Are Renin-Angiotensin-Aldosterone System Blockers Friends or Foes of the Kidneys?
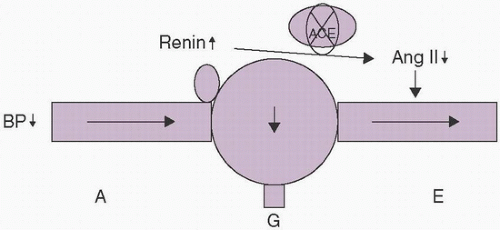
The renin-angiotensin-aldosterone system (RAAS) plays an important role in the regulation of systemic volume homeostasis and blood pressure (BP). The classic systemic RAAS is depicted in Figure 18.1. In addition, there is an intrarenal RAAS that controls glomerular capillary pressure and glomerular filtration (Fig. 18.2). There is also evolving evidence for the existence of an intracellular RAAS, as angiotensin II (Ang II) and aldosterone are capable of stimulating various cellular processes, including growth factors and reactive oxygen species, which can lead to fibrosis (Leehey et al., 2006; Bertocchio et al., 2011).
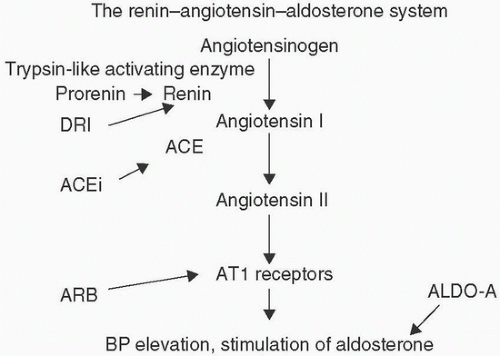 FIGURE 18.1 The systemic RAAS depicting the site of action of direct renin inhibitors (DRIs), ACE inhibitors (ACEis), ARBs, and aldosterone antagonists (ALDO-As). |
Experimental work in the 1980s provided evidence that blockade of the RAAS with angiotensin-converting enzyme (ACE) inhibitors could prevent glomerulosclerosis and progressive renal failure in animal models of kidney disease, and in particular, diabetic kidney disease (Zatz et al., 1986). These observations were followed by clinical trials suggesting a renoprotective effect of ACE inhibitors, which is, at least in part, independent of their effects on BP (Lewis et al., 1993). The mechanism of renal benefit may be explained by the observation that Ang II can preferentially constrict the efferent versus the afferent arterioles in the kidney; prevention of Ang II formation or action therefore decreases glomerular capillary pressure (Fig. 18.2). A hemodynamically mediated renoprotective effect of RAAS blockers is suggested from observations that these agents appear to preferentially decrease proteinuria when compared to other antihypertensive agents. A decrease in proteinuria has been used as surrogate of renal protection in many studies, as interventions that decrease proteinuria generally result in more favorable renal outcomes. However, there are exceptions to this, which can particularly be seen in studies where combined RAAS blockade was utilized for the treatment of diabetic kidney disease. For instance, in the Veterans Affairs Nephropathy in Diabetes Trial (VA NEPHRON-D) trial, dual RAAS blockade with the ACE inhibitor lisinopril and the angiotensin receptor blocker (ARB) losartan decreased proteinuria more than monotherapy with losartan alone; however, this did not lead to a statistically significant reduction in hard renal endpoints and was associated with a greater risk of adverse events including AKI and hyperkalemia (Fried et al., 2013).
Clinical trials comparing RAAS blockers to other antihypertensive agents have generally reported lower BPs in patients treated with RAAS
blockers. An exception was the Irbesartan Diabetic Nephropathy Trial (IDN) study, in which the ARB irbesartan was compared to amlodipine, a dihydropyridine calcium channel blocker (Lewis et al., 2001). In this study, despite similar BP control in the two arms, patients receiving the ARB had better renal outcomes. However, it should be pointed out that dihydropyridine calcium channel blockers can increase glomerular capillary pressure because of dilation of the afferent arteriole. Thus, a possible interpretation of the IDNT study is that calcium blockers have adverse renal effects rather than RAAS inhibitors having beneficial renal effects. In a recent meta-analysis, it was reported that RAAS blockers do not prolong survival in patients with diabetic kidney disease; however, they did appear to decrease end-stage kidney disease (Palmer et al., 2015).
blockers. An exception was the Irbesartan Diabetic Nephropathy Trial (IDN) study, in which the ARB irbesartan was compared to amlodipine, a dihydropyridine calcium channel blocker (Lewis et al., 2001). In this study, despite similar BP control in the two arms, patients receiving the ARB had better renal outcomes. However, it should be pointed out that dihydropyridine calcium channel blockers can increase glomerular capillary pressure because of dilation of the afferent arteriole. Thus, a possible interpretation of the IDNT study is that calcium blockers have adverse renal effects rather than RAAS inhibitors having beneficial renal effects. In a recent meta-analysis, it was reported that RAAS blockers do not prolong survival in patients with diabetic kidney disease; however, they did appear to decrease end-stage kidney disease (Palmer et al., 2015).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree