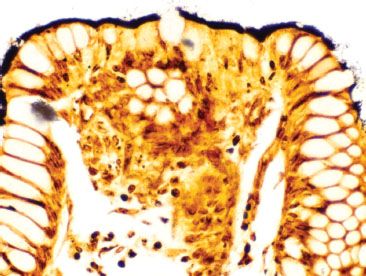
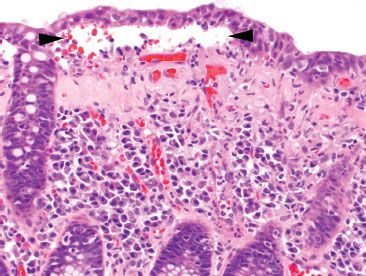
e-Figure 4.1
This colonic biopsy was taken from a 15-year-old female with abdominal pain and diarrhea. What stain would you perform to further evaluate this biopsy?
A. Acetylcholinesterase for the evaluation of Hirschsprung disease.
B. Congo red for the evaluation of amyloidosis.
C. Periodic acid–Schiff (PAS) for the evaluation of Whipple disease.
D. Silver impregnation stain, such as Warthin–Starry, for the evaluation of intestinal spirochetosis.
E. Tryptase or CD117 immunostain for the evaluation of mast cells.
Answer: Silver impregnation stain, such as Warthin–Starry, for the evaluation of intestinal spirochetosis (D).
This high magnification image shows a prominent “fuzzy” border along the surface epithelial cells, indicating the presence of intestinal spirochetosis. These organisms stain with silver impregnation stains (D). Acetylcholinesterase is a stain performed on fresh frozen tissue for the evaluation of Hirschsprung disease, which is typically diagnosed during infancy (A). It is true that Congo red (B), PAS (C), and tryptase/CD117 (D) may be helpful in other easily missed diagnoses such as amyloidosis, Whipple disease, and mastocytosis, respectively. However, there is no evidence of amyloid deposition, abundant foamy histiocytes, or mast cells in this high magnification image.
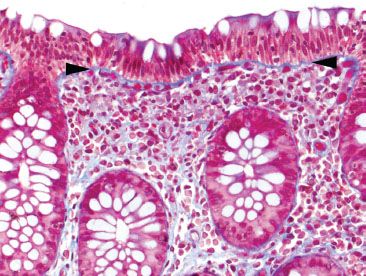
E-QUIZ QUESTION 2 (e-FIG. 4.2)
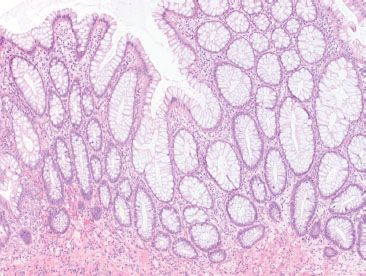
e-Figure 4.2
Following your observations from Question 1, you order a Warthin–Starry stain (shown), which confirms the presence of intestinal spirochetosis. Your clinician asks you whether there is concern for sexual abuse in this 15-year-old female. You answer:
A. Intestinal spirochetosis is sexually transmitted, but not reportable.
B. Intestinal spirochetosis is sexually transmitted, and the finding in a pediatric patient warrants further investigation into sexual abuse.
C. Intestinal spirochetosis is sexually transmitted, but only colonizes immunocompromised patients and the patient should be evaluated for both sexual abuse and HIV/AIDs.
D. Intestinal spirochetosis is transmitted by fecal-oral route, and the finding in pediatric patients is not uncommon; the finding does not implicate sexual abuse.
Answer: Intestinal spirochetosis is transmitted by fecal–oral route, and the finding in pediatric patients is not uncommon; the finding does not implicate sexual abuse (D).
Otherwise healthy children may have incidental colonization with these organisms, and the finding does not imply sexual abuse (D). Sexual transmission was initially proposed as a method of transmission due to the higher prevalence in homosexual men, but this remains unproven (A, B, C). Fecal oral transmission via contaminated water sources and colonized feces is far more likely.
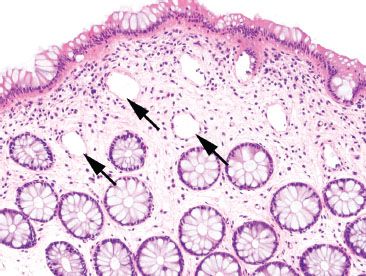
E-QUIZ QUESTION 3 (e-FIG. 4.3)
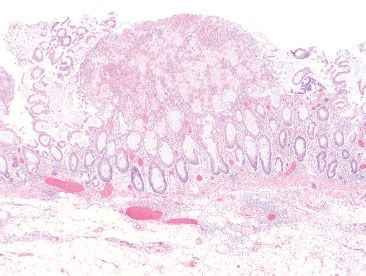
e-Figure 4.3
This colon biopsy is showing what feature?
A. Crypt distortion
B. Crypt branching
C. An innominate groove
D. Mucosal prolapse
E. Paneth cell metaplasia
Answer: An innominate groove (C).
The image depicts a normal finding in the colonic mucosa called an innominate groove (C) which should not be mistaken for crypt distortion (A) or crypt branching (B), such as seen in inflammatory bowel disease. The smooth muscle streaming seen in mucosal prolapse (D) is absent, and the crypt bases lack pink Paneth cells (E).
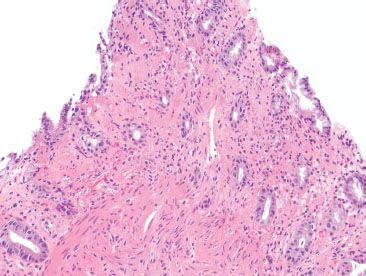
E-QUIZ QUESTION 4 (e-FIG. 4.4)
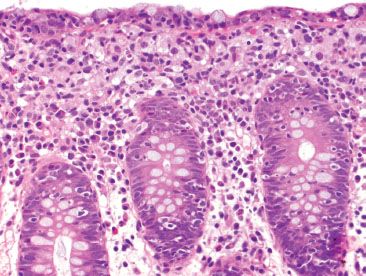
e-Figure 4.4
Which of the following statements is TRUE regarding the pseudomembranous colitis photomicrograph above?
A. If pseudomembranes are found diffusely throughout the colon, infection (such as C. difficile) is more likely than ischemia.
B. If pseudomembranes are found diffusely throughout the colon, ischemia is the most likely cause.
C. Colectomy for pseudomembranous colitis is inappropriate treatment for an infectious colitis and will likely result in a malpractice lawsuit.
D. Histologic distinction between infection and ischemic causes of pseudomembrane formation is always accurate.
E. Pseudomembranes found limited to watershed areas (such as the splenic flexure) always indicate infection.
Answer: If pseudomembranes are found diffusely throughout the colon, infection (such as C. difficile) is more likely than ischemia (A).
Knowledge of the distribution of pseudomembranes can help differentiate ischemic colitis from infectious pseudomembranous colitis; for example, when pseudomembranes are diffusely distributed, the cause is much more likely infectious (A), compared to ischemia, which is often segmental and found in watershed areas (B and E). Histologic distinction is rarely possible (D), and stool testing (culture or toxin test) remains the gold standard. Patients with severe or refractory infectious pseudomembranous colitis may warrant colectomy (C).
E-QUIZ QUESTION 5 (e-FIG. 4.5)
e-Figure 4.5
Careful examination of this colon biopsy reveals significant surface and crypt intraepithelial lymphocytosis. Which of the following statements is true?
A. Lymphocytic colitis qualifies as a “chronic colitis” because of the significant amount of chronic inflammation.
B. Lymphocytic colitis should never have neutrophils or cryptitis.
C. Lymphocytic colitis is always caused by an infectious etiology.
D. The distinction between lymphocytic and collagenous colitis is critical, as the treatment protocols differ widely.
E. Lymphocytic colitis is the presence of increased intraepithelial lymphocytes in the absence of histologic features of chronic injury (chronicity).
Answer: Lymphocytic colitis is the presence of increased intraepithelial lymphocytes in the absence of chronicity (E).
Lymphocytic colitis is the presence of increased intraepithelial lymphocytes (IELs) in the absence of chronicity (E). The IELs are not considered a feature of chronicity, and lymphocytic colitis is not a chronic colitis (A). Neutrophils may be seen in lymphocytic colitis, though sparsely (B). Medication reaction has been implicated in lymphocytic colitis, though the etiology is not always known (C). Lymphocytic and collagenous colitis share some overlapping features, and distinction between the two may not always be possible. Fortunately, the treatment protocols for both are similar (D).
E-QUIZ QUESTION 6 (e-FIG. 4.6)
e-Figure 4.6
The above colonic biopsy depicts:
A. Collagenous colitis
B. Bullous disease of the colon
C. Pseudomembrane formation
D. Acute ulceration
E. Viral infection
Answer: Collagenous colitis (A).
The colonic biopsy shows a thickened subepithelial collagen table with marked irregularity of its contour and entrapped small vessels. There is also a subepithelial cleft with the surface epithelium splitting away from the abnormal collagen table. The findings are those of collagenous colitis (A). Bullous diseases of the colon have not been described (B). Pseudomembranes are composed of fibrin and inflammatory debris, not pictured here (C). Although acute inflammation can be seen here, there is no evidence of ulcer formation (D), which should extend to the submucosa, by definition. No viral cytopathic effect is identified in this image (E).
E-QUIZ QUESTION 7 (e-FIG. 4.7)
e-Figure 4.7
After reviewing the H&E stained slide, you are concerned for collagenous colitis and order a trichrome stain to help you evaluate the subepithelial collagen (pictured). You correctly conclude:
A. This is collagenous colitis because the collagen is markedly thickened.
B. This is collagenous colitis because the collagen is extending downward as though it were “dripping candle wax.”
C. This is collagenous colitis because the collagen table has entrapped small blood vessels and fibroblast nuclei.
D. This is collagenous colitis because the abnormal collagen table has caused the surface epithelium to shear off.
E. This is not collagenous colitis; this is a normal collagen table.
Answer: This is not collagenous colitis; this is a normal collagen table (E).
Depicted is a normal subepithelial collagen table (E) that appears thin (A), smooth (B), without entrapped structures (C), and with an intact overlying epithelium (D).
E-QUIZ QUESTION 8 (e-FIG. 4.8)
e-Figure 4.8
This colon biopsy depicts:
A. Microcrypts of ischemic colitis
B. Amyloid deposition
C. Hyalinized lamina propria of ischemic colitis
D. Biopsy artifact with loss of crypt epithelium
E. Evidence of parasitic infection
Answer: Biopsy artifact with loss of crypt epithelium (D).
The biopsy depicts loss of colonic crypt epithelium (arrows) in an otherwise normal biopsy, most likely an artifact due to biopsy forceps (D). This can mimic the microcrypts of ischemic colitis (A), but note the lack of other ischemic features, such as loss of cytoplasmic mucin, withering crypts, and lamina propria hyalinization (C). The structures left behind may look like small vessels, but there is no evidence of amyloid deposition (B), and no inflammatory response or other evidence of parasitic infection is present (E).
E-QUIZ QUESTION 9 (e-FIG. 4.9)
e-Figure 4.9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








