Clots
VASCULAR ANATOMY OF LIVER
Liver constitutes 5% of body weight and receives 20% of cardiac output via hepatic artery (Ha) and portal vein (Pv)
Hepatic artery is a branch of hepaticoduodenal artery from celiac axis and carries 30% of total flow, but >50% of needed oxygen; Under high pressure, highly variable, dependant upon systemic blood pressure, regulated by adenosine concentration
Portal vein is valveless (formed from splenic & SMV), carries 70-80% of total liver blood flow and delivers <50% of needed oxygen; Under low pressure, not affected by systemic circulation, not regulated
Both Ha and Pv defined into Right & Left branches and eventually become arterioles and venules that drain into the sinusoids
At this level, hepatic arteries and sinusoids have sphincters that dynamically regulate blood flow i.e. a reduction of Pv flow leads to an immediate increase in Ha flow (total sinusoidal blood flow maintained constant; However, Pv flow is relatively constant and is not influenced by Ha flow)
At the end of sinusoid, blood enters the central venule forming the hepatic venule; Three major hepatic veins(Hv): Right/Middle/Left
The veins have different blood distributions from Ha and Pv, influencing surgical intervention
The liver is divided into eight segments, each having own afferent and efferent blood supply
Microarchitecture: See also Liver- Histopathology of Liver (Chapter 4.19)
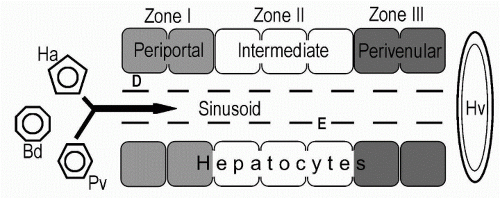
Basic element of liver structure is liver cell plate, consisting of 15-20 hepatocytes lined up between the portal area and hepatic veins
Perivenular (Zone III) hepatocytes are subject to more hypoxia because they are at end of unidirectional sinusoidal blood flow
Zone II and III are involved in drug metabolism and are rich in cytochrome P450 enzymes
Pv (portal vein)
Ha (hepatic artery)
Hv (hepatic venules)
E (fenestrated epithelium) (contain Kupffer cells)
Blood from Pv and Ha, join and traverse sinusoids, leaving the liver from Hv; Low pressure circulation in sinusoids allows plasma to pass through E, and reach D, where via direct contact with hepatocytes, exchange of nutrients and metabolites takes place
D (space of Disse) (contain Stellate cells)
Bd (bile duct)
Note: Stellate cells when activated take on characteristics of fibroblasts and cause fibrosis or cirrhosis; Kupffer cells are phagocytic cells
Note: a sick liver can produce a misbalance of clotting/anticlotting factors, hence a cirrhotic can form clots if more clotting factors produced
BUDD-CHIARI SYNDROME (BCS)
Definition:
Thrombosis/occlusion of the hepatic veins (small venules, large hepatic veins), IVC or even the right atrium
Etiologies:
Hypercoagulable: Myeloproliferative syndromes, Paroxysmal nocturnal hemoglobinuria, SLE, Protein C & S or antithrombin-III deficiency, Pregnancy/OCP
Tumor invasion: HCC, Renal, Adrenal, Pancreas
Inferior vena cava membranous web
Trauma
Postpartum
Idiopathic (Factor V Leiden may be responsible for 25% of BCS considered ‘idiopathic’)
Pathophysiology:
Increased sinusoidal pressure caused by obstructed hepatic venous outflow: hypoxic damage to hepatocytes and increased portal pressure
Continued obstruction leads to further hepatic necrosis and ultimately cirrhosis
Clinical Manifestations/Physical Exam:
Ascites (>90% of patients) is cardinal feature
RUQ pain (80% of patients)
Hepatosplenomegaly, Jaundice (slight when present), PSE and Variceal bleeding are less common and late findings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree