polyp, and skills of the endoscopist.
3.1.2 Patient Preparation
3.1.2.1 General Information
General information includes patient’s clinical history, overall conditions, and comorbid illnesses such as diabetes, hypertension, asthma, dysfunction of vital organs. Drug history is important particularly if patient is on Clopidogrel or anti-coagulants. Before endoscopic treatment we check blood tests such as blood count, liver and renal function and coagulation screen.
3.1.2.2 Bowel Preparation
Bowel preparation is essential and influences the outcome of colonoscopic polypectomy. Polyethylene glycol (PEG) electrolytes powder is most commonly used as oral purgatives. The PEG electrolytes powder, given 4 h before the examination, is associated with an excellent cleansing efficacy as well as less residual feces and fewer bubbles. For Gastroscopy patients are kept nil by mouth for 4–6 h.
3.1.2.3 Informed Consent
It is mandatory to fully inform the patient or his/her guardian before polypectomy about the procedure, benefits and risks such as bleeding and perforation.
3.1.2.4 Equipment Preparation
Polypectomy equipment should be prepared with the correct connection with high frequency electrical generator by an assistant or a nurse before procedure.
3.1.2.5 Pre-operative Medication
Use of antispasmodics or sedatives is not considered as a routine before polypectomy. However, for patients with increased colonic contractility, use of antispasmodics may help relax colon and facilitate polypectomy.
3.1.3 Importance of the Assistant
An endoscopic assistant is important member of team and should be made aware of the procedure and familiar with all the equipment and accessories needed. The cooperation between endoscopist and assistant is of great importance especially when it comes to removing the polyp. An experienced assistant is capable of coordinating with the endoscopist snaring the polyp at precisely the right moment. Furthermore, the degree of tightness when closing the snare must be moderate in case the loop closes too tightly to make a mechanical cutting of the polyp without adequate coagulation, resulting in bleeding. Some experienced endoscopist prefer close the snare themselves for controlled polypectomy.
3.1.4 Techniques for Resection
Routine endoscopic examination of colon or upper gastrointestinal tract should always be performed before polypectomy. Polypectomy can be performed during the withdrawal of endoscopy. Before rushing into the exciting part, always take time to optimize the view and position of the polyp. Choose the best approach and the most suitable devices after visual assessment of the shape and size of the polyp. Polyps in some special locations, such as fundus of stomach and rectum near dentate line, are often easy to find but hard to snare. In these cases retroflexion maneuver can be helpful to access these polyps.
3.1.4.1 Polyps <0.5 cm in Size
Polyps less than 0.5 cm in size, can be excised by direct snaring with + or without electro cautery, as well as hot biopsy forceps, or destroyed by APC (Figs. 3.1, 3.2, and 3.3). lifting the polyp can protect deep layer of the intestinal walls from electric burns. Tissues grasped in hot biopsy forceps should be sent to the lab as routine for histopathology examination. Smaller lesion even can be removed with cold snare.


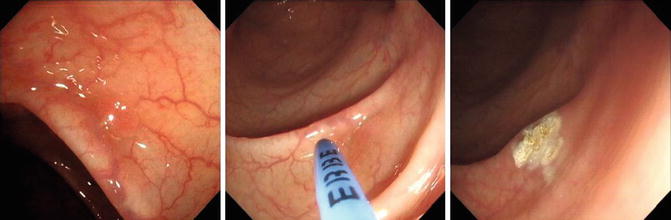

Fig. 3.1
Removing a small colon polyp by snare

Fig. 3.2
Removal of a small polyp in rectum by biopsy forceps
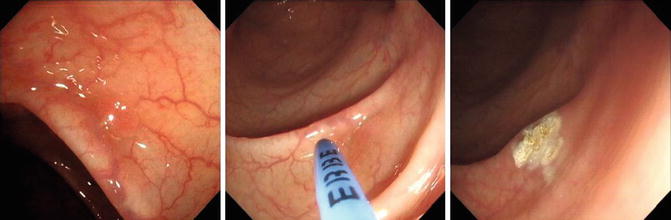
Fig. 3.3
APC treatment for a small colon polyp
3.1.4.2 Pedunculated Polyps
Small pedunculated polyps can be resected by snare polypectomy (Fig. 3.4). Large polyps may keep the pedicle out of sight, in which case using the head of the colonoscopy or forceps to push the polyp, or a change of the patient position and moderate air insufflation should expose the hidden stalk (Fig. 3.5). Avoid snaring the polyp if views suboptimal, because it may become difficult to pull off the loop and may result in unexpected bleeding.
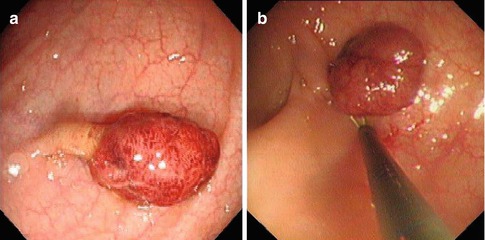
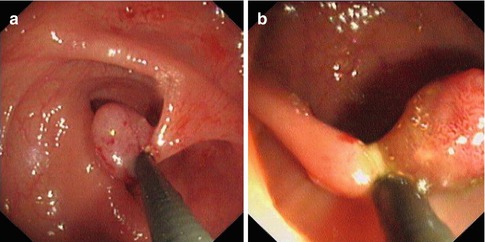
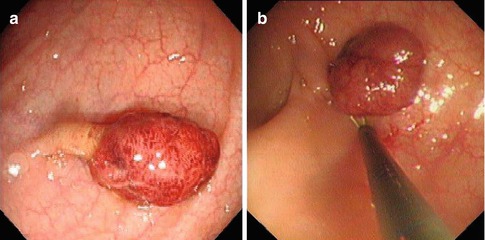
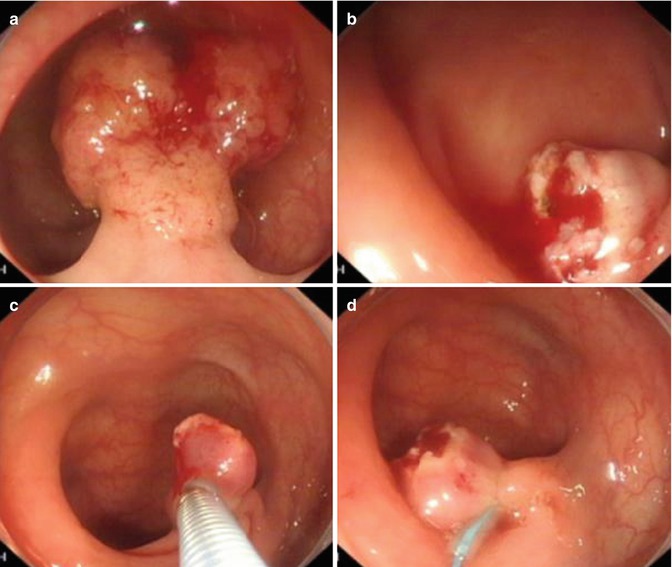
Fig. 3.4
Snare polypectomy of a pedunculated polyp. (a) A hyperemia polyp was found in colon with thin stalk. (b) Snare polypectomy was performed
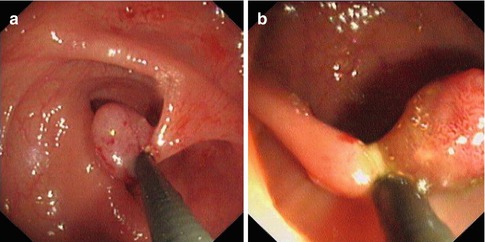
Fig. 3.5
(a) Lifting the polyp away from the intestinal wall. (b) Conserving part of the pedicle
Before resecting the polyp, optimize the view and position, fully expose the polyp, and lift it away from the intestinal wall in order to prevent mucosal burns which results from the attachment of polyp and intestinal wall.
Polyp with short pedicles, the snare should be tightened as proximal to the polyp as possible, but polyp with long stalk, it is appropriate to leave 0.5–1 cm of the pedicle (Fig. 3.6). There is no need to worry about the recurrence due to the residual pedicle because the pedicle is formed resulting from the normal mucosa pulled away by polyp instead of becoming part of polyp itself. Keeping a certain length of the pedicle ensures sufficient coagulation and reduce risk of bleeding and perforation.
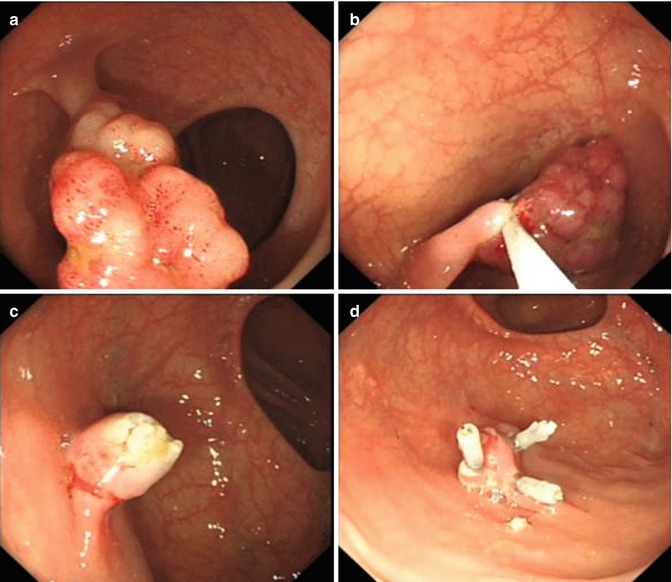
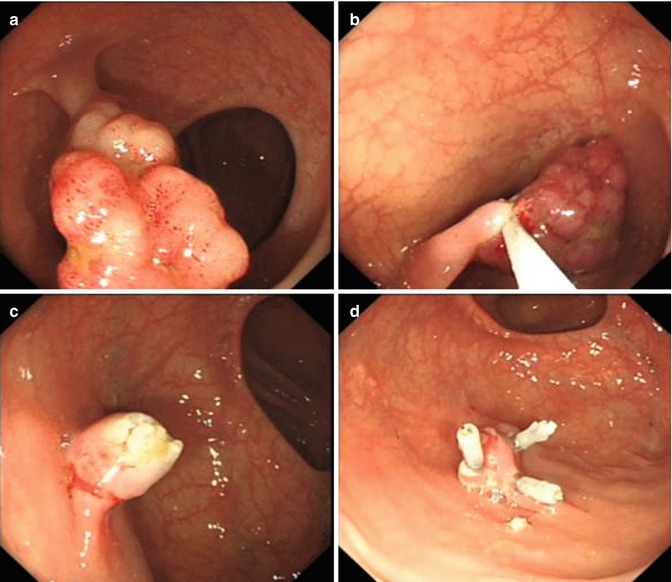
Fig. 3.6
Management of a pedunculated polyp. (a) Apedunculated polyp in colon. (b) Placing the snare proximal to the polyp. (c) Resect the polyp by electric current. (d) Using metallic clips to close the wound after the procedure
Another major concern when confronting thick-pedicle polyps or polyps with suspicious large blood vessels is the bleeding after resection. One way to prevent this complication is using an endoloop to ligate the pedicle or a metallic clip to clamp the pedicle before resection (Figs. 3.7 and 3.8), and clamping the residual pedicle with hemoclips again after the procedure to stop or prevent bleeding. Most large pedunculated polyps can be removed with suitable snares, but if the polyp head is bigger than the largest snare endoscopist can remove it in piecemeal.
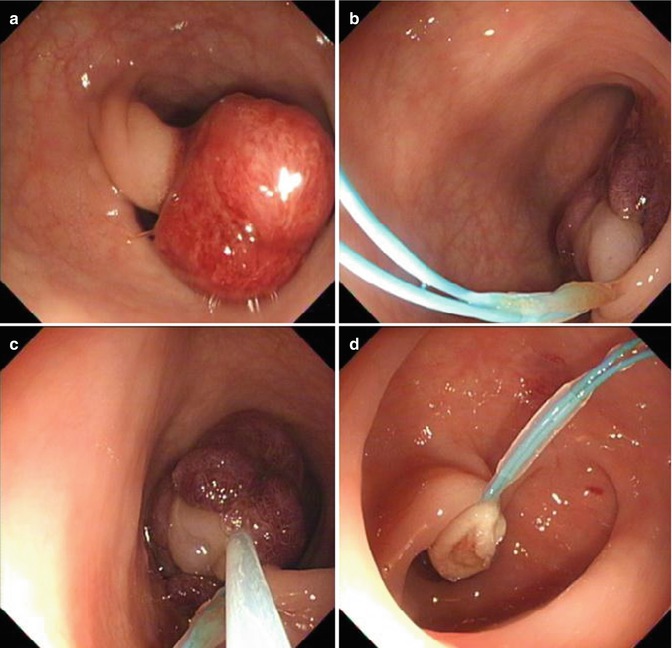
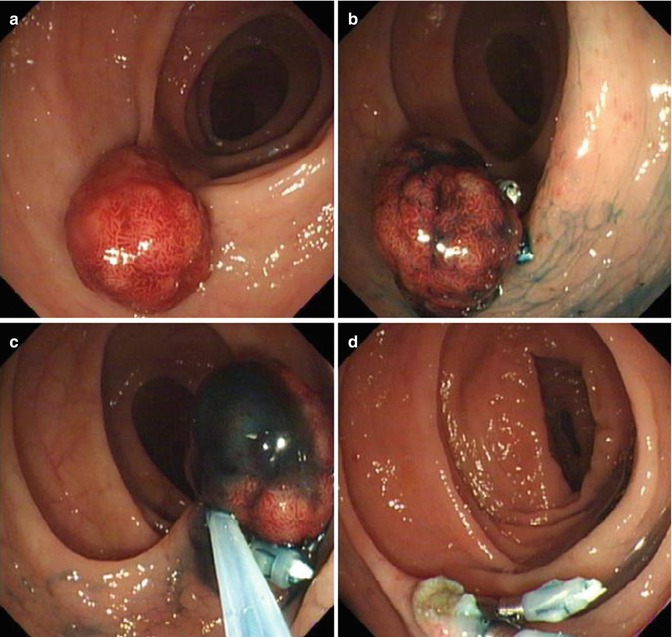
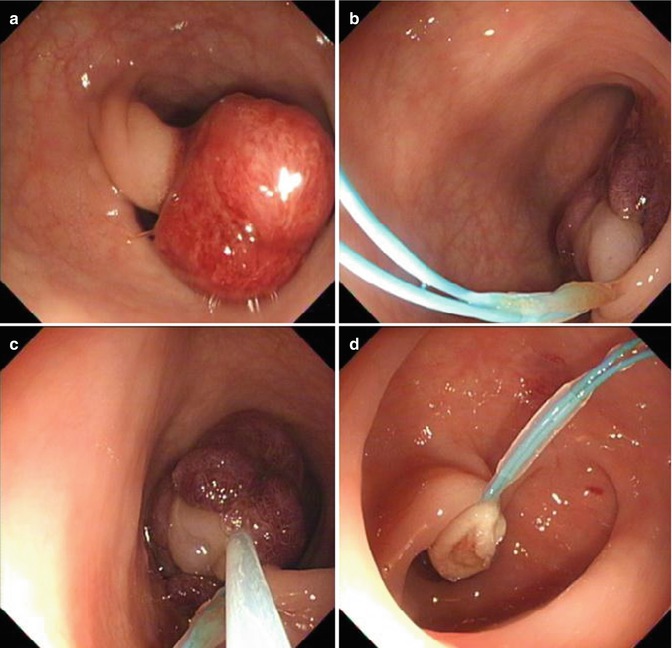
Fig. 3.7
Endoloop polypectomy of a thick-pedicle sigmoid colon polyp. (a) Apedunculated polyp with thick stalk and hyperemia mucosa. (b) An endoloop was applied in the middle of the stalk. (c) Snare ploypectomy was performed above the loop. (d) The wound after resection
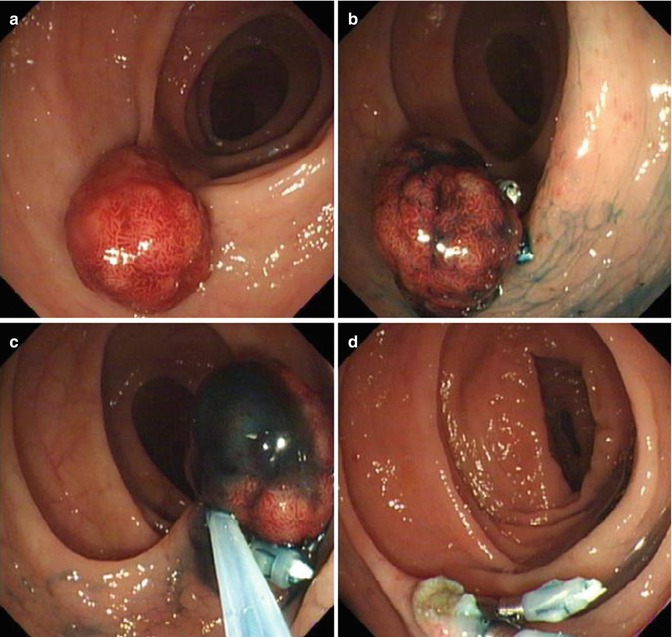
Fig. 3.8
Snare polypectomy of a massive descending colon polyp. (a) A pedunculated polyp was found in descending colon. (b) After observing it with methylene blue, metallic clips were applied to the stalk of it. (c) Snare polypectomy with electric current was performed. (d) Wound after resection
Some polyps are on an extremely long pedicle and can pose a problem for their removal because they tend to swing back and forth during the endoscopic examination. They are better to be ligated with endoloop 0.5–1 cm closer to the intestinal wall and be resected carefully (Fig. 3.9).
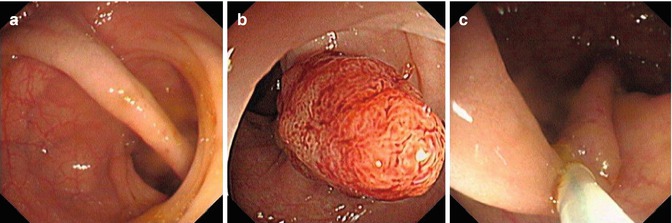
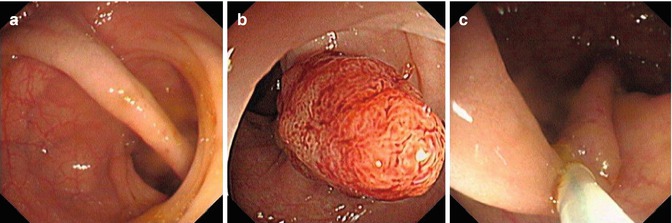
Fig. 3.9
Management of a polyp with an extremely long pedicle. (a) A long-pedicle polyp. (b) The head of the long-pedicle. (c) Endoloop was applied 1 cm from the wall
3.1.4.3 Sessile Polyps
Inappropriate resection by snare and cautery technique of sessile polyps has a great chance of bleeding and perforation. Therefore, it is better to place the snare slightly above the polyp base to perform the polypectomy in case the polyp is resected too deep into the tissue and even normal mucosa around the polyp is deeply resected, which gives rise to a higher rate of perforation. Coagulation before cutting can prevent over coagulation resulting in deep layer burns and perforation. Insufficient coagulation may cause risk of bleeding. Situation is quite tricky and should be dealt with delicately.
A comparatively safer way of removing a sessile polypis to inject saline to the base in order to lift the lesion and then perform the polypectomy (Fig. 3.10). Piecemeal polypectomy is a better approach for large sessile polyps and even in more than one session if the endoscopist finds it hard to remove the polyp all at once for safety concerns.
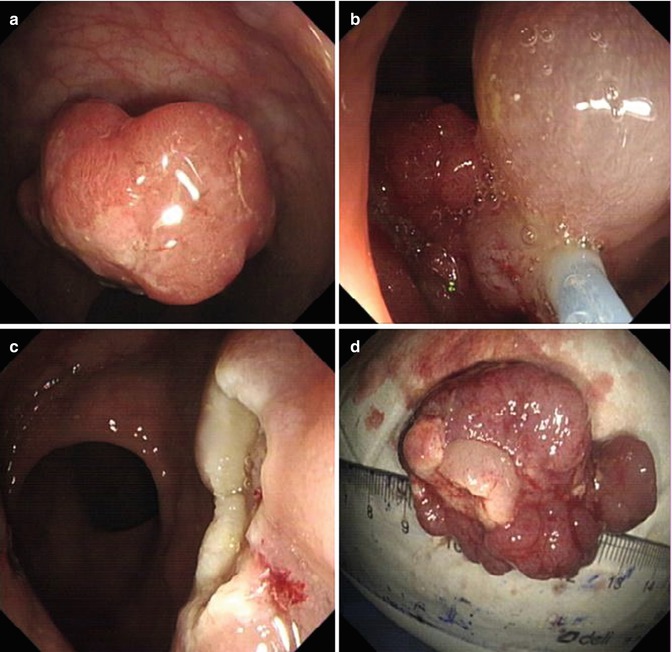
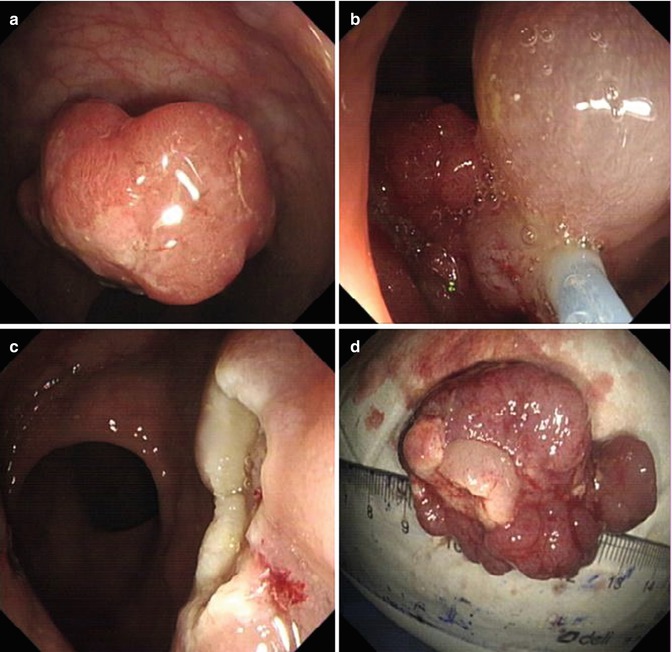
Fig. 3.10
Snare polypectomy of a rectum sessile polyp.(a) A sessile polyp in the rectum. (b) Snare polypectomy was performed for this lesion. (c) The polyp was resected completely. (d) The resected specimen
3.1.5 Techniques for Specimen Retrieval (Fig. 3.11)

Fig. 3.11
Retrieval techniques. (a) With snare. (b) Using grasping forceps. (c) Using retrieval net
A properly prepared pathologic examination of the specimen is the best and only way to assess and characterize the lesion and ensure complete resection.
A relatively simple method to retrieve small polyp specimen is to suct the polyp directly and aspirate the specimen into a trap. Disadvantage of this technique is that the aspiration may cause the specimen to be torn into smaller pieces, thus compromising pathologic examination of the remaining polyp. Suctioning the polyp onto the tip of the endoscope and taking it out along with withdrawal of the endoscope can be applied for some large polyps, however the view on withdrawal is reduced and chance of a good observation of the remaining colon is rather small. Therefore, small polyps are better to be collected by biopsy forceps and large polyps be retrieved by the use of a retrieval net or grasping forceps and removed along with withdrawals of the endoscope. A single polyp is easy to collect after polypectomy, while retrieval of multiple polyps is somehow troublesome since only one specimen can be taken out every time, and multiple insertions and withdrawals of the endoscope are required if the intention is to take out all the specimens.
3.1.6 Management of Complications
3.1.6.1 Hemorrhage
Bleeding is usually caused by insufficient coagulation particularly in some thick-pedicle lesions when vessels in the pedicle center have not been fully coagulated. Closing the loop of the snare too quickly, or too tightly particularly in thin-pedicle polyps can lead to mechanical transection (guillotine) of pedicle without adequate coagulation and thus leading to risk of bleeding. On the other hand, excessive coagulation may lead to delayed bleeding because of severe tissue burn resulting in deep ulcerations. Hence the ultimate key to prevent hemorrhage is to keep the snare tightened to a moderate degree as well as reasonable use of electro cautery.
Slight oozing after polypectomy generally does not require special management and mostly stops spontaneously. When severity of bleeding goes to dripping blood or pulsatile bleeding, actions have to be taken immediately. Endoloops ligation or metallic clips clamping should work for lesions with a residual pedicle. If residual stalk is present, it can be snared to stop bleeding. If there is no obvious pedicle, metallic clips can be applied to achieve hemostasis (Figs. 3.12 and 3.13).
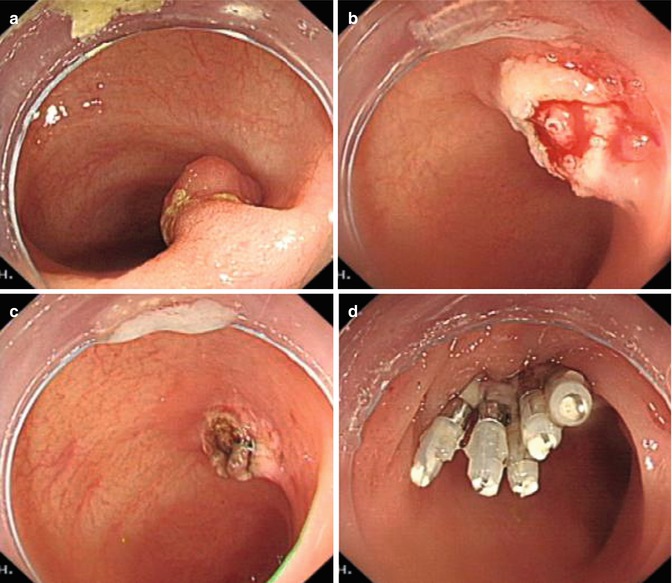
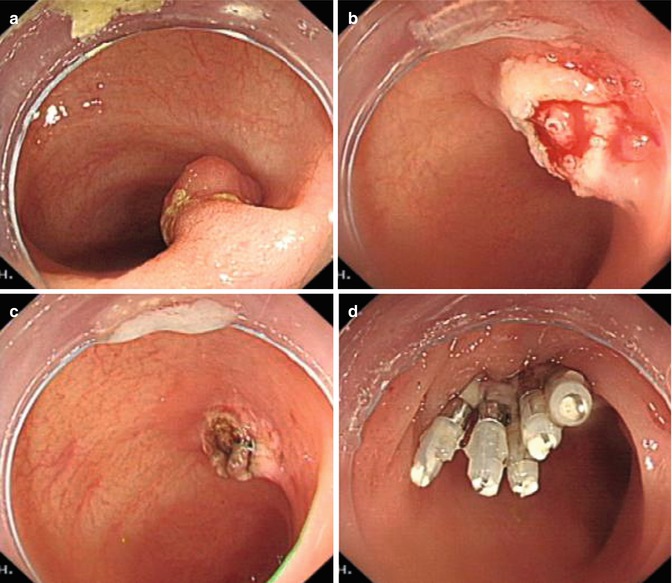
Fig. 3.12
Bleeding from the residual pedicle after polypectomy and successful hemostasis by coagulation and hemoclips. (a) Polyp before resection. (b) Active bleeding was oozing from a vessel in the middle of the pedicle. (c) Successful hemostasis was achieved. (d) metallic clips applied to close the wound