Fig. 14.1
e-TEP trocar placement
The next step is to introduce the trocar PDB balloon, sliding on the posterior fascia to reach Cooper’s ligament. We begin inflating the balloon, and with zigzag movements, the preperitoneal Retzius and lateral Bogros spaces are opened, identifying the inferior epigastric vessels. PDB trocar is exchanged for a BTT trocar, and the 10 mm 30° optic is introduced.
Under direct vision, two 5 mm trocars are placed—one in the left paraumbilical region and one in the right iliac fosa—when a left inguinal hernia is corrected.
The steps that follow are no different from those taken in conventional TEP: enlargement/opening of the Bogros and Retzius spaces, reduction of the hernia sac, and mesh placement. However, if necessary, there is further opening of the preperitoneal space, and the semilunar ligament is sectioned, thereby extending the preperitoneal space that facilitates the successful completion of the surgical steps, particularly with large inguinoscrotal hernias. See Fig. 14.2.
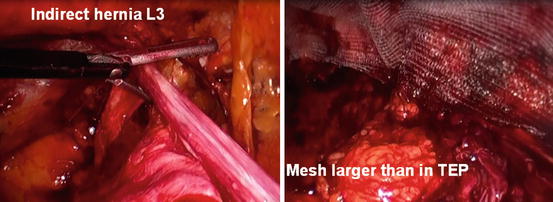
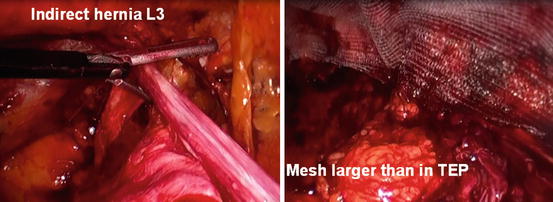
Fig. 14.2
e-TEP in right inguinal large hernia
Complications
The complications do not differ from TEP laparoscopic hernioplasty, previously explained in another chapter in this text.
Closure of the Defect in Ventral Hernia Laparoscopic Repair
Laparoscopic ventral hernia repair has been reported to have lower recurrence rates, fewer surgical site infections, and shorter hospital stays compared to open repair. The seroma formation, eventration (or bulging of mesh or tissue), and hernia recurrence remain common complications. In order to avoid or minimize these problems, primary closure of the defect by laparoscopy has gained popularity because this intervention restores the muscle continuity. It decreases the dead space, but if the defect is large, the closure could result in excessive pain and reduce the respiratory capacity [2, 3].
Indications are defects in the midline no more than 6–10 cm in diameter and no multisacular hernias with sacs not in the midline.
With this technique, the mesh necessary to cover the defect decreases. The dynamics of the abdominal wall muscle are restored more optimally and more quickly.
The incidences of seroma, mesh, tissue eventration, and hernia recurrence are significantly lower. Subjective improvement in overall patient satisfaction, cosmetic satisfaction, and functional status was reported with closing the central defect.
This technique could be superior for treating ventral hernias due to lower complication rates and higher patient satisfaction and functional status [4].
Surgical Technique [2, 3]
Transfascial sutures: from the outside, defect closure is done with transmural sutures.
Laparoscopy suture:
Closure of the defect with a continuous suture with needle. See Fig. 14.3.
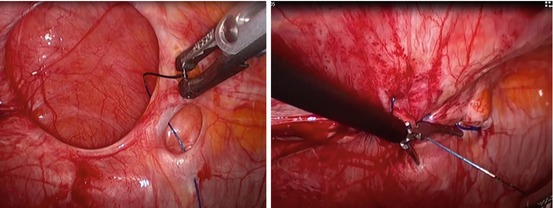
Fig. 14.3
Closure with V-Loc™ (Covidien, Dublin, Ireland) suture. 1 Incisional hernia exposed. 2 Closure of the defect with a continuous knotless (barbed) surgical suture. 3 Closure with V-Loc™ (Covidien, Dublin, Ireland) suture. 4 After the closure, the next step is the laparoscopic hernioplasty
Closure of the defect with the Endo-Stitch™ system (Covidien, Dublin, Ireland). See Fig. 14.4.
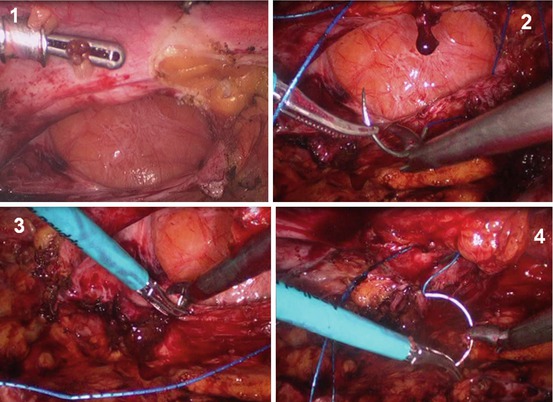
Fig. 14.4
Closure of the hernia defect with Endo-Stitch™ system (Covidien, Dublin, Ireland) with V-Loc™ (Covidien, Dublin, Ireland) suture
We use the new self-gripping sutures on both sides of the laparoscopic suture of the defect. They provide better tension and do not require an extra trocar to provide constant tension on the suture (V-Loc™, Covidien, Dublin, Ireland).
After the closure of the defect, a new measure of the hernia must be taken. The mesh is lower than if the defect had not been closed. This technique reduces the numbers of tackers significantly.
Laparoscopic Transabdominal Preperitoneal Repair of Ventral Hernia
The laparoscopic ventral hernia repair with preperitoneal placement of mesh minimizes the complications related to the intraperitoneal position of mesh and fixating devices. It allows safe use of conventional and less expensive polypropylene mesh.
Laparoscopically, ventral hernia repair is done by placing the mesh in either the preperitoneal (retromuscular) space or in the intraperitoneal onlay position. The placement of a large mesh in the preperitoneal space allows an even distribution of forces along the surface area of the mesh, which may account for the strength of repair and the decreased recurrence rates associated with it.
In intraperitoneal mesh placement, the direct contact of mesh with the abdominal contents cannot be avoided. The mesh behaves as a foreign material in relation to the abdominal contents and incites inflammatory reaction and adhesion formation [5, 6].
Following proper interface measures may not be possible. Severity of mesh-related complications depends on the position of the mesh in relation to the abdominal wall.
Diaz-Pizarro Graf and Chowbey demonstrated that preperitoneal placement of a polypropylene mesh is technically feasible and appears to have an advantage over laparoscopic intraperitoneal mesh placement for incisional hernia in selected patients [5, 6].
The fixation of the mesh can be done using tackers, fibrin glue, and new self-gripping meshes or with no fixation if the mesh is placed properly in the preperitoneal space. See Fig. 14.5.
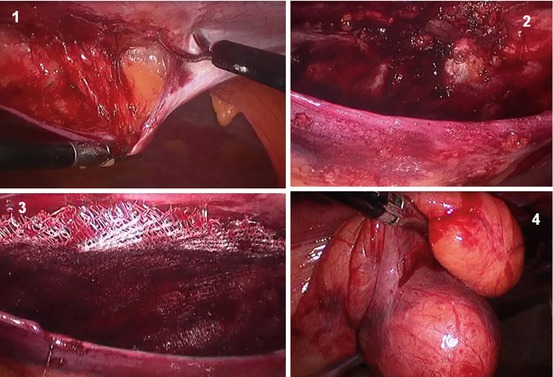
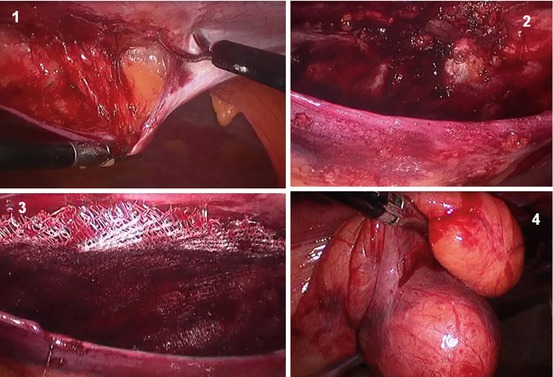
Fig. 14.5
Laparoscopic transabdominal preperitoneal repair of ventral hernia. 1 The peritoneum is opened it away from the ventral hernia. 2 The preperitoneal space is exposed and the hernia content is reduced. 3 Mesh extension along the preperitoneal space. This is a self-gripping mesh. 4 The hernia is reduced into the abdominal cavity and the peritoneum is closed
The technique is feasible and safe when performed by experts. The preperitoneal placement of the mesh not only avoids the direct contact of the prosthesis with viscera but also provides additional security of fixation and can minimize complications. It allows safe use of conventional and less expensive meshes such as polypropylene mesh, which has high intrinsic tensile strength and good memory [7].
Laparoscopic Repair of the Diastasis Recti
Endoscopic Approach in Diastasis Recti and Associated Umbilical Hernia
Currently, there are no published studies on minimally invasive surgical treatment of diastasis recti with an umbilical hernia associated [8].
The problem arises in those patients with a symptomatic umbilical hernia and diastasis recti above or below the navel. If only the hernia is surgically corrected, the defect will be closed on weak anatomical tissue which is damaged. As a result, the probability of hernia recurrence is increased with poor aesthetic outcome. Therefore, in the case of the coexistence of diastasis recti with a symptomatic umbilical hernia, it is advisable to do simultaneous correction of both pathologies.
For this, conventional surgery involves making an incision along the entire length of the fracture gap (supra-infraumbilical incision), with the probability of wound infection increased and with aesthetic deterioration involved. After this, the surgeon corrects the diastasis by plication, with or without reinforcement mesh, depending on the technique used. The umbilical hernia is corrected using mesh according to the principles of “no tension.”
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








