Diagnostic Techniques
HISTORY AND PHYSICAL EXAMINATION
The history is the foundation of all diagnosis and should be performed in a systematic and orderly fashion to avoid errors of omission. This cannot be overemphasized. History taking should be tailored to the patient’s chief complaint and should include a review of major signs and symptoms of genitourinary disease, as well as a general review of systems. Patients with voiding complaints should be asked to provide a voiding diary. In a voiding diary, the patient records the time and amount of each void for 48 hours and any incontinence episodes. A record of time and amount of fluid intake can also be very valuable in understanding the patient’s voiding problem. A careful study of a patient’s input/output voiding diary can often prevent an expensive and unnecessary urodynamic study.
Historical Data
Voiding problems:
Storage (irritative) symptoms (frequency, urgency, and nocturia)
Voiding (obstructive) symptoms (hesitancy, straining, dysuria, slow, weak, or intermittent stream, terminal dribbling, and retention); incontinence (get details)
Input/output voiding diary for 48 hours
Urethral discharge (onset, color, consistency, and last sexual contact)
Pain with urination (dysuria)
Hematuria (when started, how much, how often, color, associated pain)
Bloody ejaculation
Fever, chills, and flank pain
Pyuria and pneumaturia
Sexually related problems
Past history of genitourinary problems—kidney, bladder, prostate, infections, stones, or difficulty in urinating
General past medical history with review of systems (cardiorespiratory, hypertension, diabetes, neurologic, gastrointestinal, and careful review of medications and allergies)
Physical Examination
Abdomen—pain or tenderness, palpable masses, auscultation for bruits, palpate for bladder distension, costovertebral angle tenderness
Hernias—umbilical or inguinal hernias
Penis—discharge, foreskin, palpable plaques, and meatus
Testes—size, tenderness, palpable masses, hydrocele, spermatocele, varicocele, transillumination, and beading of vas
Vaginal examination—discharges, cystocele, rectocele, enterocele, prolapse, bimanual palpation
Rectal examination—sphincter tone, prostate (size, consistency, nodules, mobility, and tenderness)
Skin lesions—morphology and distribution
URINALYSIS
Urinalysis is the single most important screening test available to the urologist and includes both chemical and microscopic components.
Urine Collection
Proper urine collection is necessary for accurate interpretation of urinalysis or culture. All tests must be performed on a freshly voided specimen. Urine that has been left standing becomes alkaline, with lysis of red blood cells, disintegration of casts, formation of crystals, and proliferation of bacteria. If it is not possible to examine the urine promptly, it should be refrigerated.
▪ Males
A voided, midstream clean-catch urine sample is routine; however, split voided specimens are sometimes helpful in localizing the source of infection or hematuria (see section “Technique for Urine Specimen Localization”).
▪ Females
▪ Infants
Suprapubic needle aspiration is usually the only effective method for obtaining a noncontaminated specimen for culture. A sterile plastic bag over the genitalia can be used for a routine urinalysis.
Gross Inspection
Color and appearance should be noted. Normal urine is pale urine but is affected by the patient’s hydration status. A cloudy or milky appearance can be due to the precipitation of phosphates (phosphaturia) in alkaline urine, pyuria, or, rarely, chyluria. Amorphous phosphates are frequently seen in the urine grossly and microscopically after meals.
Specific Gravity
Specific gravity (SG), measured by hydrometer or refractometer, can give a good estimate of the patient’s hydration, barring significant renal impairment. The normal range is 1.003 to 1.030. Glucose, protein, or intravenous contrast agents in the urine can cause a falsely elevated value. An SG >1.020 indicates concentrated urine and a fixed SG of 1.010 indicates renal insufficiency.
Chemical Dipstick
The urine dipstick permits simultaneous performance of a battery of useful chemical tests in <2 minutes. These are screening tests, and positive results generally need confirmation by other more precise tests. Faulty dipstick results can be caused by mixing of chemicals from adjacent pads as a result of excess urine on the dipstick or holding the dipstick in a vertical position. Do not use outdated dipsticks or allow them to sit out exposed to air or light for extended periods.
▪ pH (Range 4.5-9)
Urine pH is normally slightly acidic, except after a meal. A highly alkaline pH (>7.5) suggests infection with a urea-splitting organism such as Proteus.
▪ Protein
Qualitative protein estimation by the dipstick can be a tip-off to significant renal diseases, such as glomerular, tubulointerstitial, and renovascular diseases. Some other causes of positive protein readings include urologic cancer, multiple myeloma, white cells, vaginal secretions, prolonged fever, and readings after excessive exercise. Positive dipstick results should be quantitated with a 24-hour urine collection (normal <200 mg/day).
▪ Glucose
Normally, all filter glucose is reabsorbed by the proximal tubules. Urinary glucose detection indicates serum glucose levels above 180 mg/dL. Glucose determination by dipstick is both sensitive and specific; positive readings generally indicate diabetes mellitus.
▪ Hemoglobin
Hemoglobin by dipstick is not specific for red cells; however, it is a good screening test. Positive results suggest more than three red blood cells per high power field (hpf). Free hemoglobin and myoglobin can cause false-positive results. False-positive dipstick hematuria can occur from urine concentration in a dehydrated patient, excessive exercise, or contamination from menstrual blood. Dipstick hematuria must be confirmed by microscopic examination.
▪ Leukocyte Esterase and Nitrite Tests
The leukocyte esterase and nitrite tests are used to screen for urinary tract infection (UTI) in the nonurologic medical setting. Leukocyte esterase is produced by neutrophils and nitrates are converted to nitrites by gram-negative bacteria. Thus, the finding of positive leukocyte esterase and nitrites by dipstick suggests a UTI; however, microscopy for white blood cells and urine culture is the preferred method of diagnosing a UTI.
Microscopic Examination
Microscopy of the centrifuged urinary sediment is essential for every urinalysis.
▪ Procedure
Ten milliliters fresh urine is centrifuged at 3,000 rpm for 3 to 5 minutes. Nearly all supernatant is removed by turning the tube upside down. After returning to the upright position, the centrifuge
tube is tapped to resuspend the sediment. This suspension is then tapped onto the glass slide and covered with a coverslip.
tube is tapped to resuspend the sediment. This suspension is then tapped onto the glass slide and covered with a coverslip.
▪ Microscopy
Microscopy is first performed at low power (100× magnification, i.e., 10× objective) looking specifically for cells, casts, bacteria, crystals, yeasts, or trichomonads. Once any of these elements is observed, then high power (400× magnification, i.e., 40× objective) should be used for specific identification. Adjust the microscope to increase contrast by minimizing the condenser aperture. This improves visualization of fine detail. The approximate volume of urine under a coverslip at high-power magnification is 1/20,000 to 1/50,000 of a milliliter.
Red Blood Cells
Red blood cells in the urine can be differentiated into two morphologic types: urothelial and glomerular. The distinction indicates where the erythrocytes arose. Urothelial red blood cells suggest bleeding from urothelium such as from urothelial or renal parenchymal cancer, stones, or infection, while glomerular red blood cells suggest bleeding from non-neoplastic renal parenchymal disease such as glomerulonephritis.
Urothelial red blood cells are regular with smooth, rounded, or crenated membranes and an even hemoglobin distribution. As few as one per hpf suggests urologic disease.
Glomerular red blood cells are dysmorphic with irregular shapes and cell membranes and minimal or uneven hemoglobin distribution. More than 1,000,000 are normally excreted in the urine over a 24-hour period. The upper limit of normal is 1,000/mL urine or one for every two hpf. Two or more per hpf suggest glomerular disease.
White Blood Cells
Generally more than 5 to 8 white blood cells per hpf are considered abnormal (pyuria) in a properly collected specimen. This finding would justify empirical therapy in a patient with symptoms of infection. Clumping suggests a more severe inflammatory response. Causes of pyuria include UTI (pyelonephritis, cystitis, prostatitis, urethritis, etc.), renal tuberculosis (sterile pyuria), and urolithiasis.
Casts
Casts are formed in the distal tubules and collecting ducts from a mucoprotein matrix of the Tamm-Horsfall protein and
cellular elements. They generally signify intrinsic renal (nephron) disease.
cellular elements. They generally signify intrinsic renal (nephron) disease.
Red blood cell casts are diagnostic of glomerular bleeding (i.e., glomerulonephritis).
White blood cell casts are rarely seen but suggest pyelonephritis. Peroxidase staining is necessary to confirm that they are indeed polymorphonuclear leukocytes.
Granular casts (coarse, fine, and waxy) represent sloughed renal tubular epithelial cells and indicate intrinsic renal tubular disease.
Squamous Epithelial Cells
Squamous epithelial cells are common in the sediment in females and arise from the distal urethra and vagina.
Bacteria and Yeasts
As few as one bacterium per hpf in a strict, properly collected specimen indicates bacteriuria. Five bacteria per hpf indicate colony counts of about 100,00/mL. Candida albicans‘ characteristic budding hyphae is the most common yeast found in urine usually in diabetics.
Crystals
Crystals in the urine suggest stone disease. Calcium oxalate, uric acid, and cystine crystals precipitate in acidic urine, while calcium phosphate and triple-phosphate (struvite) crystals precipitate in alkaline urine.
URINE CULTURE
The presumptive diagnosis of a UTI based on symptoms and urinalysis should be confirmed by culture. Culture of a properly collected urine specimen (as described above) will provide identification, quantification, and specific antimicrobial sensitivities for the offending pathogen. Urine should be cultured immediately or within 24 hours of immediate refrigeration.
Bacterial Count
Cultures are read after 24 hours of incubation as the number of colony forming units per milliliter of urine. Final culture results are complete including antibiotic sensitivity testing 48 hours after incubation. Infection is defined as 103 to 105 bacteria per milliliter in a properly collected specimen.
Technique for Urine Specimen Localization
Collecting the urine specimen in specific segmented samples is useful for localizing the source of a UTI or inflammatory process in males. Ensure that the patient has a full bladder and that the glans is properly prepared. Collect each specimen into a separate sterile container.
VB1—collect the first 10 mL voided (urethral sample)
VB2—collect a midstream sample after patient has voided about 200 mL (bladder sample)
Stop voiding
EPS—massage prostate and collect drops of prostate secretions (prostatic sample)
VB3—again have patient void immediately and collect first 10 mL (prostatic sample)
LABORATORY TESTS
Serum Creatinine
Serum creatinine is a simple measurement that accurately reflects the glomerular filtration rate (GFR). Creatinine is a metabolic product of creatine phosphate in the skeletal muscle. The daily production is relatively stable for a given individual and is proportional to muscle mass. Creatinine clearance occurs mainly by glomerular filtration (90%) and, to a lesser extent, by tubular secretion (10%). Thus, creatinine clearance approximates GFR, and a doubling of serum creatinine indicates a 50% reduction in GFR. As individual nephrons (out of the 1,000,000/kidney) are lost to disease, the remainder hypertrophy, and single nephron GFR increases to maintain the overall GFR. A loss of 40% to 50% of renal mass is required before GFR begins to fall and creatinine rises. Note—a normal creatinine in a term infant is only 0.1 to 0.4 mg/dL because of low muscle mass.
Blood Urea Nitrogen
Urea is a metabolic product of protein catabolism that is excreted by the kidneys. Blood levels tend to reflect GFR but can be influenced by dietary protein intake, hydration, gastrointestinal bleeding, and glucocorticoids. The blood urea nitrogen/creatinine ratio, which is normally 10:1, can be a useful indicator.
▪ Conditions with Elevated BUN/Creatinine Ratio
Dehydration
Prerenal azotemia
Urinary tract obstruction
Blood in gastrointestinal tract
Increased tissue catabolism
Increased dietary protein intake
Treatment with glucocorticoids
Prostatic Acid Phosphatase
Acid phosphatase is an enzyme produced by various body tissues; however, the prostate is noted to be the most concentrated source. Human prostatic acid phosphatase (PAP) is a glycoprotein of 102,000 MW. Routine enzymatic serum assays specific for PAP utilize thymolphthalein phosphate as substrate. Blood samples should be chilled immediately after collection to avoid loss of enzyme activity. An elevated serum enzymatic PAP suggests metastatic disease. Routine use of PAP has been essentially replaced by prostate-specific antigen (PSA).
Prostate-Specific Antigen (hK3)
PSA is a 34-kDa glycoprotein found only in the cytoplasm of prostatic epithelial cells. It is a protein product of the human kallikrein gene family identified as hKLK3 or hK3. It is believed to function as a neutral serine protease that lyses seminal coagulum. It can be detected in the semen and serum of males with prostate tissue. It cannot be detected in females. PSA exits in serum both free and complexed (cPSA) to protease inhibitors.
PSA is specific only for prostate tissue and cannot differentiate benign from malignant prostate conditions. However, levels correlate with prostate size and the presence of prostate cancer. In addition, men with prostate cancer have a greater fraction of PSA complexed to serum proteins (cPSA). Normal levels of PSA are age dependent (see chart) and can be affected by androgen levels. In addition to prostate cancer, serum PSA levels can be elevated by acute prostatitis, vigorous prostatic manipulation or surgery, and markedly enlarged benign prostate glands. Serum PSA has been utilized extensively in prostate cancer for early detection, staging, and monitoring response to therapy. Serum PSA screening remains the best means for detecting early prostate cancer. PSA levels above 10 ng/mL are highly suspicious for the
presence of prostate cancer, even in males with a normal digital rectal examination. However, 20% of men with prostate cancer have a normal PSA.
presence of prostate cancer, even in males with a normal digital rectal examination. However, 20% of men with prostate cancer have a normal PSA.
▪ Age-Specific Guidelines for PSA Normal Levels | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Percent Free Prostate-Specific Antigen
The percent free PSA is a useful adjunct for differentiating a benign from malignant source of PSA when the PSA level is between 4.0 and 10.0 ng/mL. A low percent free PSA (<10%) increases the likelihood that prostate cancer is present while a high percent free PSA (>30%) favors a benign prostate. Direct measurement of cPSA levels provides equivalent prostate cancer detection specificity.
Prostate-Specific Antigen Velocity
The rate of change of PSA or PSA velocity has been shown to be useful for early detection of prostate cancer. A PSA velocity >0.7 ng/mL per year averaged over at least 18 months with three repeated PSA measurements is associated with an increased detection of prostate cancer.
Prostate-Specific Antigen Density
The ratio of serum PSA to prostate volume measured by prostate ultrasound is related to the chance of detecting prostate cancer on biopsy. A PSA density >0.1 has been suggested to be a useful marker for indicating prostate biopsy.
Alkaline Phosphatase
Alkaline phosphatase is an enzyme produced by many tissues, especially bone, liver, intestine, and placenta. Most enzymes present in normal serum is derived from metabolic activity in the
bone. Prostate cancer metastatic to the bone causes an elevation in alkaline phosphatase secondary to increased metabolic activity in the bone surrounding the metastatic lesion. When an elevated total alkaline phosphatase is in question, the bone derived isoenzyme can be isolated by its heat lability (bone burns). If the enzymatic activity of the heated fraction is <30% of the total, it suggests bone as the origin (bone isoenzyme is inactivated by heating).
bone. Prostate cancer metastatic to the bone causes an elevation in alkaline phosphatase secondary to increased metabolic activity in the bone surrounding the metastatic lesion. When an elevated total alkaline phosphatase is in question, the bone derived isoenzyme can be isolated by its heat lability (bone burns). If the enzymatic activity of the heated fraction is <30% of the total, it suggests bone as the origin (bone isoenzyme is inactivated by heating).
Lactate Dehydrogenase
Lactic acid dehydrogenase (LDH) is a cellular enzyme found in a number of different tissues. Elevated LDH can be found in germ cell tumors (GCTs).
24-Hour urine Collection
A 24-hour collection is often necessary for the workup of stone-forming patients and for an accurate assessment of renal function or proteinuria in a patient with renal disease. The most common reason for inaccuracy of values obtained from a 24-hour urine collection is due to incomplete collection. An incomplete collection is suggested by an inadequate amount of total creatinine in the sample because the total amount of creatinine excreted in 24 hours is dependent on muscle mass and is generally constant. The normal production of creatinine is 1.0 mg/kg/hour.
▪ Stone Risk Workup
A 24-hour urine collection for calcium, phosphorus, oxalate, magnesium, citrate, and uric acid is standard in the evaluation of the repeat stone former. Results can help plan stone prevention regimens.
▪ Creatinine Clearance
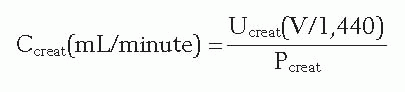
Creatinine clearance can be calculated from a 24-hour urine collection by knowing the volume of urine in milliliters per 24 hours (V), urine creatinine concentration in milligrams per milliliter (Uc), plasma creatinine concentration in milligrams per milliliter (Pc), and the following formula: (1,440 minutes/24 hour)
Creatinine clearance can be estimated without a 24-hour urine collection simply by knowing the patient’s age, sex, weight, and serum creatinine and using the following formula:
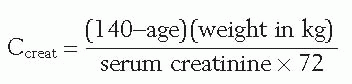
Multiply answer by 0.85 for females.
This formula is invalid in the setting of acute renal failure because its application requires a stable serum creatinine (steady state).
▪ Proteinuria
Normal 24-hour protein excretion is <200 mg. Heavy proteinuria (>2 g/day) is suggestive of renovascular, glomerular, or tubulointerstitial disease.
Urinary Electrolytes
Spot urinary sodium (Na) and potassium (K) measurements can be a valuable tool in diagnosing hypovolemia or prerenal azotemia. The kidney has an impressive capacity to hold onto sodium.
Human Chorionic Gonadotropin
Human chorionic gonadotropin (hCG) is a 38,000 MW doublechain glycoprotein with α- and β-subunits normally secreted by the syncytiotrophoblastic cells of the placenta. The α-subunit of hCG resembles that found in leutinizing hormone, follicle-stimulating hormone, and thyroid-stimulating hormone. The β-subunit is structurally unique and is used for antigenic detection. hCG is normally secreted during pregnancy. It has a metabolic half-life of 24 to 36 hours, and normal adult levels should be <5 mIU/mL. Elevated levels of hCG are detected in patients with GCTs: all patients with choriocarcinoma, in 40% to 60% of embryonal carcinomas, and in 5% to 10% of pure seminomas.
α-Fetoprotein
α-Fetoprotein (AFP) is a 70,000 MW single-chain glycoprotein normally secreted by the fetal yolk sac. It is also produced by trophoblastic cells of embryonal carcinoma and yolk sac tumors. It is not made by pure choriocarcinoma or seminoma. Elevated AFP is found in 50% to 70% of nonseminomatous testis tumors.
It has a half-life of 5 to 7 days, and normal adult levels should be <40 ng/mL (see Chapter 26).
It has a half-life of 5 to 7 days, and normal adult levels should be <40 ng/mL (see Chapter 26).
IMAGING TECHNIQUES
Roentgen Rays and Radiation
X-rays are electromagnetic waves of energy created when highspeed electrons hit the tungsten target of an x-ray tube. They are invisible because they have a shorter wavelength than visible light, which also gives them their greater penetrating ability. X-rays can produce an image on photographic film or fluorescent detectors, which accounts for their value in medical imaging. An x-ray is ionizing energy or radiation owing to its ability to liberate electrons from atoms and thus can have a detrimental affect on biologic matter.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




