A subset of patients with chronic constipation, up to 50% at tertiary centers, have difficult defecation, which can be suspected by clinical features and confirmed by anorectal tests. Symptoms of difficult defecation (ie, defecatory disorders) may occur in isolation or in association with symptoms of irritable bowel syndrome. Patients with defecatory disorders may have normal or slow colonic transit. Defecatory disorders should be recognized early because pelvic floor retraining by biofeedback therapy is superior to laxatives for management.
Clinical Features
Among people with chronic constipation, clinical experience suggests that some symptoms, such as the excessive straining or the sense of anorectal obstruction/blockage during defecation and the use of manual maneuvers (ie, vaginal splinting or anal digitation) to facilitate defecation are suggestive of defecatory disorders. Other symptoms (eg, lumpy or hard stools, sensation of incomplete evacuation, less than3 defecations/week) are not. Moreover, symptoms should be interpreted in the context of stool consistency, which should be preferably characterized by asking patients to refer to a Bristol stool form scale. While normal people may experience difficulty in evacuating hard stools, difficulty in evacuating soft stools or enema fluid is particularly suggestive of defecatory disorders. Not infrequently, irritable bowel syndrome and pelvic floor dysfunction will coexist.
In defecatory disorders, inspection of the anal orifice may reveal anal fissures or large hemorrhoids in patients with pelvic floor dysfunction. Digital rectal examination can assess anal pressure at rest, when patients contract or squeeze their anal sphincter and pelvic floor muscles, and during simulated evacuation. Normally, simulated evacuation is accompanied by relaxation of the anal sphincter and puborectalis muscle and perineal descent by 1 to 4 cm ( Fig. 1 ). Patients with defecatory disorders have one or more abnormal findings, including anismus (ie, high anal resting pressure), reduced or excessive perineal descent (ie, ballooning of the perineum), and/or rectal prolapse. The puborectalis may not relax normally or, paradoxically, may contract during simulated evacuation. In my experience, relaxation of the puborectalis may not be perceptible even in patients with normal anorectal functions. Therefore, except for patients who have paradoxical puborectalis contraction, abnormal perineal descent, particularly if markedly reduced or absent, is more useful than impaired puborectalis relaxation for identifying defecatory disorders. Similar to anorectal testing, the digital rectal examination is influenced, to a greater extent in some patients than others, by the vagaries of trying to simulate defecation in the left lateral position in a physician’s office.
Nonetheless, 2 recent studies observed that a careful digital examination compared favorably to objective assessments of anorectal functions. In the first study, there was excellent agreement, as evidenced by a correlation coefficient of 0.8, between anal resting and squeeze pressures graded by the digital rectal examination scoring system (DRESS) and anorectal manometry in 383 patients with defecatory symptoms of whom 303 patients had a complete data set. In another cohort of 209 patients (191 men) with symptoms of chronic constipation, 134 of 183 patients (73%) with dyssynergia by anorectal manometry also had dyssynergia on a digital rectal examination (ie, “digital dyssynergia”). Digital dyssynergia was identified on the basis of the presence of 2 or more of the following features: impaired perineal descent, paradoxical anal contraction, or impaired push effort. Four patients, however, who had “digital dyssynergia” had normal manometry. Hence, a digital rectal examination was 75% sensitive and 87% specific for diagnosing dyssynergia as predicted by manometry; the corresponding positive and negative predictive values were 97% and 37%, respectively. Among 94 patients who had an abnormal balloon expulsion test, which is the most sensitive and specific test for diagnosing rectal evacuation disorder, 75 (80%) of patients had digital dyssynergia. But 59 of 115 patients (51%) with a normal balloon expulsion test also had “digital dyssynergia”; hence a digital exam was 56% specific relative to rectal balloon expulsion. While there was good agreement (>85%) between the digital rectal examination and manometry for identifying a normal anal resting and squeeze pressures, agreement for identifying weak resting and squeeze pressures was fair (approximately 50% to 55%). In summary, a digital rectal examination is useful for assessing anal functions, should be interpreted in the context of symptoms, and when necessary, particularly in patients with suspected defecatory disorders, confirmed by anorectal manometry. In chronic constipation, a normal test is more useful than an abnormal test.
Anorectal Tests
Anorectal tests should be performed in constipated patients who do not respond to simple laxatives, or even earlier, in patients who have symptoms and signs of difficult defecation. In most patients, anorectal manometry and a rectal balloon expulsion test suffice to confirm or exclude defecatory disorders. In selected circumstances (ie, when only one test is abnormal, when pelvic organ prolapse or a large rectocoele is suspected, or when there is a discrepancy between the clinical features and these anorectal tests), barium or magnetic resonance (MR) defecography is necessary to break the tie.
The rectal balloon expulsion test is a very simple, sensitive, and specific test for diagnosing defecatory disorders. Patients are asked to expel a 4-cm rectal balloon filled with 50 ml of warm water while seated on a commode; normally this requires less than 1 minute; patients with defecatory disorders require more time or cannot expel the balloon. Alternatively, patients are asked to expel a rectal balloon, connected over a pulley to weights, in the left lateral decubitus position; patients with pelvic floor dysfunction require more external traction to expel the balloon. Perception of the desire to defecate is essential prior to normal defecation. Some patients with defecatory disorders have reduced rectal sensation. While most laboratories inflate a rectal balloon by a standard volume, typically 50 ml, it has been suggested that when rectal sensation is reduced, patients may not perceive the desire to defecate at a volume of 50 ml, limiting their ability to evacuate the balloon even though rectal evacuation is preserved. An alternative approach is to inflate the balloon by increasing volumes until patients experience the desire to defecate. These 2 techniques (ie, fixed versus variable balloon inflation) of assessing rectal evacuation have not been compared in patients.
Anal manometry may reveal a high anal resting pressure or anismus (ie, 90 mm Hg or greater) in defecatory disorders. A reduced rectoanal pressure gradient, expressed as the ratio or the difference between rectal and anal pressure, during simulated evacuation, is also used to identify disordered rectal evacuation. However, in my experience, this measure is not as useful as a balloon expulsion test since (1) dyssynergia did not predict an abnormal rectal balloon expulsion test in healthy people, (2) many asymptomatic people also have an “abnormal” gradient during simulated evacuation, and (3) there is considerable overlap in the rectoanal pressure gradient between health and defecatory disorders and, among constipated patients, between patients who have and do not have a defecatory disorder. Hence, further studies to evaluate the utility of the rectoanal pressure gradient for identifying defecatory disorders are necessary. Except for Hirschsprung’s disease, the rectoanal inhibitory reflex is preserved in chronic constipation.
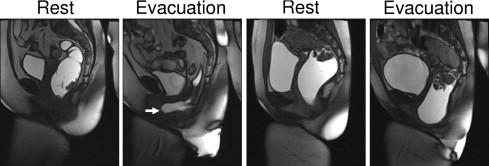
Barium or MR defecography can identify structural abnormalities (eg, rectocele, enterocele, and rectal prolapse) and evaluate anorectal motion by measuring various parameters (ie, anorectal angle, perineal descent, anal diameter, puborectalis indentation and rectal contents) at rest, during voluntary contraction, and during rectal evacuation. Barium defecography should be performed with barium paste rather than liquid barium and radiologists should be encouraged to measure anorectal parameters in addition to providing an overall impression. It can be challenging to measure these parameters because the bony landmarks necessary for making these measurements may not be clearly visible. Hence, perineal descent is measured relative to markings on a commode. MR defecography overcomes this limitation and, in contrast to barium defecography, does not entail radiation exposure, and also visualizes bladder and urogenital prolapse. In a controlled study, MR defecography identified disturbances of evacuation and/or squeeze in 94% of patients with suspected defecation disorders. In addition to examining the images, I also find it useful to review real-time images of the defecography.
While these anorectal tests are useful for identifying defecatory disorders, there are several caveats to interpreting test results. First, these tests may be abnormal even in asymptomatic people. Second, the literature suggests there is a relatively poor correlation among various tests (eg, anorectal manometry and defecography) in patients with defecatory disorders and that there is no true gold standard diagnostic test. Third, it is my perception that some patients with clinical features of pelvic floor dysfunction have seemingly normal rectal evacuation by testing, perhaps because they strain excessively to overcome increased pelvic floor resistance. Thus, an integrated assessment of clinical features and anorectal tests is necessary to confirm or exclude defecation disorders.
Anorectal Tests
Anorectal tests should be performed in constipated patients who do not respond to simple laxatives, or even earlier, in patients who have symptoms and signs of difficult defecation. In most patients, anorectal manometry and a rectal balloon expulsion test suffice to confirm or exclude defecatory disorders. In selected circumstances (ie, when only one test is abnormal, when pelvic organ prolapse or a large rectocoele is suspected, or when there is a discrepancy between the clinical features and these anorectal tests), barium or magnetic resonance (MR) defecography is necessary to break the tie.
The rectal balloon expulsion test is a very simple, sensitive, and specific test for diagnosing defecatory disorders. Patients are asked to expel a 4-cm rectal balloon filled with 50 ml of warm water while seated on a commode; normally this requires less than 1 minute; patients with defecatory disorders require more time or cannot expel the balloon. Alternatively, patients are asked to expel a rectal balloon, connected over a pulley to weights, in the left lateral decubitus position; patients with pelvic floor dysfunction require more external traction to expel the balloon. Perception of the desire to defecate is essential prior to normal defecation. Some patients with defecatory disorders have reduced rectal sensation. While most laboratories inflate a rectal balloon by a standard volume, typically 50 ml, it has been suggested that when rectal sensation is reduced, patients may not perceive the desire to defecate at a volume of 50 ml, limiting their ability to evacuate the balloon even though rectal evacuation is preserved. An alternative approach is to inflate the balloon by increasing volumes until patients experience the desire to defecate. These 2 techniques (ie, fixed versus variable balloon inflation) of assessing rectal evacuation have not been compared in patients.
Anal manometry may reveal a high anal resting pressure or anismus (ie, 90 mm Hg or greater) in defecatory disorders. A reduced rectoanal pressure gradient, expressed as the ratio or the difference between rectal and anal pressure, during simulated evacuation, is also used to identify disordered rectal evacuation. However, in my experience, this measure is not as useful as a balloon expulsion test since (1) dyssynergia did not predict an abnormal rectal balloon expulsion test in healthy people, (2) many asymptomatic people also have an “abnormal” gradient during simulated evacuation, and (3) there is considerable overlap in the rectoanal pressure gradient between health and defecatory disorders and, among constipated patients, between patients who have and do not have a defecatory disorder. Hence, further studies to evaluate the utility of the rectoanal pressure gradient for identifying defecatory disorders are necessary. Except for Hirschsprung’s disease, the rectoanal inhibitory reflex is preserved in chronic constipation.
Barium or MR defecography can identify structural abnormalities (eg, rectocele, enterocele, and rectal prolapse) and evaluate anorectal motion by measuring various parameters (ie, anorectal angle, perineal descent, anal diameter, puborectalis indentation and rectal contents) at rest, during voluntary contraction, and during rectal evacuation. Barium defecography should be performed with barium paste rather than liquid barium and radiologists should be encouraged to measure anorectal parameters in addition to providing an overall impression. It can be challenging to measure these parameters because the bony landmarks necessary for making these measurements may not be clearly visible. Hence, perineal descent is measured relative to markings on a commode. MR defecography overcomes this limitation and, in contrast to barium defecography, does not entail radiation exposure, and also visualizes bladder and urogenital prolapse. In a controlled study, MR defecography identified disturbances of evacuation and/or squeeze in 94% of patients with suspected defecation disorders. In addition to examining the images, I also find it useful to review real-time images of the defecography.
While these anorectal tests are useful for identifying defecatory disorders, there are several caveats to interpreting test results. First, these tests may be abnormal even in asymptomatic people. Second, the literature suggests there is a relatively poor correlation among various tests (eg, anorectal manometry and defecography) in patients with defecatory disorders and that there is no true gold standard diagnostic test. Third, it is my perception that some patients with clinical features of pelvic floor dysfunction have seemingly normal rectal evacuation by testing, perhaps because they strain excessively to overcome increased pelvic floor resistance. Thus, an integrated assessment of clinical features and anorectal tests is necessary to confirm or exclude defecation disorders.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




