| 8 | Diverticulosis and Diverticulitis |
 Definitions
Definitions
Colonic diverticula are fingerlike outpouchings protruding outward from the intestinal lumen.
True and pseudodiverticula. A distinction is made between true diverticula and pseudodiverticula. The seldom-occurring true diverticula are present at birth and usually only appear in the right hemicolon. Pseudodiverticula, which occur much more frequently, are acquired. They can be found anywhere in the colon, though they tend to appear in the left hemicolon. True diverticula are characterized by herniation of the entire colon wall, including the muscle layer. Pseudodiverticula are herniations of only mucosa and submucosa, through defects in the muscular coat. Thus, the walls of pseudodiverticula are thinner and less stable than those of true diverticula. While true diverticula usually only occur one at a time, pseudodiverticula normally occur in multiple. True diverticula and pseudodiverticula are not endoscopically distinguishable.
A further distinction can be made with regard to pseudodiverticula, which can be further divided into incomplete and complete diverticula. Incomplete diverticula include only mucosal and submucosal layers and remain intramural, located in the muscle layer, while complete diverticula protrude beyond the circular muscle layer.
Inflammation. The presence of colonic diverticula without any complications is referred to as (colonic) diverticulosis. Diverticulitis occurs if one or more diverticula become inflamed (generally symptomatic).
Diverticulosis
 Clinical Picture
Clinical Picture
Epidemiology. Colonic diverticulosis is a modern-day disease, first described by Cruveilhier in 1894. Since then, its prevalence has been increasing in industrialized countries, while remaining constant in developing nations. Mean frequency (combined age groups) in western industrialized nations is 20–40%; in Southeast Asia and Africa it is only 2–4%. Disease frequency is clearly associated with age: while diverticulosis seldom occurs among those under age 30, its prevalence among those over age 80 is 50–65%. Predisposition to diverticulosis has not been shown unequivocally to vary between men and women. However, in younger age groups, the disease appears to be slightly more common among men and in older age groups it appears to be more common among women.
Symptoms. Most individuals affected by diverticulosis remain asymptomatic over their lifetime; a minority of patients, 20–30%, exhibit clinically relevant complications (diverticulitis, stenosis, perforation, or bleeding). Nonspecific symptoms that may be related to diverticulosis include cramplike lower abdominal pain (usually located in the lower left abdomen), a feeling of fullness, bloating, and irregular bowel habits. Differentiation from diverticulitis is possible if these nonspecific symptoms are not accompanied by signs of inflammation. In some cases, it is impossible to differentiate between diverticulosis and irritable bowel syndrome and it is doubtful whether the symptoms are related to diverticulosis.
Etiology. Etiology and pathogenesis of diverticulosis are attributed to the low amount of fiber in the western diet, which leads to lower stool volume in the colon. This eventually causes a decrease in lumen diameter, which in turn increases wall tension of the colon according to the Laplace law. The sigmoid colon, in particular, can be affected, due to its intense contractions and high proportion of segmentation. Stool is condensed, thereby reducing stool volume in the sigmoid, and the width of the lumen is narrower than in the right hemicolon.
 Diagnosis
Diagnosis
Role of endoscopy. Diverticulosis is most often diagnosed using endoscopy or radiology with a contrast enema (Fig. 8.1). More recently, computed tomography has also been used. Diagnosis using sonography is also possible under good echo conditions. Especially in cases of less pronounced diverticulosis, diagnosis sometimes occurs incidentally during endoscopy or radiology of the colon or abdomen.
Colonoscopy is usually indicated as a diagnostic tool for known or suspected diverticulosis (more often for potential differential diagnoses than for main diagnosis), though it also can be used for treatment (Tab. 8.1). Endoscopic surveillance is not indicated for uncomplicated diverticulosis, not least due to risk of potential complications during endoscopy, but also given the lacking treatment corollary. Signs of acute diverticulitis are a contraindication for colonoscopy due to increased risk of perforation.

Fig. 8.1 Sigmoid diverticulosis, visible on radiographs with contrast enema.
Diagnostic indications | |
|---|---|
| symptoms of obstruction (alternating constipation and diarrhea, recent onset of constipation) |
| unexplained abdominal pain (if accompanied by signs of inflammation, first conduct radiological or sonographic examination for signs of diverticulitis) |
| prior hematochezia |
| unclear radiological findings (e.g., to determine malignant/benign nature of stenoses, exclude neoplasia for hypertrophied folds or stool particles) |
| preoperative to determine which colonic segments are affected by diverticula |
Treatment indications | |
| hematochezia |
| endoscopic treatment of postdiverticular stenoses (if surgical intervention has been declined or is considered to be risky due to accompanying disease) |

Fig. 8.2 Accordionlike lumen narrowing (myochosis) and thickened folds caused by hypertrophied circular muscles, diverticulosis in the sigmoid colon.

Fig. 8.3 Significant narrowing of the lumen (myochosis). Visualization into the haustra harboring the diverticula is made more difficult.

Fig. 8.4 Proximity of a diverticulum to a blood vessel, which is penetrating the circular muscle layer, causing a weakness in the colon wall.

Fig. 8.5 Close proximity of diverticulum and blood vessels. Slanted angle of entry of vessels into the wall and slanted path of diverticulum are clearly visible.

Fig. 8.6 Mild case of diverticulosis in sigmoid colon. Small, single diverticulum, soft folds, no significant myochosis.

Fig. 8.7 Moderate case of sigmoid diverticulosis. Several small diverticula, folds already somewhat thickened, no clinically relevant narrowing of the lumen yet.

Fig. 8.8 More severe case of sigmoid diverticulosis. Numerous diverticula, some already giant, folds are noticeably thickened, myochosis.
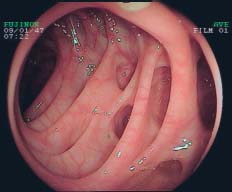
Fig. 8.9 Pronounced diverticulosis in the sigmoid. Many large or very large diverticula, lumen is severely narrowed, more difficult view into haustra.

Fig. 8.10 Diverticulosis of the ascending colon. Clearly recognizable ileocecal valve at right. Proximity of diverticulum to a blood vessel suggests a pseudodiverticulum.

Fig. 8.11 Diverticulosis at the hepatic flexure. The diverticula are still partly filled with feces.

Fig. 8.12 Diverticulum with impacted feces. Impacted feces impede bowel cleansing in patients with diverticulosis.

Fig. 8.13 Severely impacted and hardened stool (fecalith) in a diverticulum.
 On the one hand, lacking stool volume and resulting increased wall tension (see above) lead to hypertrophy of the circular muscle layer, which can be seen endoscopically as a thickening of the circular muscle folds with an accordionlike shortening of the lumen (also referred to as myochosis) (
On the one hand, lacking stool volume and resulting increased wall tension (see above) lead to hypertrophy of the circular muscle layer, which can be seen endoscopically as a thickening of the circular muscle folds with an accordionlike shortening of the lumen (also referred to as myochosis) (






 8.1), ranging from solitary, barely detectable diverticula to multiple giant diverticula involving nearly the entire colon. The changes to the folds and the degree of compression and deformation of the lumen (myochosis) also varies greatly.
8.1), ranging from solitary, barely detectable diverticula to multiple giant diverticula involving nearly the entire colon. The changes to the folds and the degree of compression and deformation of the lumen (myochosis) also varies greatly.











