Cholangiocarcinoma
DEFINITION:
Bile duct cancers that arise from the epithelial cells of the bile ducts (does not include gallbladder or ampullary cancer)
Classification:
Intrahepatic: originate from small or large intrahepatic ducts proximal to right and left hepatic duct bifurcation
Perihilar Extrahepatic (65%): includes the confluence of the right and left hepatic duct bifurcation
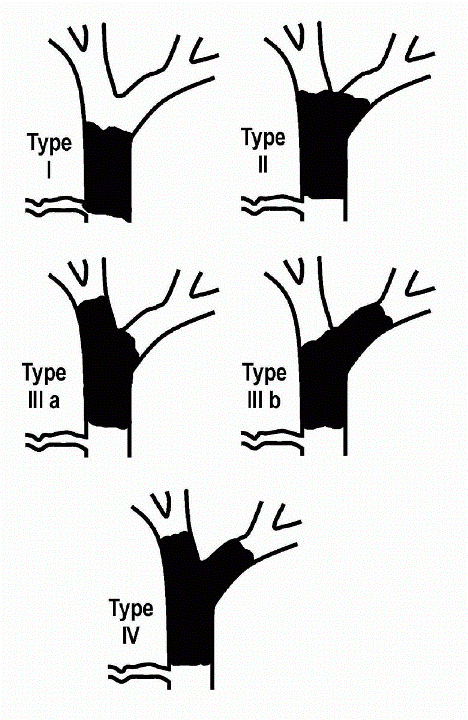
Further classified according to involvement of the hepatic ducts: Bismuth Classification (Figure)
Type I: tumors below the confluence
Type II: tumors reaching the confluence
Type IIIA & IIIB: tumors occluding the common hepatic and Right or Left hepatic duct
Type IV: tumors that are multicentric or involving confluence and both hepatic ducts
Klatskin tumors: term used to define involvement of the common hepatic duct bifurcation
Distal Extrahepatic: from common bile duct to the point where the bile duct lies posterior to the duodenum
|
EPIDEMIOLOGY:
Rare; Represent 3% of GI malignancies with an incidence of 1-2 per 100,000; ♂ > ♀
Nearly all (>90%) are adenocarcinomas, further divided into:
Sclerosing: invade bile duct early, associated with low respectability and cure rates
Nodular: constricting annular lesion of the bile duct and highly invasive
Papillary: rare, present as bulky masses in the common bile duct and early presenting symptoms
ETIOLOGIES:
Several risk factors identified:
PSC/UC patients represents 30% of all diagnosed cholangiocarcinoma (lifetime risk is 10-15% for PSC/UC patient)
Difficult to diagnose since biliary tree is abnormal to begin with; >30% diagnosed within 2 years of PSC diagnosis
Screening suggested by some clinicians: US and CA19-9 annually or semi-annually if cirrhotic
A CA19-9 >100 U/ml and a malignant appearing stricture has been used in lieu of tissue diagnosis to begin treatment
Choledochal cysts, Caroli’s syndrome, Congenital hepatic fibrosis: 15% risk of malignant change (average age at diagnosis is 34)
Unclear why; could possibly be related to biliary stasis or chronic inflammation via pancreatic juice reflux
Parasitic infection:
Infection with liver flukes (Clonorchis and Opisthorchis) is associated with intrahepatic bile duct cancer, especially in Asia
Consuming undercooked fish leads to adult worms laying eggs in the biliary system leading to chronic inflammation
Hepatolithiasis and Cholelithiasis:
Unclear if gallstones really predispose to cholangiocarcinoma
There is a clear association with intrahepatic stones (much higher prevalence in Asia) and cholangiocarcinoma
Toxic exposures:
Thorotrast, an old radiologic contrast agent banded in the 1960’s showed a clear association
Association of smoking and alcohol are conflicting as is occupational exposures (auto, rubber, wood)
Lynch syndrome II and Multiple biliary papillomatosis
Have an associated increased risk
Chronic liver disease:
Other possible risks:
Diabetes, HIV infection
PATHOPHYSIOLOGY:
Conversion from normal to malignant bile epithelium is probably a stepwise accumulation of genetic mishaps similar to colon cancer
Evidence of such genetic abnormalities is poorly understood
Evidence of oncogenes (K-ras) and tumor suppressor genes (p53) have been described
CLINICAL MANIFESTATIONS/PHYSICAL EXAM:
Usually symptomatic when there is obstruction of the biliary system causing painless jaundice and:
Pruritus-intermittent (66%), abdominal pain (30-50%), weight loss (30-50%), fever (10-20%), clay-colored stools and dark urine
Signs include jaundice (90%), hepatomegaly (25-40%), and rarely a RUQ mass (10%) or Courvoisier’s sign (palpable gallbladder)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree