Cardiology
Question 1
A 55-year-old woman smoker is seen in the emergency room (ER) complaining of several days of increasing facial fullness, orthopnea, and swelling in her neck and hands. Physical examination is notable for obvious facial swelling, with conjunctival edema, jugular venous distention, and symmetric swelling of both upper extremities. Fullness is present in both supraclavicular fossae, but there is no clear lymph node enlargement, and the lungs are clear. The patient is tachycardic, but no gallop, murmur, or rub is present. No hepatomegaly, ascites, or pedal edema is present. Chest radiography reveals a right hilar mass. The patient is admitted to the hospital at midnight, and you order which of the following?
a) An emergency upper extremity venogram
b) An emergency computed tomography (CT) scan of the chest
c) An emergency echocardiogram (ECHO)
d) Diuretics and elevation of the head of the bed until the morning
View Answer
Answer and Discussion
The answer is d.
Objective: Understand the urgent management of superior vena cava (SVC) syndrome.
The clinical diagnosis of SVC syndrome is clearly evidenced by symptoms of increased venous pressure and chest X-ray (CXR) showing potential etiology with a right hilar mass. Although the presentation is dramatic, it is not life-threatening, and the initial management is symptomatic, with loop diuretics and elevation of the head of the bed. Emergency diagnostic procedures are rarely indicated.
Question 2
You see the previous patient the next morning. She feels better, although she remains quite edematous and cannot lie flat. You order the following test to determine the etiology of the patient’s SVC syndrome:
a) CT scan of the chest
b) Thyroid scan
c) Serologic test for syphilis
d) Upper extremity venogram
e) All of the above
View Answer
Answer and Discussion
The answer is a.
Objective: Understand the appropriate diagnostic workup for SVC syndrome.
All of these tests are used to identify the etiology of SVC syndrome. Malignancy is the most common cause of SVC syndrome and is suggested by this patient’s chest radiograph. Therefore, a CT scan should be the next test to determine both the etiology and further anatomic definition of the process. A thyroid scan helps identify a thyroid mass causing extrinsic compression, but would not present as a right hilar mass. An upper extremity venogram is helpful for intravascular obstruction, but would not give further definition of a mass.
Question 3
You are called by the radiologist that afternoon with the results of the chest CT scan. This study reveals a large right hilar and a mediastinal mass, with evidence of compression of the SVC. Your response is which of the following?
a) Expeditiously proceed to bronchoscopy or mediastinoscopy to establish the tissue diagnosis
b) Recognize the risk of invasive diagnostic procedures in patients with SVC syndrome and order sputum cytology
c) Identify this as an incurable malignancy and refer the patient for urgent radiation therapy
d) Identify this as an incurable malignancy and refer the patient for hospice care
View Answer
Answer and Discussion
The answer is a.
Objective: Identify the most common etiology of SVC syndrome.
Invasive diagnostic procedures do not pose any increased risk in patients with SVC syndrome. Although the etiology is likely to be malignant, several of the potential malignant diagnoses are curable with appropriate treatment, and this treatment may include chemotherapy. Aggressive and expeditious attempts to establish a histologic diagnosis are indicated so that the most effective treatment can be initiated in an organized fashion.
Question 4
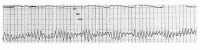
An 18-year-old, 58-kg female asthmatic patient is intubated in the emergency department for respiratory failure from status asthmaticus. You aggressively fluid resuscitate her. She is being treated with clarithromycin, ceftriaxone, Solu-Medrol, bronchodilators, and lorazepam and has been stable for 3 days. On day 3, she became agitated overnight and was given haloperidol. Suddenly, she became hypotensive, and her pulse was not palpable. The electrocardiogram (ECG) tracing is shown below.
|
The patient is still hypotensive, her white blood cell count is 15,000/mm3, and her hemoglobin is 10 g/dL. You will do all of the following, except
a) Perform cardioversion-defibrillation
b) Administer magnesium intravenously
c) Temporarily disconnect the patient from the ventilator circuit
d) Correct hypocalcemia, hypokalemia, and alkalosis
View Answer
Answer and Discussion
The answer is c.
Objective: Identify drug-drug interaction in the intensive care unit (ICU) setting.
This question highlights an important topic in critical care medicine-drug interactions. This scenario demonstrates the ability of drugs to lengthen the QT interval, thereby predisposing to torsades de pointes. Another important effect of drug interaction in the critically ill patient is hypotension caused by partial adrenal insufficiency. This drug interaction occurs in patients receiving drugs that can increase the activity of the P450 system (e.g., phenytoin, phenobarbital). When the P450 system is activated, the metabolism of steroids increases, creating a state of partial adrenal insufficiency. This drug interaction should be suspected in patients receiving medication that can increase the metabolism of the P450 system and in patients with persistent hypotension in the absence of other etiologies. An increasingly recognized offender is etomidate, a medication commonly used in rapid-sequence intubation, which blocks adrenal steroid production directly.
Macrolides and haloperidol, drugs commonly used in the ICU, are known to increase the QT interval. Patients with underlying ischemic heart disease and electrolyte and acid-base abnormalities are more likely to develop this complication. Phenothiazines, antiarrhythmic medications, tricyclic antidepressants, and antipsychotic agents and cisapride can prolong the QT interval as well.
Question 5
A 56-year-old woman with advanced arthritis of the right knee and a diagnosis of hypertension and hyperlipidemia has atypical chest pain with a normal ECG. The best diagnostic option is
a) Stress (exercise or dobutamine) ECG
b) Coronary angiography
c) Exercise echocardiography
d) Dipyridamole-thallium imaging
e) echocardiography (ECHO)
View Answer
Answer and Discussion
The answer is d.
Objective: Identify the optimal method of stress testing in the diagnosis of coronary artery disease (CAD).
This is a 56-year-old woman who is described as having advanced arthritis. Therefore, exercise stress will likely result in the patient being unable to exercise maximally or even at all. Because the patient is a female with atypical pain, she would be considered to have an intermediate pretest probability and therefore would be a good candidate for a stressimaging study. Proceeding directly to coronary angiography with such a relatively low pretest probability would potentially subject the patient to an unnecessary invasive test.
Question 6
A 28-year-old woman with hypertension and diabetes presents with left-sided chest pain at rest and exercise. The best diagnostic option is
a) Exercise ECG
b) Coronary angiography
c) Exercise echocardiography
d) Exercise thallium imaging
e) None of the above
View Answer
Answer and Discussion
The answer is e.
Objective: Identify the pretest probability of CAD and the subsequent level of evaluation required.
This patient has a very low pretest probability for having CAD (˜4%) due to her age, gender, and the atypical nature of the pain. Because of this low pretest probability, the accuracy of a given test will not significantly affect the post-test probability of disease. It is only in those patients with an intermediate pretest likelihood of disease that the accuracy of the test will have a significant effect on post-test probability. Therefore, none of the choices provides the best diagnostic option, as that likely includes consideration of another etiology for the pain other than cardiac.
Question 7
A 68-year-old man presents with central retrosternal chest pain on exercise. The best diagnostic option is
a) Exercise ECG
b) Coronary angiography
c) Exercise echocardiography
d) Exercise thallium imaging
e) None of the above
View Answer
Answer and Discussion
The answer is b.
Objective: Understand the identification of the pretest probability of CAD and the subsequent level of evaluation required.
This patient would have a high pretest probability of disease; therefore, coronary angiography would provide information on the site, the severity, and extent of the disease. Although an exercise electrocardiography study as well as an imaging study with echocardiography or thallium perfusion imaging would be useful in risk stratifying such a patient, the definitive test to detect disease in this patient with such a high pretest probability would be coronary angiography.
Question 8
A 48-year-old man with hypertensive left ventricular (LV) hypertrophy complains of atypical chest pain. The best diagnostic option is
a) Exercise ECG
b) Coronary angiography
c) Exercise echocardiography
d) Dipyridamole-thallium imaging
e) None of the above
View Answer
Answer and Discussion
The answer is c.
Objective: Identifying the optimal method of stress testing in the diagnosis of CAD.
An exercise ECG stress test is likely to be nondiagnostic in patients with LV hypertrophy. As a result of the resting secondary ST-T wave repolarization changes characteristic of LV hypertrophy, a false-positive result is likely and may therefore inappropriately lead to further testing. A coronary angiogram would lead to undue risk from an invasive procedure, particularly in a 48-year-old man with atypical pain. A dipyridamole-thallium study is also limited by the potential of falsely positive perfusion defects that likely are secondary to subendocardial ischemia from abnormal coronary flow reserve. Subendocardial ischemia can occur in hypertrophied hearts despite the presence of normal epicardial vessels. Exercise echocardiography has been demonstrated to be more specific in this patient population, as the basis for this test is an assessment of LV function rather than perfusion, which can be affected by abnormalities in coronary flow reserve.
Question 9
A 52-year-old man needs a femoropopliteal bypass. What would you recommend first for risk stratification?
a) Exercise ECG
b) Coronary angiography
c) Dobutamine echocardiography
d) Dipyridamole-thallium imaging
e) Clinical evaluation
View Answer
Answer and Discussion
The answer is e.
Objective: Identify the initial assessment for risk stratification and cardiac optimization prior to a vascular surgical procedure.
The initial risk stratification should include a clinical examination that initially is directed at determining the urgency of surgery, assessing risk, identifying the need for noninvasive testing in selected patients, and initiating measures to reduce operative risk in those at high risk. Those patients identified to have three or more revised cardiac index criteria (high-risk surgery, history of ischemic heart disease, history of cerebrovascular disease, insulin-dependent diabetes mellitus, or preoperative serum creatinine >2.0 mg/dL) and poor functional capacity (<4 METs) should undergo stress testing if it will change management.
Question 10
The following probably constitute significant CAD, except
a) Proximal left anterior descending (LAD) stenosis of 80%
b) LAD stenosis of 60% with angina
c) Right coronary artery stenosis of 50%
d) Left circumflex coronary artery stenosis of 50% with a positive exercise ECG
View Answer
Answer and Discussion
The answer is c.
Objective: Understand the definition of significant CAD.
Significant CAD is typically considered to be present with lesions >50% of the artery diameter. But coronary stenoses in the 50% range may or may not be functionally significant in terms of a reduction in coronary flow, as flow reduction is modulated by collateral vessels, location, and length of stenoses and related to bends and bifurcations as well as other variables. Coronary artery stenoses >90% have been demonstrated to restrict flow at rest without the provocation of stress. Therefore, in this question, a proximal LAD stenosis of 80% almost certainly is considered significant disease, and an LAD stenosis of 60% in the presence of typical angina pectoris also quite likely represents significant flow-limiting coronary disease. Finally, a left circumflex coronary stenosis of 50% with the presence of positive exercise ECG changes is likely to represent significant CAD, yet a right coronary stenosis of 50% in the absence of a functional test that is positive for ischemia or the presence of
concomitant symptoms may represent the presence of significant stenosis.
concomitant symptoms may represent the presence of significant stenosis.
Question 11
Which of the following patients has the greatest probability of CAD?
a) A 48-year-old woman with atypical chest pain
b) A 25-year-old man with typical angina
c) A 45-year-old man with atypical chest pain
d) A 70-year-old man with atypical chest pain
View Answer
Answer and Discussion
The answer is d.
Objective: Identify the pretest probability of CAD.
Based on the Diamond and Forester estimate of pretest probability of disease, which is based on age, gender, and symptoms of chest pain, a 70-year-old man with atypical chest pain is likely to have a pretest probability of disease approximating 70%. Of note, the 25-year-old man with typical angina also would have a significant but slightly lower pretest probability of disease. A 45-year-old man with atypical chest pain would have a pretest probability of approximately 46%, whereas a woman of similar age with atypical symptoms would have a dramatically lower pretest probability of disease, estimated to be approximately 13% and reflecting the delayed onset of disease among the female population, which likely is related to the protective effect of estrogen prior to menopause.
Question 12
All of the following are indications for surgery in severe chronic mitral regurgitation (MR), except
a) Shortness of breath on exertion
b) LV ejection fraction (EF) of 45%
c) Dilated left ventricle (end-systolic dimension of 5 cm)
d) Frequent ventricular ectopy
e) Recurrent atrial fibrillation
View Answer
Answer and Discussion
The answer is d.
Objective: Identify the indications for surgery in the treatment of severe chronic MR.
In severe MR, repair/replacement is indicated with New York Heart Association (NYHA) class II-IV symptoms or in the absence of symptoms with decreased LV ejection fraction (LVEF) less than 60% or LV end-systolic dimension greater than 4 cm. Frequent ventricular ectopy is common and does not necessarily improve with surgery. It is not considered an indication for valve surgery in MR.
Question 13
Consider the following hemodynamic data: left atrial pressure, 25 mmHg; LV pressure, 120/10 mmHg; aortic pressure, 120/80 mmHg; and cardiac index, 1.9 L/minute/m2. These are most consistent with which valvular lesion?
a) Mitral stenosis (MS)
b) MR
c) Aortic stenosis
d) Aortic regurgitation (AR)
e) None of the above
View Answer
Answer and Discussion
The answer is a.
Objective: Understand the relevant hemodynamic parameters associated with valvular heart disease.
High left atrial pressure with a pressure gradient across the mitral valve in diastole and a low cardiac output is consistent with a diagnosis of MS.
Question 14
Recognized complications of isolated MS include all of the following, except
a) Atrial fibrillation
b) Pulmonary hypertension
c) Atrial thrombus
d) Right heart failure
e) LV enlargement
View Answer
Answer and Discussion
The answer is e.
Objective: Understand the natural history and complications associated with MS.
Isolated MS does not cause LV enlargement; left ventricle size is normal or small due to reduced inflow to the left ventricle.
Question 15
The following statements concerning surgical correction of MR are correct, except
a) Repair is most likely to be possible in rheumatic valves.
b) Repair has a lower complication rate than prosthetic replacement.
c) LV function declines more after prosthetic replacement than with repair.
d) Surgery is indicated in severe MR with symptomatic deterioration.
e) Men are more likely to require surgical correction of regurgitation than women.
View Answer
Answer and Discussion
The answer is a.
Objective: Understand indications for surgical correction of MR, as well as the surgical limitations of the treatment of MR.
Mitral valve repair is considered superior to replacement in most patients meeting criteria for surgical correction. Mitral
valve repair is most likely to be successful in mitral valve prolapse (MVP) and least likely in rheumatic disease and endocarditis. Mitral valve repair in ischemic and functional MR is also less beneficial.
valve repair is most likely to be successful in mitral valve prolapse (MVP) and least likely in rheumatic disease and endocarditis. Mitral valve repair in ischemic and functional MR is also less beneficial.
Question 16
Common symptoms of aortic stenosis include all of the following, except
a) Dyspnea
b) Syncope
c) Ankle edema
d) Angina
e) Fatigue
View Answer
Answer and Discussion
The answer is c.
Objective: Identify the common symptoms and manifestations of aortic stenosis.
The cardinal features of symptomatic aortic stenosis are heart failure, syncope, and angina. Other common findings are dyspnea on exertion, decreased exercise tolerance, and dizziness. Ankle edema and other signs of right heart failure are uncommon in aortic stenosis.
Question 17
The most reliable physical finding in predicting severe aortic stenosis is
a) Loudness of the murmur
b) Absent first heart sound
c) Loud second heart sound
d) Delayed carotid upstroke
e) Palpable fourth heart sound
View Answer
Answer and Discussion
The answer is d.
Objective: Understand the physical examination findings found in aortic stenosis.
All of the choices with the exception of absent first heart sound can be found in aortic stenosis (first heart sound is usually normal). However, delayed carotid upstroke is the most reliable predictor of severe aortic stenosis. Examination findings can be reliably used to confirm the suspicion of aortic stenosis, but echocardiography is still needed to exclude the diagnosis unequivocally.
Question 18
Surgical intervention is indicated in severe aortic stenosis for all of the following, except
a) Recent exercise-induced syncope
b) LV EF of 45% with normal coronary vessels
c) Shortness of breath on walking two blocks
d) Associated significant AR
e) Exertional chest pain usually relieved by rest
View Answer
Answer and Discussion
The answer is d.
Objective: Identify the indications for surgery in the treatment of severe aortic stenosis.
AR does not affect the decision regarding surgery in aortic stenosis. Surgery is indicated for symptomatic severe aortic stenosis, severe aortic stenosis undergoing coronary artery bypass grafting or other surgical procedure on the aorta or cardiac valves, and severe aortic stenosis with an EF less than 50%. Untreated, these patients have decreased 2-year survival rates and higher likelihood of sudden cardiac death.
Question 19
Consider the following hemodynamic data: left atrial pressure, 15 mmHg; LV pressure, 220/15 mmHg; aortic pressure, 100/60 mmHg; and cardiac index, 1.9 L/minute/m2. These are most consistent with which valvular lesion?
a) Tricuspid stenosis
b) MS
c) Aortic stenosis
d) AR
e) Tricuspid regurgitation
View Answer
Answer and Discussion
The answer is c.
Objective: Understand relevant hemodynamic parameters associated with valvular heart disease.
Low cardiac output and a large pressure gradient between the left ventricle and aorta during systole suggest the diagnosis of aortic stenosis.
Question 20
Indications for surgical treatment in severe AR include the following, except
a) LV EF of 53%
b) Increasing LV size on sequential echo (LV end-systolic dimension of 6 cm)
c) Shortness of breath
d) Aortic root size >6 cm
e) Anginal chest pain
View Answer
Answer and Discussion
The answer is a.
Objective: Identify the indications for surgery in the treatment of severe AR.
Replacement/repair of the aortic valve is indicated when symptoms are present. Asymptomatic patients should have surgical treatment when there is a reduced LV EF less than 50%, or if they have aortic root dilatation, or progressive LV dilatation on serial ECHOs.
Question 21
A 27-year-old woman has recent onset of shortness of breath going upstairs and a history of palpitations. Physical examination reveals a regular pulse, a loud S1, and an apical diastolic murmur. The most likely diagnosis is
a) Aortic stenosis
b) MS
c) AR
d) Tricuspid stenosis
e) None of the above
View Answer
Answer and Discussion
The answer is b.
Objective: Understand the physical examination findings seen in MS.
The physical findings associated with MS can be subtle, but in addition to clinical history can help in making a diagnosis that is confirmed by echocardiography. A loud S1 and an apical diastolic murmur that is low-pitched are classic findings. Pink to purple colored patches (termed mitral facies) and signs of right-sided congestive heart failure can also be seen.
Question 22
A 36-year-old man presents to the ER with sudden onset of atrial fibrillation. He is hemodynamically stable but has a systolic murmur at the left upper sternal border radiating to the back, a widely fixed split second heart sound, and a diastolic flow rumble along the right lower sternal border. The most likely diagnosis is
a) Ventricular septal defect (VSD)
b) Atrial septal defect (ASD)
c) Pulmonic stenosis (PS)
d) Aortic stenosis
View Answer
Answer and Discussion
The answer is b.
Objective: Understand commonly seen congenital heart disease findings and presentations.
ASD commonly presents in the adult, and the first symptom may be the sudden onset of atrial flutter or atrial fibrillation. At least 12% to 15% of adult patients have atrial fibrillation preoperatively. Physical findings that demonstrate this as an ASD are the murmur of increased pulmonary blood flow at the left upper sternal border radiating to the back, the pathognomonic finding of a fixed split-second heart sound, and the diastolic flow rumble along the right mid-right lower sternal border (functional tricuspid stenosis), which suggests that this patient has a large left-to-right shunt at the atrial level. Adult patients with ASD tend to have large defects that raise the question of whether somewhat smaller defects in childhood actually get stretched and become larger defects in adults with significant left-to-right shunts. ASDs are also more common in women, with a female-to-male ratio of 2 to 3:1.
Question 23
A 22-year-old professional female basketball player was noted to have an unusual murmur on her sports physical before the season began. The doctor thought he heard a continuous murmur at the left upper sternal border associated with a slightly widened pulse pressure and brisk to abounding pulses. The most likely diagnosis is
a) VSD
b) ASD
c) Coarctation of the aorta
d) Patent ductus arteriosus (PDA)
View Answer
Answer and Discussion
The answer is d.
Objective: Understand commonly seen congenital heart disease findings and presentations.
Many adult patients with patent ductus are asymptomatic, depending on the size of the left-to-right shunt and the size of the ductus. Frequently, the condition is discovered by the unusual quality of a continuous murmur at the left upper sternal border that can sound like an innocent venous hum. Because a patent ductus is an aortopulmonary runoff; however, the pulse pressure frequently is widened, and the pulses are brisk to bounding. Today, most lesions of ductus can be closed in the catheterization laboratory without surgery.
Question 24
A 32-year-old woman is noted to have a systolic blood pressure (BP) of 170/100 mmHg. She has a prominent aortic ejection click and murmurs heard over the ribs on both sides anteriorly and over the back posteriorly. In addition, no pulses are palpable in the lower extremities, and she complains of mild claudication with exertion. The most likely diagnosis is
a) ASD
b) Aortic stenosis
c) Coarctation of the aorta
d) VSD
View Answer
Answer and Discussion
The answer is c.
Objective: Understand commonly seen congenital heart disease findings and presentations.
Adult patients with coarctation almost always present with systolic hypertension, and diastolic hypertension may occasionally be seen as well. A bicuspid aortic valve is noted in a significant proportion of patients with coarctation; therefore, an aortic ejection click may be heard. These patients frequently have collateral murmurs from intercostal arteries heard over the anterior and posterior chest as well as increased collaterals from the thyrocervical trunk. The pulses in the lower extremity may be weak to absent. If the coarctation is severe enough, the individuals may complain of claudication with exercise. The approach to correction in adult patients is usually percutaneous stent placement.
Question 25
A 42-year-old man presents for his first visit to your clinic. He has always been cyanotic, clubbed, and physically restricted. His hematocrit is 68%, with a hemoglobin level of 24 g. He has never undergone surgery, and his oxygen saturation on room air is 62%. Cardiac catheterization demonstrates a large VSD, overriding aorta, and severe calcification of the entire right ventricular outflow tract with small pulmonary arteries bilaterally. The diagnosis in this patient is
a) Double-outlet right ventricle
b) Truncus arteriosus
c) Tetralogy of Fallot (TOF)
d) Atrioventricular (AV) canal
View Answer
Answer and Discussion
The answer is c.
Objective: Understand commonly seen congenital heart disease findings and presentations.
TOF is the most common form of cyanotic congenital heart disease in adolescents and adults. The hallmark of tetralogy is severe valvular and subvalvular PS associated with a large VSD. Patients shunt right to left at the ventricular level; therefore, they are cyanotic and clubbed. In addition, cyanotic patients are polycythemic; once their hematocrit is > 65%, they are at increased risk for stroke or spontaneous cerebral hemorrhage. The approach to tetralogy is surgical, with relief of the right ventricular outflow tract obstruction and closure of the VSD.
Question 26
A 30-year-old woman presents to your office with the murmur of MR. She has been known to have a complete heart block since childhood and is now somewhat fatigued and short of breath. You notice that on her chest radiograph she has a completely straight left heart border. The most likely diagnosis in this patient is
a) VSD
b) Rheumatic MR
c) Corrected transposition of the great arteries
d) PDA
View Answer
Answer and Discussion
The answer is c.
Objective: Understand commonly seen congenital heart disease findings and presentations.
Patients with congenitally corrected transposition frequently present as adults. Although a morphologic right atrium is connected to a morphologic left ventricle via the mitral valve, the blood flows from that ventricle to the pulmonary artery. It returns then to a morphologic left atrium, which crosses a tricuspid valve into a morphologic right ventricle that pumps blood out the aorta, and the aorta is anterior and to the left. Patients with this condition frequently present in adulthood because the blood is flowing from inverted ventricles but out the appropriate arteries. Patients with corrected transposition, however, are either born with complete heart block or develop heart block at a rate of 2% per year. In addition, they often have VSD and PS. The chest radiograph shows a completely straight left heart border because of the anterior and leftward position of the aorta. Patients also frequently have an Ebsteinlike malformation of the left-sided AV valve (tricuspid valve), and that valve is frequently regurgitant.
Question 27
A 28-year-old man has been known to have Wolff-Parkinson-White syndrome with episodes of supraventricular tachycardia. You order a chest radiograph and are surprised at the significant cardiomegaly, with what appears to be marked right atrial enlargement. The patient also has a murmur of tricuspid regurgitation. The most likely diagnosis is
a) ASD
b) VSD
c) Tricuspid stenosis
d) Ebstein anomaly
View Answer
Answer and Discussion
The answer is d.
Objective: Understand commonly seen congenital heart disease findings and presentations.
Ebstein anomaly is the only congenital cardiac defect commonly associated with preexcitation syndromes like Wolff-Parkinson-White. Patients frequently have significant tricuspid regurgitation with a markedly dilated right atrium. Ebstein patients are prone to all rhythm disorders, including both atrial and ventricular arrhythmias, and they have a significant incidence of sudden death.
Question 28
Which of the following statements is incorrect after acute myocardial infarction (MI)?
a) Even during an acute MI, angiography remains safe to perform.
b) More than 85% of infarct-related arteries are totally occluded during the acute phase of ST segment elevation MI (STEMI).
c) The incidence of totally occluded infarct vessels decreases with time after STEMI secondary to spontaneous fibrinolysis.
d) Most patients who die from an acute MI have advanced coronary atherosclerosis involving significant obstruction in at least one coronary artery.
e) None of the above
View Answer
Answer and Discussion
The answer is e.
Objective: Understand the natural history of acute MI and its evaluation.
During an acute MI, angiography remains safe, with primary percutaneous coronary intervention (PCI) often considered
the appropriate treatment. Of importance, most infarct-related arteries are occluded during the acute STEMI phase. This is reduced after infarction secondary to spontaneous fibrinolysis. Most patients who die of an acute infarction have advanced coronary atherosclerosis involving a significant coronary obstruction in at least one coronary artery.
the appropriate treatment. Of importance, most infarct-related arteries are occluded during the acute STEMI phase. This is reduced after infarction secondary to spontaneous fibrinolysis. Most patients who die of an acute infarction have advanced coronary atherosclerosis involving a significant coronary obstruction in at least one coronary artery.
Question 29
Which of the following statements concerning risk stratification after an acute MI is not correct?
a) Women possess an improved postinfarction prognosis compared with that of men.
b) The single most important determinant of both short- and long-term survival is the residual LV systolic function.
c) Silent ischemia, as detected by Holter monitoring, has a similar prognosis to that of symptomatic ischemia after infarction.
d) Diabetes mellitus contributes to an increased postinfarction risk.
View Answer
Answer and Discussion
The answer is a.
Objective: Understand the role of risk stratification on prognosticating outcome after acute MI.
Important adverse prognostic predictors after an MI include the extent of LV systolic dysfunction and coexistent morbidity, including diabetes mellitus. Silent ischemia, as detected at Holter monitoring, portends a worse prognosis, as does being of female gender.
Question 30
The following items are features of non-ST elevation MI (NSTEMI), except
a) The residual coronary artery stenosis generally is severe.
b) Prominent collaterals serve the infarct-related artery.
c) A greater likelihood of a previous infarction exists.
d) Recurrent infarction is less likely compared with STEMI patients.
View Answer
Answer and Discussion
The answer is d.
Objective: Understand the features of NSTEMI.
NSTEMI are characterized by the residual, high-grade coronary stenosis, prominent collaterals, and greater likelihood of previous MI. The EF is lower, but the reinfarction rate is higher compared with that in patients with STEMI.
Question 31
The following statements regarding fibrinolytic therapy are true, except
a) An improved mortality has been shown in patients with inferior infarction after fibrinolytic administration.
b) The earlier the fibrinolytic treatment is administered, the greater the impact on survival.
c) Preservation of LV function depends on early fibrinolytic administration.
d) Cardiopulmonary resuscitation is an absolute contraindication for fibrinolytic therapy.
View Answer
Answer and Discussion
The answer is d.
Objective: Understand the usage, outcomes, and contraindications of fibrinolytics in the treatment of acute MI.
Fibrinolytic therapy is most beneficial within the early phases of an acute MI. Its use is primarily reserved for situations where access to primary PCI is not available in a timely fashion. Reduced morbidity and mortality is shown for all infarction, including inferior infarction. Enhanced LV systolic function is noted with earlier fibrinolytic administration. Cardiopulmonary resuscitation remains a relative, not an absolute, contraindication to fibrinolytic therapy.
Question 32
You are called to see a patient whose cardiac monitor reveals bradycardia. Indications for a temporary pacemaker in patients with acute MI include the following, except
a) New left anterior fascicular and right bundle-branch block
b) New second-degree Mobitz type I AV block responsive to atropine administration
c) New left bundle-branch block with first degree AV block
d) Complete heart block
View Answer
Answer and Discussion
The answer is b.
Objective: Understand the complications encountered after acute MI.
It is important to consider that bradycardia can further decrease myocardial perfusion and temporary pacing may be required. Indications for temporary pacing during an acute MI include new-onset bifascicular block, second-degree Mobitz type II AV block, and complete heart block. First-degree AV block and Mobitz type I Wenckebach second-degree AV block require careful observation but not temporary pacing.
Question 33
True statements concerning the ECG findings during an acute MI include the following, except
a) Sinus tachycardia is frequently present.
b) An accelerated idioventricular rhythm postfibrinolytic therapy warrants urgent electric cardioversion.
c) Atrial dysrhythmias such as atrial fibrillation are commonly observed.
d) The development of complete heart block portends a worse prognosis.
View Answer
Answer and Discussion
The answer is b.
Objective: Understand the ECG findings associated with an acute MI.
In the presence of an acute MI, increased sympathetic tone often is reflected in the form of sinus tachycardia. Atrial arrhythmias frequently are demonstrated in part related to atrial ischemia, increased circulating catecholamines, acutely elevated intracardiac pressures, and cardiac chamber dilatation. Advanced forms of heart block are associated with larger infarction, which portend a worse prognosis. Accelerated idioventricular rhythms frequently manifest after successful reperfusion during the acute myocardial injury phase, rarely require treatment other than careful observation, and represent a noninvasive marker of successful coronary blood flow restoration.
Question 34
In a patient presenting with an acute coronary syndrome (ACS) and an ECG demonstrating an extensive anterolateral myocardial injury pattern, appropriate treatment measures would include the following, except
a) The prophylactic placement of an intra-aortic balloon pump to attenuate the degree of myocardial injury given the large MI
b) Intravenous fibrinolytic therapy
c) Intravenous β-blocker administration in the absence of advanced heart failure and hemodynamic compromise
d) An urgent coronary angiography with the goal of performing a PCI and possible coronary stent placement
View Answer
Answer and Discussion
The answer is a.
Objective: Understand the treatment of acute MI.
In the presence of an acute chest discomfort syndrome and an ECG demonstrating acute myocardial injury, the restoration of coronary artery blood flow in the most expedient manner results in reduced morbidity and mortality. This can be achieved by administering intravenous fibrinolytic therapy or proceeding directly with coronary angiography and PCI. β-Blockers reduce myocardial oxygen demand, attenuate myocardial ischemia, and limit the size of an infarction. β-Blockers should be administered to all acute MI patients in the absence of a hemodynamic contraindication. In the presence of cardiogenic shock, drug-refractory congestive heart failure, and recurrent life-threatening cardiac dysrhythmias believed to be ischemia-mediated, the placement of an intra-aortic balloon pump in the peri-infarction period can achieve a positive clinical benefit. The routine use of an intra-aortic balloon pump is not indicated and may subject the patient to excess morbidity secondary to vascular injury, cholesterol and systemic embolization, and infection, all without a tangible benefit. The use of an intra-aortic balloon pump is an individualized decision for each acute MI patient.
Question 35
A 60-year-old Asian man is referred to you for evaluation of a heart murmur. He speaks no English and is not accompanied by any family member able to translate. As you wait for the translator to arrive, you are able to communicate sufficiently to obtain permission for a physical examination. His pulse is regular, with a rate of 80 beats/minute, and his BP is 100/85 mmHg. Carotid pulse has a slow upstroke. No jugular venous distension is present. The apex is slightly displaced laterally. A systolic thrill is palpable over the aortic area and carotids. Auscultation reveals a harsh ejection systolic murmur. Valsalva maneuver does not accentuate the murmur. The second aortic sound is soft. With which of the following are these findings most consistent?
a) MR
b) MVP
c) Aortic stenosis
d) Hypertrophic obstructive cardiomyopathy (HOCM)
e) MS
View Answer




Answer and Discussion
The answer is c.
Objective: Understand the clinical findings associated with valvular heart disease.
All the signs and symptoms in this case point to aortic stenosis. This is a systolic murmur, which eliminates MS. The murmur of HOCM is increased with Valsalva maneuver. Neither MR nor MVP is associated with narrowed pulse pressure or slow upstroke.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree