Fig. 4.1
Pneumoflator
A system that emits a light source. A fiber-optic light bundle. Illumination is provided by a high intensity but “cold” broadband light source.
Energy Sources (Fig. 4.2)

Fig. 4.2
Energy sources: LigaSure™ (top) (Courtesy of Covidien, Dublin, Ireland), UltraCision Harmonic (center) (Courtesy of Ethicon Endo-Surgery, Blue Ash, OH, USA), and Thunderbeat (bottom) (Courtesy of Olympus, Center Valley, PA, USA)
Electrosurgery to perform a cauterization of the structures. It could be by monopolar or bipolar electrode. Today, the best advance in electrosurgery is the LigaSure™ system (Covidien, Dublin, Ireland); it incorporates a microcomputer that allows correct vessel ligation according to the thickness of the structures.
Ultrasonic energy (UltraCision Harmonic, Ethicon Endo-Surgery, Blue Ash, OH, USA): This makes a correct dissection by cavitation of the structures. It is able to perform a vessel ligation ultrasonically.
Today, there are instruments that combine these two types of energies: Thunderbeat (Olympus, Center Valley, PA, USA), integration of ultrasonic and advanced bipolar energies delivered through a single multifunctional instrument, allowing a surgeon to simultaneously seal and cut vessels up to and including 7 mm in size with minimal thermal spread.
Trocars and Laparoscopic Dissecting and Grasping Instruments
Trocars (Fig. 4.3)

Fig. 4.3
Trocars (5 mm) and BTT trocar (Hasson)
In ventral hernia repair, the most frequently used trocars are two 5 mm trocars and one 10–12 mm trocar. When the mesh is very large, it could be useful to have a 15 mm trocar.
In inguinal hernia repair, we use two 5 mm trocars and one 10–12 mm trocar. There are many variations, according to the two main types of surgeries:
TAPP: 2 5 mm trocars and one 10 mm trocar, generally. But we can exchange the 10 mm trocar for a 5 mm trocar (optic) if we use a lightweight mesh, as it is able to handle a 5 mm trocar. We sometimes use a 3 mm trocar on the left side (for the nondominant hand) instead of the 5 mm trocar.
TEP: 2 5 mm trocars and two special trocars: BTT and PDB.
There is a device that combines the two special trocars into one: spacemaker, which allows the balloon dissection of the preperitoneal space (usually created by the PDB) and fixes the fascia with a miniballoon in order to maintain that newly created preperitoneal cavity (usually performed by the BTT).
Instruments
Endograspers (Endo Clinch™ and Endo Grasp™, Covidien, Dublin, Ireland), endoshears, and endodissectors are the main instruments in laparoscopic hernia repair. See Fig. 4.4.

Fig. 4.4
Different styles of graspers, shears, dissectors, and 30° optic in laparoscopy
Other instruments such as an endohook, the Endoloop® (Ethicon Endo-Surgery, Blue Ash, OH, USA), or the Endo Stitch™ (Covidien, Dublin, Ireland) could be used according to the characteristics of the hernia surgery. In single-port surgery, we use roticulator instruments such as the roticulator-endodissector.
Optics
5 mm optic: With inclined end, to offer 30°, or normal end that offers 0°
10 mm optic: 30° or 0°
Other optics: 3 mm optic 0° (its use is rare), roticulator optics in robotic and single-port surgery
See Fig. 4.5 a, b for the basic instruments used in laparoscopic hernia repair.


Fig. 4.5
(a, b) Basic instruments in laparoscopic hernia repair
Role of Triangulation Techniques and Ergonomics in Laparoscopic Surgery
There is no uniform consensus regarding port placement for advanced laparoscopic procedures. The placement of ports is currently dictated by the surgeon’s preference based on individual experience. To facilitate smooth instrument manipulation along with adequate visualization during laparoscopy, trocars usually are placed in triangular fashion. This is termed triangulation. See Fig. 4.6a.
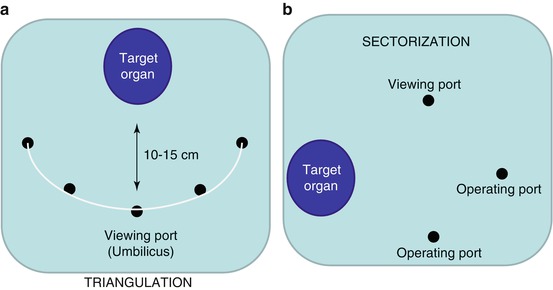
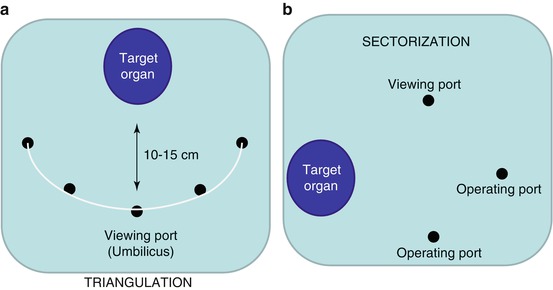
Fig. 4.6
(a, b) Triangulation (a) and sectorization (b) in laparoscopy
The target organ should be 15–20 cm from the central port used for placing the optical trocar [1]. Generally, the two remaining trocars are placed in the same 15–20 cm arc at 5–7 cm on either side of the optical trocar [2]. This allows the instrument to work at 60°–90° angles with the target tissue and to avoid problems of long handles due to port placement that is too distant or too close; it also avoids the problem of abdominal wall interference. If necessary, two more retracting ports can be placed in the same arc but more laterally so that instruments do not clash.
When the optical trocar is placed as one of the lateral port trocars, it is called sectorization. See Fig. 4.6b. Sectoring of instruments should be avoided by beginners since it requires a greater degree of understanding of laparoscopic views and significantly different one-eye coordination.
More specifically, there are ergonomic issues that are unique to laparoscopic hernia repair, such as the strain of working against the camera (mirror-image effect) and the complex movements required to repair hernia defects from underneath the anterior abdominal wall during ventral hernioplasty. The attention to the current operative environment and the selection of appropriate available instrumentation may improve operative efficiency and protect the health of the surgeon.
The etiology of the ergonomic problem in laparoscopy is multifactorial. Consideration should be given to instrumentation, image quality, the positioning of the patient, the surgical staff, and the equipment. Within the current ergonomic constraints of laparoscopy, changes can and should be made to increase the comfort of the surgeon and reduce muscular fatigue. Instrumentation should be selected not only for function but also for ease of use and proper individual surgical fit.
The operating table should be positioned so that the instrument handles are at the surgeon’s elbow level [3]. Similarly, the video monitor should be positioned at or slightly above eye level. Suspended mobile monitors may facilitate this adjustment. The monitor should be in alignment with the operative target and the surgeon. Foot pedals that control energy sources should be placed within a small radius from the surgeon’s feet to avoid stiffening and straining to maintain balance. Patient position is also crucial. The patient should be positioned to allow gravity to assist with operative exposure, reducing the exertion needed from the surgeon and assistants for retraction.
The patient’s arms should be tucked during ventral herniorrhaphy to provide freedom of movement by the surgeon and assistants around the operating table. Attention to these details in positioning and operative setup should greatly improve operative efficiency.
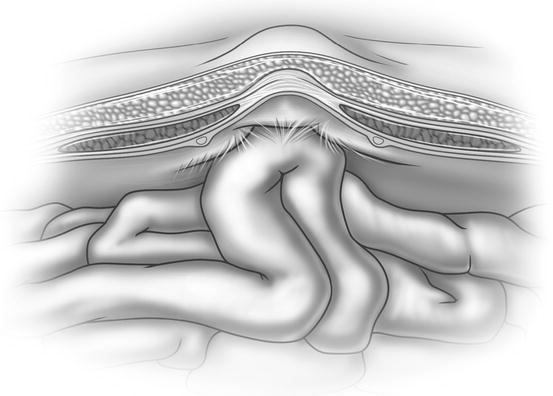
Incisional Ventral Hernia
It was in 1991 that the first laparoscopic approach in the repair of incisional hernia was reported. Since that time, there has been a steady acceptance of this procedure because of the improvement in the recovery of the patient, the decreased rates in wound complications and mesh infections, and the notable decline in the recurrence rate compared with that of the open technique. In general, all the significant steps of the two different approaches are similar. The laparoscopic approach may be more suitable for straightforward hernias, with open repair reserved for the more complex hernias. Laparoscopic ventral hernia repair appears to be an acceptable alternative that can be offered by surgeons proficient in advanced laparoscopic techniques [4]. See Fig. 4.7.