Fig. 1
Peroral video cholangioscopy. a white-light imaging, b narrow-band imaging
Cholangioscopic Findings in Benign and Malignant Lesions
Several investigators have identified characteristic cholangioscopic findings in various biliary-tract diseases (Table 1). The normal bile duct shows a flat surface, with or without shallow pseudodiverticulae, which represents the orifice of the bile duct gland and a fine network of normal thin vessels. In inflammatory diseases, e.g., chronic cholangitis and primary sclerosing cholangitis, irregular surface, scarring, and pseudodiverticulae with or without intradiverticulae are often seen [22]. Dilated tortuous vessels without encasement or fusion of vessels can be seen in immunoglobin G4 (IgG4)-related sclerosing cholangitis due to vascular congestion [22]. On the other hand, irregular papillary or granular lesions, and nodular elevated lesions are typical cholangioscopic findings that raise concern for biliary neoplasia. Friability of the lesions and easy bleeding are often seen with dilated or non-dilated tortuous vessels. In terms of typical neoplastic vessels, so-called “tumor vessels,” either angiogenic or tumorigenic, are partially dilated vessels with encasement and fusion of vessels. We previously reported that the features of vessels were divided into four types: (1) sporadic fine vessels which are frequently seen in normal mucosa, (2) aggregated fine vessels without dilation which are frequently seen in chronic inflammation (Type I), (3) dilated and tortuous vessels without encasement or fusion of vessels (Type II), (4) partially dilated vessels without encasement and fusion of vessels (Type III; Fig. 2, Vessel patterns). Type I vessels are usually benign and Type III are typically malignant lesions. However, in the case of Type II vessels, such a differentiation between benign and malignant lesions poses a diagnostic dilemma given the cholangioscopic similarities .
Fig. 2
Vascular patterns of bile duct mucosa
Table 1
Cholangioscopic findings in various biliary tract lesions
Lesions | Cholangioscopic findings |
|---|---|
Normal | Flat surface with or without shallow pseudodiverticulae |
Fine network of normal vessels | |
Inflammatory lesions | Bumpy surface, pseudodiverticulae with or without intradiverticula stones |
Regular granular lesions (hyperplasia) | |
Dilated or non-dilated tortuous vessels without encasement or fusion of vessels | |
Scaring | |
Neoplasms | Irregularly papillary or granular lesions |
Nodular elevated lesions | |
Friability and easily bleeding | |
Dilated to non-dilated tortuous vessels | |
Partially dilated vessels with or without encasement and fusion of vessels |
Therapeutic Cholangioscopy
In a mother–daughter system, therapeutic interventions are limited by the size of the available 1.2-mm working channel. Devices which fit in this narrow-working channel include the 1.9-Fr electrohydraulic lithotripsy probe (Fig. 3) and holumium yttrium aluminum garnet (YAG) laser lithotripsy. On the other hand, in PDCS using ultra-slim endoscopes, which accommodate 5-Fr devices, various therapeutic interventions (Fig. 4) such as therapeutic drug injection, tumor resection , stone extraction, migrated stent removal, argon plasma coagulation (APC), and photodynamic therapy (PDT), are feasible .
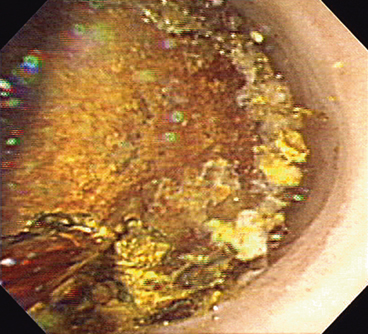

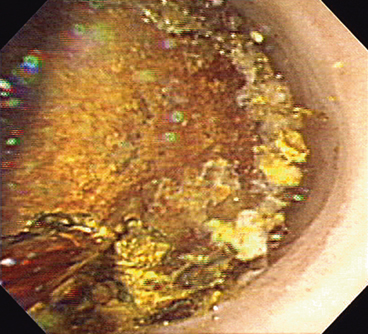
Fig. 3
Electric hydraulic lithotripsy for bile-duct stone (mother–daughter video cholangioscopy)

Fig. 4
5-Fr accessories for ultra-slim upper endoscopes
Cholagioscopic Procedure and Outcome
Cholangioscopy procedures are performed with the patient in the prone position with intravenous anesthesia (propofol, 0.5 mg/kg) or with conscious sedation (intravenous midazolam, 0.05 mg/kg).
To improve visualization during cholangioscopy, regardless of the type of POCS used, either sterile saline solution or carbon dioxide insufflation has been used. One comparative study revealed that carbon dioxide insufflation provides better imaging and reduces procedure time compared to sterile-saline solution in almost all cases except in biliary protruding lesions [23].
Through-the-Duodenoscope Cholangioscopy
Mother–Daughter Type Cholangioscopy
Procedure
The therapeutic duodenoscope, which is used as the mother scope has a 4.2-mm working channel, which helps to avoid kinking and damage to the cholangioscope. At present, several fiberoptic and video cholangioscopes (Fig. 5a, b) are commercially available in various countries. The specifications of the mother–daughter system video cholangioscopy are shown in Table 2. Two skilled endoscopists are required for effective control of the endoscopes and visualization.


Fig. 5
Mother–daughter video cholangioscopy system. a Actual procedure, b Tip of duodenal scope with daughter cholangioscope
Table 2
Specification of daughter (baby) videocholangioscopy
OLYMPUS | ||
|---|---|---|
CHF-BP260 | CHF-B260/B160 | |
Angle of view, degrees | 90 | 90 |
Observed depth, mm | 3–20 | 3–20 |
Outer diameter, mm | ||
Distal end | 2.6 | 3.4 |
Insertion end | 2.9 | 3.5 |
Bending section, degrees | ||
Up/down | 70/70 | 70/70 |
Right/left | NA | NA |
Working length, mm | 2000 | 2000 |
Working channel diameter, mm | 0.5 | 1.2 |
Image-enhanced endoscopy | NBI | NBI |
Endoscopic sphincterotomy is a usually a prerequisite for mother–daughter system POCS to facilitate scope passage across the papilla and allow an escape route for saline and carbon dioxide used for insufflation and irrigation. The daughter cholangioscope is advanced through the 4.2-mm working channel of therapeutic duodenoscope into the bile duct either free hand or over a 0.025- or 0.035-in. guide-wire. Utilizing the daughter cholangioscopes has 2-way deflections (up and down), and the mother duodenoscopes 4-way angulation, along with the elevator mechanism on the mother scope and the ability to vary from a long to short scope position; skilled endoscopists can obtain excellent controlled visualization of the entire biliary tree. An excessive use of the elevator mechanism of the mother duodenoscope can damage the daughter cholangioscope, in particular when the V-system duodenoscope (TJF-260V, Olympus medical systems, Tokyo, Japan; TJF-160V, Olympus America, Pennsylvania (PA)) is used. The video cholangioscope (CHF-B260/B160 and CHF-BP260, B260 and BP260, Olympus medical systems, Japan; B160, Olympus America) and the NBI system (CV-260SL, CVL-260SL/CV-180, CLV-180, light source, Olympus medical systems/Olympus America) should be used to highlight the vascular topography of intraductal lesions when needed.
After inspection with peroral video cholangioscopy (PVCS), the targeted biopsies from the lesions can be performed using a 3-Fr diameter ultrathin biopsy forceps (FB-44U-1, Olympus). However, with the slimmer PVCS (the CHF-BP260), a guide-wire or biopsy forceps cannot be used because of the small-working channel (0.5-mm in diameter).
Outcome
The outcomes of large case series including three retrospective studies [24–26] and 1 prospective study [27] are described in Table 3. A mother–daughter system POCS in combination with tissue sampling provided high accuracy (94–98 %), sensitivity (86–100 %), specificity (87–92 %), positive predictive value (88–99 %), and negative predictive value (96–100 %) for the diagnosis of indeterminate filling defects and biliary strictures, regardless of the use of fiberoptic or video POCS, retrospective or prospective analysis. In addition to determination of filling defects and biliary strictures, Kawakami et al. suggested that video POCS might be useful for the detection of mucosal spread of neoplasia and assists with the decision regarding extent of surgical resection in patients with cholangiocarcinoma [28].
Table 3
Summary of accuracy of mother-daughter type cohlangioscopy
Authors | n | Center | Study | Scope | Methods | Ac. (%) | Sen. (%) | Spe. (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|---|---|---|---|---|---|
Fukuda GIE 2007 | 97 | Single | R | Fiber | ERC/Tissue/POCS | 94 | 100 | 87 | 88 | 100 |
Shah CGH 2007 | 62 | Single | R | Fiber | W/wo Tissue/POCS | – | 86 | 96 | 89 | 96 |
Itoi CGH 2010 | 144 | Mum | R | Video | ERC/Tissue/POCS | 98 | 99 | 96 | 99 | 96 |
Nishikawa GIE 2013 | 33 | Single | P | Video | ERC/Tissue/POCS | 97 | 100 | 92 | 96 | 100 |
Single-Operator Fiberoptic Cholangioscopy
Procedure
A single-operator system for cholagioscopy introduced recently by Bostoc Scientific has revolutionized the field of cholangioscopy. This technology incorporates a fiberoptic cholangioscopy which is to be strapped to the duodenoscope just below the working channel with a silastic belt, a pump, a light source, and a monitor, and three disposable devices: (1) a reusable 0.77-mm diameter optical probe (SpyGlass), (2) a 10F disposable 4-lumen catheter (SpyScope) consisting of a 0.9-mm channel for the SpyGlass fiber-optical probe, a 1.2-mm instrumentation channel and two dedicated 0.6-mm irrigation channels, and (3) a disposable 3F biopsy forceps (SpyBite) [29–32] (Fig. 6a, b). The modular system consists of 3 components: (1) a reusable 0.77-mm diameter optical probe (SpyGlass) for direct visual examination of the targeted duct, (2) a 10F disposable 4-lumen catheter (SpyScope) consisting of a 0.9-mm channel for the SpyGlass fiber-optical probe, a 1.2-mm instrumentation channel and two dedicated 0.6-mm irrigation channels, and (3) a disposable 3F biopsy forceps (SpyBite) for tissue acquisition in the pancreaticobiliary system [29, 30]. Since the SpyScope catheter has 4-way tip deflection, it provides good catheter maneuverability in the duct for diagnostic visualization and interventions. In contrast, the conventional mother–daughter POCS is capable of only 2-way tip deflection. Improvement of maneuverability (4-way tip deflection) may enable free-hand cholangioscope insertion without a guide-wire. Once the tip of the cholangioscope is advanced into the bile duct, irrigation of sterile saline is usually required for better visualization.
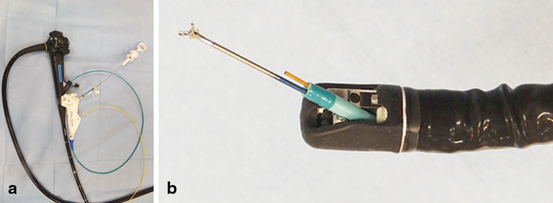
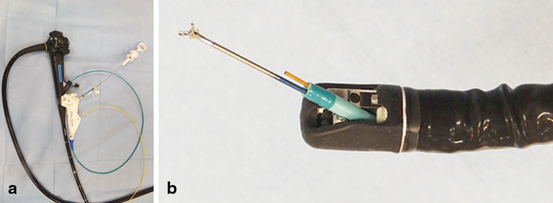
Fig. 6
Single-operator cholangioscopy system (SpyGlass). a Outside appearance. b Tip of duodenal scope with SpyScope and SpyBite
Outcome
Experimental benchmark and clinical feasibility studies have already been described by Chen [29] and Chen and Pleskow [30]. To date, there are three prospective studies including one multi-center study and two single-center studies on the evaluation of SpyGlass in biliary diseases [32–34]. One single center study showed that the diagnostic accuracy of SpyGlass cholangioscopic impression was 89 % although the diagnostic accuracy of SpyBite cholangioscopic biopsy was slightly lower at 82 % [32]. A multi-center study revealed that the SpyGlass cholangioscopic accuracy was 78 %. In contrast, the diagnostic accuracy of SpyBite cholangioscopic biopsy was only 49 %. These results suggest that visualization and targeted tissue acquisition are complementary during cholangioscopy. Others have reported greater success with targeted biopsy. For instance, Draganov reported that the diagnostic accuracy of POCS biopsy (85 %) was superior to both cytology brushing (39 %) and fluoroscopic standard forceps biopsy (54 %) [34].
Peroral Direct Cholangioscopy
Urakami et al. first reported on the PDCS with a standard upper endoscope using the direct-insertion technique in 1977 [6] . However, as noted above, PDCS has not been widely adopted due to technical difficulties associated with direct peroral intubation of the bile duct with a standard upper endoscope. As a result, presently, the use of the mother–daughter system POCS has become widespread. The introduction of the single-operator cholangioscope system, has spurred efforts at direct peroral cholangioscopy. Recently, Larghi and Waxman reported a feasibility study of PDCS using a conventional ultra-slim upper video endoscope [7] (Table 4). Since then, several studies on the diagnostic and therapeutic PDCS have been published [8–15].
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








