e-Figure 1.1
Which of the following is the best diagnosis for this esophageal biopsy submitted as “rule-out eosinophilic esophagitis”?
A. Amyloidosis underlying squamous mucosa
B. Squamous mucosa with mild graft versus host disease (GVHD)
C. Unremarkable squamous mucosa
D. Granular cell tumor undermining squamous mucosa
Answer: Amyloidosis underlying squamous mucosa (A).
Amyloidosis is an easily overlooked diagnosis owing to the pale and sometimes focal nature of the findings. Amyloid appears as amorphous, acellular eosinophilic material on H&E. Congo red staining can be utilized to confirm the diagnosis with amyloid-appearing bright orange under direct light, and apple-green when polarized. There are no apoptotic bodies, dyskeratotic keratinocytes, or prominent intraepithelial lymphocytes to suggest GVHD (B). Moreover, GVHD is a clinicopathologic diagnosis requiring the appropriate setting of bone marrow transplantation and typically a rash and GI symptoms, pertinent features lacking in this case. Granular cell tumors can have a low-power appearance similar to that of amyloid, but the eosinophilic material characteristic of granular cell tumor is more coarse (“granular”), confined within the cytoplasm, and S100 reactive (D). In contrast, amyloid deposition is extracellular, smooth and homogenous, and S100 nonreactive.
E-QUIZ QUESTION 2 (e-FIG. 1.2)
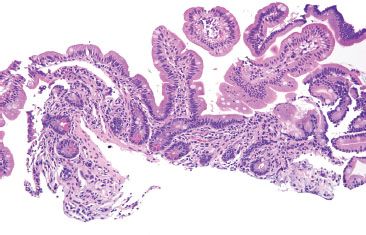
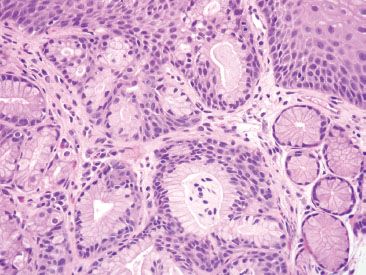
e-Figure 1.2
Which of the following is the best diagnosis for this biopsy labeled “distal esophagus” from a 13-year-old male with abdominal pain and an unremarkable endoscopic examination?
A. Cardiac mucosa with nondiagnostic findings
B. Barrett mucosa, negative for dysplasia
C. Low-grade dysplasia in Barrett mucosa
D. Eosinophilic esophagitis
E. Small bowel mucosa with nondiagnostic findings (“carry-over”)
Answer: Small bowel mucosa with nondiagnostic findings (“carry-over”) (E).
This case had been previously diagnosed as Barrett mucosa but was submitted to us for consultation based on the patient’s young age and the important clinical implications. While Barrett mucosa can (rarely) develop in children, not every goblet cell in an esophageal biopsy signifies Barrett mucosa. The diagnosis of Barrett mucosa requires both an abnormal endoscopic impression as well as goblet cells in the esophagus.1,2 Since this patient had an unremarkable clinical examination, the diagnosis of Barrett mucosa was not entertained. Moreover, there are several clues pointing to a small bowel “carry-over” artifact. First, the villiform architecture and the finding of Paneth cells in virtually each crypt are more in keeping with small bowel mucosa whereas Barrett mucosa usually has incomplete metaplasia and lacks Paneth cells and a brush border. In addition, the depicted duodenal mucosa is at the edge of the tissue block, suggesting it may represent a tissue “carry-over” artifact (e-FIG. 1.3). Such artifacts typically occur via contamination of the endoscopic or grossing instruments.

e-Figure 1.3
E-QUIZ QUESTION 3 (e-FIG. 1.4)
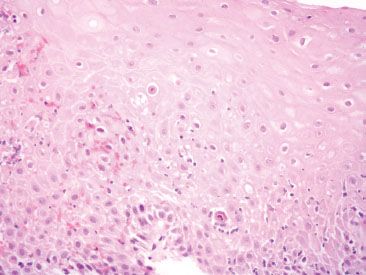
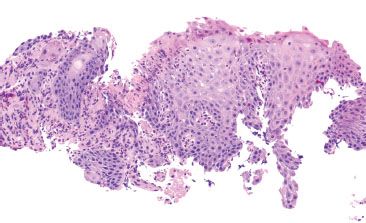
e-Figure 1.4
Which of the following is the best diagnosis for this esophageal biopsy from a 43-year-old man with a history of bone marrow transplantation, GI symptoms, and a skin rash?
A. Unremarkable squamous mucosa
B. Squamous mucosa with mild graft versus host disease (GVHD), grade I
C. Squamous mucosa with moderate GVHD, grade II
D. Squamous mucosa with severe GVHD, grade III
Answer: Squamous mucosa with moderate graft versus host disease (GVHD) (C).
General features of GVHD of the esophagus include intraepithelial lymphocytes, apoptotic bodies, dyskeratotic keratinocytes, and necrosis. The overall abundance of the changes are utilized to grade the GVHD as either mild (grade I), moderate (grade II), or severe (III). In this example, dyskeratotic keratinocytes and apoptotic bodies are easily identified such that they reach the threshold for moderate GVHD. Mild GVHD would have only occasional findings (not quite as conspicuous as moderate GVHD), and severe GVHD would have mucosal necrosis. In addition, medication injury and infectious etiologies can have similar histologic findings and consideration of these possibilities is worthwhile. Toward this end, a careful medication review and a low threshold to order CMV and HSV immunohistochemical stains on cases of possible GVHD is prudent.
E-QUIZ QUESTION 4 (e-FIG. 1.5)
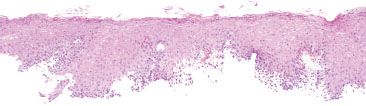
e-Figure 1.5
Which of the following is the best diagnosis given this low-power H&E impression?
A. Unremarkable squamous mucosa
B. Candidiasis
C. Eosinophilic esophagitis
D. Esophagitis dissecans superficialis
Answer: Candidiasis (B).
The image shows patchy parakeratosis, which should prompt a careful examination for candidiasis. Note the high-power view, which shows the diagnostic pseudohyphae embedded within the parakeratotic debris (circle, e-Fig. 1.6). Intraepithelial eosinophils and basal hyperplasia are absent, precluding consideration of eosinophilic esophagitis (C). Esophagitis dissecans superficialis is characterized by an often fragmented specimen with a “mummified” or “ghost” superficial squamous layer (D). Recall the following endoscopic “buzzwords” or characteristic endoscopic appearances for choices B–D.
• Candidiasis&emdash;white plaques
• Eosinophilic esophagitis&emdash;furrowing or felinization
• Esophagitis dissecans superficialis&emdash;a sloughing appearance with white sheets of tissue that appear to easily dislodge during the endoscopic examination
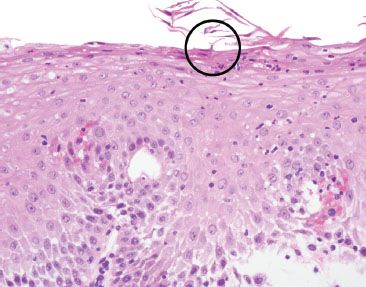
e-Figure 1.6
E-QUIZ QUESTION 5 (e-FIG. 1.7)
e-Figure 1.7
Which of the following is the best diagnosis for this esophageal biopsy from a 55-year-old man with a history of reflux and an irregular Z-line?
A. Cardiac mucosa with multilayered epithelium, negative for Barrett mucosa
B. Barrett mucosa, negative for dysplasia
C. Low-grade dysplasia in Barrett mucosa
D. Dysplasia in Barrett, basal crypt pattern
E. Pancreatic acinar metaplasia
Answer: Cardiac mucosa with multilayered epithelium (A), negative for Barrett mucosa.
This consultation case was submitted along with a preliminary diagnosis of intramucosal carcinoma in Barrett mucosa. However, the histologic features are those of multilayered mucosa, a common mimic of true goblet cells of the distinctive type. Multilayered mucosa bears resemblance to both squamous and glandular mucosa with pseudogoblet cells. The appearance is reminiscent of that of immature squamous metaplasia of the uterine cervix. A PAS/AB highlights the tinctorial appearance of the mucin in multilayered mucosa as a two-tone purple-blue color that is a cross between the character of true-goblet cells (deeply basophilic) and foveolar mucosa (magenta) (not shown). Some authors regard multilayered mucosa as the precursor to Barrett mucosa,3,4 but as of this writing here are no official recommendations on the diagnosis and management of multilayered epithelium.
E-QUIZ QUESTION 6 (e-FIG. 1.8)
e-Figure 1.8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








