Fig. 15.1
(a) Bladder lesion. (b) Bipolar resectoscope. (c) Post transurethral resection image
15.5 Partial Cystectomy
Partial cystectomy provides a feasible approach in a select group of bladder cancer patients who meet certain qualifying criteria. Though it does maintain a conventional voiding mechanism and erectile function, not all patients are appropriate candidates. Patients with urachal carcinoma, solitary tumor located in a bladder diverticulum, dome, or posterolateral aspect of the bladder are optimal candidates assuming there is no evidence of carcinoma in situ (CIS) elsewhere in the bladder at time of random bladder biopsies. Transurethral prostatic biopsies are recommended to complete the staging process. There should be enough space to allow for wide excision without need for ureteral reimplantation. Partial cystectomy allows for a full thickness resection of the diseased bladder, with adequate negative margins, as well as a concomitant pelvic lymph node dissection. Kassouf and colleagues reported that only 5 out of 37 patients who underwent partial cystectomy subsequently required a radical cystectomy. Of these five patients, only one patient died of bladder cancer with a median of 37 months of follow-up from the time of delayed cystectomy [9]. Patients undergoing partial cystectomy must understand that they must be compliant for lifelong cystoscopic evaluation if they choose this treatment option. The gold standard for performing partial cystectomy is the open surgical approach. However, recent advances in minimally invasive surgery may allow for a laparoscopic or robotic resection of a portion of the bladder.
15.6 Technique for Open Partial Cystectomy
The patient is placed in supine position with slight Trendelenburg and the abdomen and genitalia are prepped and draped giving access to the genitalia for sterile Foley catheter placement, which should be placed within the sterile surgical field. A regional or general anesthetic approach may be used for the procedure. All visible bladder tumors should always be resected prior to consideration for partial cystectomy. This is to minimize any risk of tumor spillage. The bladder may be accessed via a transperitoneal or extraperitoneal approach. If the lesion or diverticulum is posterior, a transperitoneal approach is suggested. Sometimes, if there is a possibility for difficult identification of the tumor site at time of resection, cystoscopic marking with either fulguration or dye should be considered at the time of surgery. A low vertical midline incision is used to enter the peritoneal cavity. Of note, a Maylard incision may be considered if the patient has strong reservations against a midline incision. Once the peritoneal cavity is entered, a pelvic lymph node dissection can be performed in the standard fashion. To aid in the dissection of the bladder, it may help to fill the bladder slightly with sterile water and clamp the Foley catheter. Overly distending the bladder may make it more susceptible to perforation at time of dissection.
It is important to quickly identify anatomic landmarks that help in the further mobilization of the bladder and facilitate partial cystectomy. The medial umbilical ligament can be followed to the superior vesical artery. The artery can then be ligated on the side of the bladder lesion. This will help further mobilize the bladder. The vas deferens on that side may be identified and mobilized or transected as needed. It is recommended that the perivesical fat directly over the suspected tumor area remain attached to the bladder. If the lesion is on the posterior wall, the peritoneum overlying the posterior bladder may be incised. This will allow the rectum to be mobilized off the bladder, if needed giving access to the posterior wall. All adjacent bowel contents should be packed away so as to avoid any contamination from spillage. Once the bowel is packed away from the field surrounding the bladder, the bladder is evaluated and the tumor location is verified. This can be accomplished via manual palpation or with concomitant cystoscopy. If cystoscopy is needed, the Foley catheter should be removed in a manner to avoid tumor spillage.
Once the site of the tumor has been verified, 2–0 delayed absorbable sutures are placed to help elevate the bladder at time of cystotomy and partial cystectomy. The Foley catheter has been unclamped and the bladder has been completely drained at this point. The bladder is incised and the tumor is removed with an approximate 2 cm margin is excised. Special care should be paid to the location of the ureteral orifices. Frozen biopsies at the margin sites are suggested if there are any questions at the time of resection. A standard two-layer closure with a 2–0 delayed absorbable suture is recommended. The bladder may be filled with 150–200 cc of sterile water to confirm a watertight closure. Once the stay sutures have been removed, and the Foley catheter is draining appropriately, an abdominal drain is placed in a dependent location of the pelvis. The drain should stay in for at least 5–7 days and output should be monitored prior to its removal at an outpatient setting. Since the closed suction drain is intraperitoneal and there is concern regarding the amount of fluid present in the drain, a creatinine level of the drain fluid should be obtained. The Foley catheter should stay in place for at least 1 week. A cystogram is performed prior to removal of the catheter to check for any contrast extravasation.
15.7 Robot Assisted Partial Cystectomy
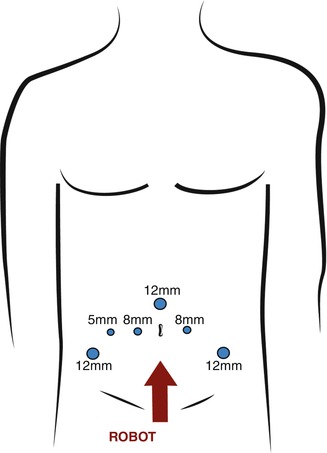
The technique for robot assisted partial cystectomy shares a similar trocar set up with techniques for robot assisted radical cystectomy [10] (Fig. 15.2). Once general anesthesia is adequate, a Foley catheter and orogastric tube is placed. The patient is placed in a modified low lithotomy position and the operating table is placed in steep Trendelenburg position. Special care is given to adequately pad and secure the patient to avoid any movement of the patient while the robot is docked. This will prevent pressure related complications. The abdomen is shaved, prepped, and draped in the standard fashion. Access and insufflation techniques are per surgeon preference. At our institution, unless there is a significant history of multiple abdominal surgeries and risk of bowel adhesions, the Veress needle is placed in a supraumbilical incision and a 12 mm blunt dilating trocar is placed through the same incision. If there is any worry about midline adhesions, an off site entry is performed. The off set teaching laparoscope is used to perform lysis of adhesions when multiple ports are not feasible secondary to multiple intestinal adhesions to aid in proper dissection.