Primary urethral cancer is one of the rare urologic tumors. Distal urethral tumors are usually less advanced at diagnosis compared with proximal tumors and have a good prognosis if treated appropriately. Low-stage distal tumors can be managed successfully with a surgical approach in men or radiation therapy in women. There are no clear-cut indications for the choice of the most appropriate treatment modality. Organ-preserving modalities have shown effective and should be used whenever they do not compromise the oncological safety to decrease the physical and psychological trauma of dismemberment or loss of sexual/urinary function.
Key points
- •
Stage and anatomic location of the primary urethral tumor guide the choice of treatment modality and are the main determinants of prognosis and survival.
- •
Surgical options range from local excision to transurethral resection to partial urethrectomy/penectomy to total penectomy in men or excision of the urethra, vulva, and vaginal wall in women.
- •
For distal urethral tumors, surgical options are more appropriate for men whereas radiation therapy is a reasonable option in women.
- •
Routine inguinal or ilioinguinal lymphadenectomy for higher-stage tumors should be considered; however, there are few data derived from the treatment of primary urethral cancer to support it.
- •
Multimodal therapy is usually reserved for more advanced stages in combination with surgery to improve survival.
Introduction
Epidemiology
Primary urethral carcinomas (PUCs) are rare and account for less than 1% of genitourinary cancers. Most of the data rely on studies with small numbers of patients or case reports. PUCs arise from the urethral epithelium or from periurethral glands. The incidence of PUCs is known to be 3 to 4 times more common in women than in men. Recent data from the Surveillance, Epidemiology, and End Results (SEER) database, however, reported higher incidence in men, with an annual age-adjusted incidence rate of PUCs of 4.3 per million in men and 1.5 per million in women.
Etiology
Chronic inflammation, strictures, and sexually transmitted diseases are implicated in PUC. Columnar and mucinous adenocarcinoma may arise from glandular metaplasia and cribriform adenocarcinoma has its origins from the prostate. Squamous cell carcinoma (SCC) is associated with human papillomavirus (HPV) infection in both genders. HPV 16 or HPV 18 is associated in 60% of urethral carcinoma in women and HPV 16 is associated with 30% of pendulous urethra SCC in men. More than half the patients diagnosed with PUC have a history of stricture, and 25% have a history of sexually transmitted disease.
Anatomic Histopathology
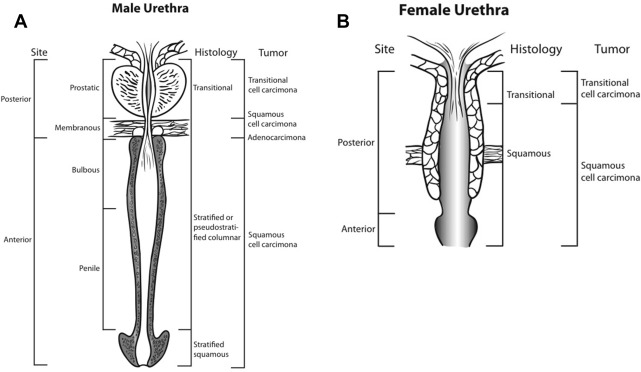
In men, the anterior urethra includes the penile and the bulbous urethra. The posterior urethra includes the prostatic and the membranous urethra. In women, the anterior urethra constitutes the distal one-third whereas the proximal two-thirds constitute the posterior urethra. The distal urethra in men is the penile and glandular urethra whereas in women the distal urethra constitutes the distal one-third of the urethra.
In women, lymphatics from the posterior urethra drain to the external and internal iliac and obturator lymph node chains. The anterior urethra drains to the superficial and then to the deep inguinal lymph nodes. In men, the lymphatics from the anterior urethra drain into the superficial and deep inguinal lymph nodes (and occasionally into the external iliac lymph nodes). The posterior urethra drains directly into one or any combination of the presacral, obturator, and external iliac lymphatic channels.
Different histologic types for PUC follow an anatomic distribution due to the presence of different epithelial histology depending on location ( Fig. 1 ). SCC is believed the most common type, representing more than 60% of PUCs in men and women. According to contemporary data extracted from the SEER, however, the distribution may be different. Among women, urothelial carcinoma (UC), SCC, and adenocarcinoma each represented approximately 30% of PUCs. In men, UC represented 78%, SCC 12% and adenocarcinoma 5% of cases.
Introduction
Epidemiology
Primary urethral carcinomas (PUCs) are rare and account for less than 1% of genitourinary cancers. Most of the data rely on studies with small numbers of patients or case reports. PUCs arise from the urethral epithelium or from periurethral glands. The incidence of PUCs is known to be 3 to 4 times more common in women than in men. Recent data from the Surveillance, Epidemiology, and End Results (SEER) database, however, reported higher incidence in men, with an annual age-adjusted incidence rate of PUCs of 4.3 per million in men and 1.5 per million in women.
Etiology
Chronic inflammation, strictures, and sexually transmitted diseases are implicated in PUC. Columnar and mucinous adenocarcinoma may arise from glandular metaplasia and cribriform adenocarcinoma has its origins from the prostate. Squamous cell carcinoma (SCC) is associated with human papillomavirus (HPV) infection in both genders. HPV 16 or HPV 18 is associated in 60% of urethral carcinoma in women and HPV 16 is associated with 30% of pendulous urethra SCC in men. More than half the patients diagnosed with PUC have a history of stricture, and 25% have a history of sexually transmitted disease.
Anatomic Histopathology
In men, the anterior urethra includes the penile and the bulbous urethra. The posterior urethra includes the prostatic and the membranous urethra. In women, the anterior urethra constitutes the distal one-third whereas the proximal two-thirds constitute the posterior urethra. The distal urethra in men is the penile and glandular urethra whereas in women the distal urethra constitutes the distal one-third of the urethra.
In women, lymphatics from the posterior urethra drain to the external and internal iliac and obturator lymph node chains. The anterior urethra drains to the superficial and then to the deep inguinal lymph nodes. In men, the lymphatics from the anterior urethra drain into the superficial and deep inguinal lymph nodes (and occasionally into the external iliac lymph nodes). The posterior urethra drains directly into one or any combination of the presacral, obturator, and external iliac lymphatic channels.
Different histologic types for PUC follow an anatomic distribution due to the presence of different epithelial histology depending on location ( Fig. 1 ). SCC is believed the most common type, representing more than 60% of PUCs in men and women. According to contemporary data extracted from the SEER, however, the distribution may be different. Among women, urothelial carcinoma (UC), SCC, and adenocarcinoma each represented approximately 30% of PUCs. In men, UC represented 78%, SCC 12% and adenocarcinoma 5% of cases.
Patient evaluation overview
Clinical Presentation
PUCs can present with hematuria or bloody urethral discharge. These are the presenting symptoms in up to 62% of the cases. Symptoms of locally advanced disease include a palpable urethral mass in 52%, bladder outlet obstruction in 48%, pelvic pain in 33%, urethrocutaneous fistula in 10%, and abscess formation in 5%. When they become clinically evident, urethral cancers are already locally advanced in 45% to 57%
Clinical Evaluation
For local staging, clinical examination should include palpation of the external genitalia and digital rectal examination in men to assess for mass/induration. In women, palpation of the urethra should be done. Speculum visualization to inspect the vaginal wall and vulva is also advised, in addition to bimanual examination. Palpation of the inguinal lymph nodes should be routinely performed. In contrast to penile cancer, the presence of palpable lymph nodes in urethral cancer is almost always metastasis.
Urine Cytology
The sensitivity of urine cytology in detecting PUC varies according to gender and histologic type. In a study by Toujier and Dalbagni, the sensitivity of urine cytology for UC in men was 80% compared with 50% in women. For SCC, however, the sensitivity in men was 50% compared with 77% in women.
Urethrocystoscopy
Urethroscopy and biopsy visualize the urethral tumor appearance, location, and extent and determine the histologic type. A concomitant cystoscopy should be performed to rule out the presence of a concomitant primary bladder tumor.
Imaging
Radiologic imaging is used to assess local tumor spread and metastasis to lymph nodes and distal organs. MRI is an excellent modality for local tumor staging of PUC ( Tables 1 and 2 ). MRI can assess involvement of the corpora cavernosa, status of pelvic and inguinal lymph nodes, and response to chemotherapy. The accuracy of MRI for staging urethral cancer has been reported to be approximately 75% and is superior to CT in visualizing tissue planes.
| Primary urethral (male and female) | |
| TX | Primary tumor cannot be assessed |
| T0 | No evidence of primary tumor |
| Ta | Noninvasive papillary, polypoid, or verrucous carcinoma |
| Tis | CIS |
| Tis pu | CIS, involvement of prostatic urethra |
| Tis pd | CIS, involvement of prostatic ducts |
| T1 | Tumor invades subepithelial connective tissue |
| T2 | Tumor invades any of the following: corpus spongiosum, prostatic stroma, periurethral muscle |
| T3 | Tumor invades any of the following: corpus cavernosum, beyond prostatic capsule, anterior vagina, bladder neck (extraprostatic extension) |
| T4 | Tumor invades other adjacent organs |
| Regional lymph nodes | |
| NX | Regional lymph nodes cannot be assessed |
| N0 | No regional lymph node metastasis |
| N1 | Metastasis in a single lymph node 2 cm or less in greatest dimension |
| N2 | Metastasis in a single lymph node more than 2 cm in greatest dimension or multiple lymph nodes |
| Distant metastasis | |
| MX | Distant metastasis cannot be assessed |
| M0 | No distant metastasis |
| M1 | Distant metastasis |
| Histopathologic grading (urothelial) | |
| PUNLUMP | Papillary urothelial neoplasm of low malignant potential |
| Low-grade | Well differentiated |
| High-grade | Poorly differentiated |
| Histopathologic grading (nonurothelial) | |
| GX | Grade of differentiation cannot be assessed |
| G1 | Well differentiated |
| G2 | Moderately differentiated |
| G3-4 | Poorly differentiated/undifferentiated |
| Stage Grouping | |||
|---|---|---|---|
| Stage 0a | Ta | N0 | M0 |
| Stage 0is | Tis | N0 | M0 |
| Tis pu | N0 | M0 | |
| Tis pd | N0 | Mo | |
| Stage I | T1 | N0 | M0 |
| Stage II | T2 | N0 | M0 |
| Stage III | T1/T2 | N1 | M0 |
| T3 | N0/N1 | M0 | |
| Stage IV | T4 | N0/N1 | M0 |
| Any T | N2 | M0 | |
| Any T | Any N | M1 | |
CT scan of the abdomen, in addition to chest radiograph (or CT chest) should be performed in all patients with invasive disease to detect distant metastases. PET CT is a promising modality for the detection of lymph node involvement and distant metastasis for PUC. PET CT is particularly useful for looking at suspicious sites of metastasis detected on alternate imaging (ie, CT/MRI).
Pharmacologic treatment options
One report discusses successful treatment with topical fluorouracil (5-FU) cream of carcinoma in situ (CIS) located close to or at the meatal opening in 2 patients. After treatment, 1 patient had no evidence of disease at 13 months and the other was also disease-free at 26 months.
Surgical treatment options in men
The standard treatment of distal PUC is total or partial penectomy. The surgical approach in PUC is derived from surgery for penile carcinoma. The size, stage, and anatomic location of a distal PUC dictate the choice of the surgical approach. A partial penectomy is chosen when residual penile length is sufficient with negative surgical margins. In urethral cancer, the traditional excision margin of 2 cm has been extrapolated from the general traditional management of penile carcinoma. Recent reports in penile cancer suggest that margins can be limited to 1 cm without compromising oncologic control. Furthermore, a large series on primary distal urethral cancer in men has achieved excellent local disease control even with margins less than 5 mm. Other more conservative penile-preserving approaches, such as transurethral resection, partial urethrectomy, and radiation, have been reported with satisfactory results in select cases.
Dinney and colleagues reported on 15 men with tumors in the penile urethra (n = 11) or fossa navicularis (n = 4) treated primarily with surgery. Tumors of the fossa navicularis of all stages were treated with either partial urethrectomy or partial penectomy with disease-specific survival (DSS) rates of 100% after a mean follow-up of 93 months. Penile urethral cancers had a DSS of 60% after a mean follow-up of 48 (5–156) months. Treatment consisted of surgical monotherapy in 5, a combination of surgery and chemotherapy in 4, and chemotherapy alone in 2. Surgical monotherapy consisted of 3 partial penectomies, 1 total penectomy with cystoprostatectomy, and 1 partial penectomy with pelvic node dissection. Two patients required adjuvant chemotherapy after surgery due to the presence of positive sentinel node biopsy.
Penile-preserving surgery, such as transurethral fulguration, local excision, or partial urethrectomy, is an attractive alternative to the traditional penectomy approach for early-stage distal tumors. The efficacy of these penile-preserving approaches in achieving long-term disease-free survival has been demonstrated by several studies ( Table 3 ). A series from the United Kingdom reported on penile-preserving surgeries for 18 men with distal PUC. Within a mean follow-up of 26 (9–58) months, 78% of the patients were alive and free of disease. One patient with a T1 tumor and 2 patients with CIS of the meatus were treated with biopsy and formation of hypospadias followed by topical 5-FU cream. Four patients underwent a 2-stage urethroplasty with buccal mucosa flap and 3 were treated with glansectomy with hypospadias and partial-thickness skin graft reconstruction. Six patients were treated with partial penectomy and reconstruction and 2 patients with large tumors of the penile urethra underwent anterior urethrectomy and perineal urethrostomy.





