Phosphorus/
Magnesium Homeostasis
CALCIUM
Physiology and Measurement
■ Normal daily dietary calcium intake in adults is ~1,000 mg; however, net gut absorption is about 100 to 200 mg. In the steady state, the absorbed calcium is excreted in the urine. Vitamin D increases gut absorption. Calcium plays an important role in the strengthening of bones and teeth, muscle contraction, nerve conduction, and blood clotting.
■ The vast majority (~99%) of total body calcium is stored in bone. Of the 1% extracellular calcium, ~50% is bound to albumin, with the remainder being free (ionized) calcium or complexed calcium (the latter is a small percentage and can usually be ignored for clinical purposes).
■ The normal plasma total calcium (Ca) is 8.5 to 10 mg/dL (2.125 – 2.5 mmol/L), and ionized calcium (Ca2+) about half that amount, that is, 4.25 to 5 mg per dL (1.0625 – 1.25 mmol/l). Since the molecular weight of calcium is 40, 1 mmol of calcium is 40 mg. Thus to convert mg/dL to mmol/L, divide by 0.1 × molecular weight (i.e., 4). Since calcium is divalent, to convert mmol/L to mEq/L, multiply by 2. Thus, a plasma-ionized calcium level of 5 mg/dL = 1.25 mmol/L = 2.5 mEq/L. All of these units are used in clinical practice.
■ Because of calcium–albumin binding, the plasma total calcium decreases by 0.8 mg per dL (0.2 mmol/L) for each 1.0 g per dL (10 g/L) decrease in plasma albumin. Hypoalbuminemia will not affect plasma-ionized calcium. However, ionized (but not total) calcium will fall if there is an increase in pH of the plasma, owing to enhance calcium–albumin binding.
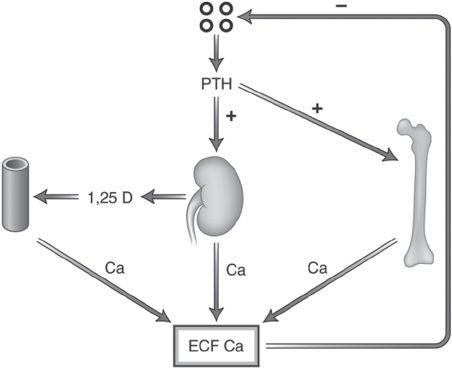
■ Plasma calcium is regulated by parathyroid hormone (PTH)/vitamin D. A decrease in plasma-ionized calcium increases PTH secretion, which mobilizes skeletal calcium, stimulates formation of 1α, 25-dihydroxyvitamin D, thus increasing gut calcium absorption, and decreases urinary calcium excretion. An increase in plasma-ionized calcium will have the opposite effects. These relationships are depicted in Figure 8.1. These effects occur very soon after the calcium level becomes low. The timeline is as follows:
■ Within seconds—PTH is secreted
■ Within hours to days—PTH synthesis is increased
■ Within weeks to months—parathyroid cell proliferation occurs
■ After many months—parathyroid glands may become autonomous, that is, tertiary hyperparathyroidism (Silver et al., 1996).
Disorders of Calcium Metabolism
■ Hypocalcemia
■ Hypoparathyrodism (decreases calcium release from bone)
• Autoimmune
• Hungry bone syndrome (Ca shifts into bone for remineralization S/P parathyroidectomy)
■ Vitamin D deficiency (decreases gut calcium absorption)
■ Gut malabsorption (e.g., intestinal disease)
FIGURE 8.1 Effects of PTH on calcium homeostasis. (From Kronenberg HM, Memed S, Polonsky KS, et al. Hormones and disorders of mineral metabolism. In: Williams Textbook of Endocrinology. 11th ed. Philadelphia, PA: Saunders; 2007:1024, with permission.)
■ Renal failure
• Deficient 1α,25-(OH)2-vitamin D production, decrease in the number of vitamin D receptors, and resistance to the action of vitamin D (Korkor, 1987). Phosphorus retention leads to an increase in fibroblast growth factor 23 (FGF23) production, which inhibits renal 1α-hydroxylase in the kidney.
• Hyperphosphatemia per se results in an increase in “calcium–phosphorus product” in blood and favors movement of calcium into tissues, particularly bone.
• Hypocalcemia associated with renal failure results in an increase in PTH secretion (secondary hyperparathyroidism). The typical laboratory constellation in secondary hyperparathyroidism in renal failure is thus low calcium, high phosphorus, and high PTH.
• Acute renal failure associated with rhabdomyolysis can lead to profound hypocalcemia, due to the severity of hyperphosphatemia (muscle breakdown releases phosphorus into the extracellular fluid) and deposition of calcium in damaged muscle.
■ Other less common causes of hypocalcemia include acute pancreatitis (calcium–fatty acid precipitation), hypomagnesemia (decreases PTH release and peripheral action), and certain medications (bisphosphonates, cinacalcet, citrate).
■ Hypercalcemia
■ Hyperparathyroidism:
• Primary hyperparathyroidism—increased calcium release from bone due to parathyroid adenoma
• Secondary hyperparathyroidism—In early secondary hyperparathyroidism, calcium is low. With prolonged disease, hypercalcemia may develop with adynamic bone disease and markedly reduced bone turnover. In such patients, hypercalcemia which develops with calcium-containing phosphate binders used to treat hyperphosphatemia is due to a marked reduction in the bone uptake of calcium
• Tertiary hyperparathyroidism—When maximum medical management fails to control the hyperparathyroidism and the parathyroids remain overactive for many months, tertiary hyperparathyroidism may result, that is, the parathyroids become autonomous. Tertiary hyperparathyroidism has been defined as hyperparathyroidism that fails to resolve with maximum medical management or as hyperparathyroidism that persists despite renal transplantation (McIntosh et al., 1966)
■ Vitamin D excess (increases gut calcium absorption) (Fetchick et al., 1986)
■ Malignancy (multiple mechanisms, including bone resorption, ectopic PTH secretion, secretion of PTH-related peptide)
■ Other less common causes of hypercalcemia include granulomatous disease (increased activity of renal 25-OH-vitamin D-1α hydroxylase with increased production of 1α,25-(OH)2-vitamin D), immobilization (increased calcium release from bone) (Stewart et al., 1982), Paget disease (increased bone turnover), thyrotoxicosis (increased calcium release from bone) (Mundy et al., 1976), familial hypercalcemic hypocalciuria (inactivating mutation of calcium-sensitive receptor in parathyroid glands and kidney tubules, leading to higher setpoint for plasma calcium to suppress PTH release and increased renal calcium reabsorption), and certain medications such as thiazides (decreased urinary calcium excretion) (Duarte et al., 1971), lithium (increased PTH release), and calcium plus alkali supplements (Burnett et al., 1949).
Symptoms and Signs of Hypocalcemia and Hypercalcemia
■ Hypocalcemia:
■ Perioral paresthesias
■ Carpopedal spasm (Trousseau sign if occurs after arterial occlusion with BP cuff)
■ Tetany
■ Chvostek sign (facial muscle twitching when tapping facial nerve at parotid gland)
■ Prolonged QT interval on electrocardiogram (EKG); congestive heart failure (Kazmi & Wall, 2007)
■ Hypercalcemia:
■ Constipation
■ Polyuria/polydipsia
■ Confusion
■ Coma (if severe)
■ Shortened QT interval on EKG
■ Osteitis fibrosa cystica (Silverberg et al., 1989)
Treatment of Hypocalcemia and Hypercalcemia
■ Hypocalcemia
■ Oral or intravenous (if symptomatic) calcium
■ Vitamin D (if indicated)
■ Hypercalcemia
■ Intravenous (IV) fluids (if volume depleted, increases urinary calcium excretion)
■ Furosemide (increases urinary calcium excretion) once volume replete; stop thiazides if being given
■ Bisphosphonates (prevent bone resorption)
■ Calcitonin (increases bone uptake of calcium)
■ Calcimimetics (activate calcium-sensitive receptor in parathyroid glands and kidney tubules, leading to lower set-point for plasma calcium to suppress PTH release and decreased renal calcium reabsorption), if appropriate
■ Dialysis (removes calcium) (indicated in severe hypercalcemia if coma present)
■ Consider parathyroidectomy if appropriate.
PHOSPHORUS
Physiology and Measurement
■ Recommended dietary phosphorus intake in adults is ~700 mg (Institute of Medicine Food and Nutrition Board). Intestinal phosphorus absorption is higher with inorganic phosphate additives (found in processed and “junk” foods) than with organic phosphates naturally found in “whole” foods, since the latter are bound to proteins and phytates that limit their absorption. Vitamin D increases phosphorus absorption.
■ Most (~ 80%) of total body phosphorus is stored in bone, with most of the remainder in cells in the form of phospholipids and phosphorylated intermediates.
■
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree