CHAPTER 7 CYSTIC DISEASE OF THE LIVER
INTRODUCTION
This chapter emphasizes open surgical approaches to cystic disease of the liver.
DIAGNOSIS
Ultrasound
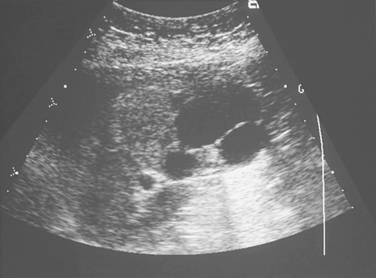
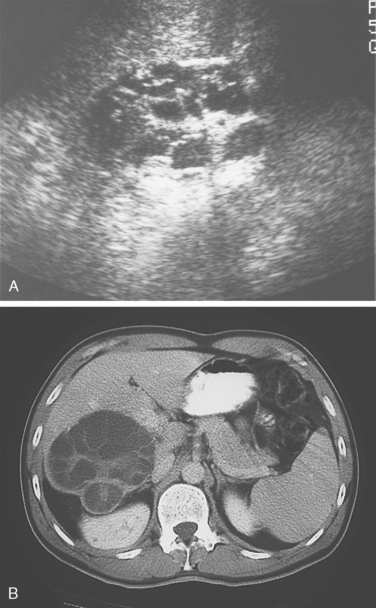
Simple cysts are characterized by acoustic enhancement posterior to the mass. They are solitary, thin-walled without focal thickening or nodularity, and anechoic without debris, and they lack septa. Septa typically are found in cystadenomas (Fig. 7-1); mural or septal nodularity most typically is seen in cystadenocarcinoma (Fig. 7-2). Hydatid cysts are typically hypoechoic and contain concentric peripheral daughter cysts within the larger cyst, and may have partial or complete calcification of the cyst wall (Fig. 7-3). Additionally, biliary ductal dilation or intraductal debris may be found within the biliary tree. Layering of blood within cysts may be seen after hemorrhage.
Computed Tomography
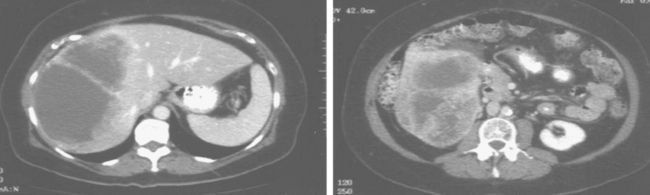
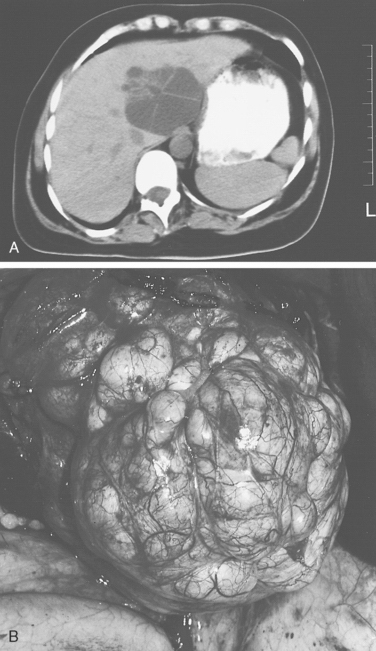
Computed tomographic (CT) features of hepatic cysts are similar to features seen on ultrasound (see Fig 7-3). Cyst hemorrhage and infection are confirmed by intracystic fluid layering or increased density. Vascular enhancement within the cyst wall or mural nodules suggest a cyst-associated malignancy or a cystadenocarcinoma (Fig. 7-4), whereas only septations occur with cystadenoma (Fig. 7-5). Polycystic liver disease (PLD) usually has some component of hepatic venous compression, but ascites usually indicates marked compression of all the major hepatic veins and the retrohepatic inferior vena cava. CT can define the extent of the compression of the major hepatic veins and inferior vena cava and help determine the extent of cyst resection or fenestration required to resolve hepatic venous outflow obstruction.
Endoscopic retrograde cholangiopancreatography (ERCP) documents the site and degree of biliary obstruction or often the site of biliary communication in jaundiced patients. Finally, cholangiography is essential to differentiate bile duct cysts from hepatic cysts with biliary communication. Magnetic resonance cholangiopancreatography (MRCP) also can be used for definition of the biliary system.
SIMPLE CYSTS
TREATMENT
Management by Laparotomy
Wide excision is essential, preferably excising greater than half the cyst to prevent sealing of the cyst remnant by adjacent viscera or diaphragm or residual cyst wall contraction with cyst recurrence. If less than half of the cyst is excisable, omentoplasty and ablation of the residual cyst epithelium by coagulation or sclerosant should be performed. Alternatively, hepatic resection prevents recurrence totally.
CYSTADENOMA AND CYSTADENOCARCINOMA
Cystadenomas are more common in women, and clinical presentation is similar to that of large simple cysts. Prominent intraductal septa and focal wall thickening with or without mural nodularity are the hallmarks of cystadenomas on imaging studies (see Figs. 7-1 and 7-5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree