ESSENTIALS OF DIAGNOSIS
ESSENTIALS OF DIAGNOSIS
Jaundice is most often caused by decompensation of preexisting chronic liver disease, alcoholic hepatitis, and gallstone disease.
Careful history, physical examination, and routine laboratory tests lead to accurate diagnosis in 85% of patients with jaundice.
Cirrhosis can be diagnosed on the basis of two physical findings (asterixis, ascites) and two laboratory findings (decreased serum albumin [<2.8 g/dL], prolonged prothrombin time [INR >1.6]).
Dilated intrahepatic bile ducts indicate obstruction from extrahepatic causes (stone, structure, tumor).
Absence of dilated ducts in jaundiced patients with serum bilirubin >10 mg/dL suggests intrahepatic cholestasis.
Sepsis, drugs, sickle cell disease, and chronic hepatitis are the most common causes of intrahepatic cholestasis.
GENERAL CONSIDERATIONS
Jaundice refers to the yellowish discoloration of tissue resulting from the deposition of bilirubin in tissues; this indicates that the serum bilirubin is likely 3 mg/dL or higher. Jaundice most often is the result of acute or chronic liver disease, or biliary tract disease, and less commonly the result of hemolytic disorders. The differential diagnosis of jaundice has changed significantly in the past decade due largely to a sharp decline in the incidence of viral hepatitis types A and B as a result of immunization. The most common causes of jaundice in the adult population now are decompensation of preexisting chronic liver disease, alcoholic hepatitis, sepsis and abnormal hemodynamic conditions, and gallstone disease.
PATHOGENESIS
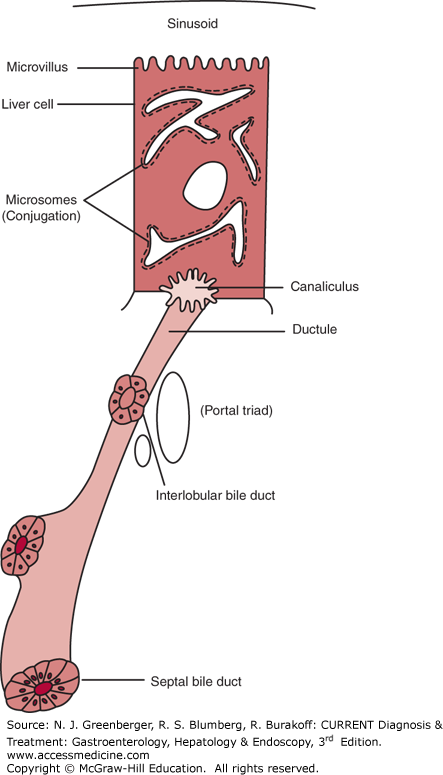
Jaundice can occur as a result of acute or chronic parenchymal liver disease, extrahepatic biliary tract obstruction (due to stone, stricture, or tumor), intrahepatic cholestasis (having several causes, as detailed in the following text), and hemolytic anemia. Serum bilirubin derives from the degradation of senescent red cells in the reticuloendothelial system. Each day a normal individual destroys 50 mL of red blood cells, which gives rise to 7.5 g of hemoglobin. Each gram of hemoglobin that is degraded results in production of 35 mg of bilirubin. Unconjugated bilirubin is liquid soluble, water insoluble, and hence circulates bound to albumin. The hepatic processing of bilirubin involves uptake of unconjugated bilirubin, conjugation with uridine diphosphate glucuronyl transferase, transfer to the bile canaliculus, and excretion into the intrahepatic biliary tree (Figure 38–1). Bilirubin is excreted in the bile primarily as bilirubin diglucuronide (80%), bilirubin monoglucuronide (20%), and unconjugated bilirubin (<1%). Any disease process that results in an increased load of unconjugated bilirubin presented to the liver, impaired conjugation, or impaired excretion of conjugated bilirubin, either intrahepatic or extrahepatic, can lead to accumulation of bilirubin in the blood, resulting in jaundice.
CLINICAL FINDINGS
On the basis of a detailed history and a carefully conducted physical examination, along with the routine liver tests summarized in the following text, the examiner should be able to formulate a differential diagnosis and be correct in over 85% of the patients who present with jaundice and evidence of liver disease. The importance of a careful history and physical examination along with critical evaluation of the standard liver tests cannot be overemphasized.
Table 38–1 summarizes the specific information to be obtained from patients with jaundice or liver disease. The information is grouped into that relating to viral hepatitis, medications, alcohol use, and miscellaneous relevant information.
Viral hepatitis Ask about: Blood transfusion (especially if before 1990) Intravenous drug use Sexual practices: • Anal-receptive intercourse • Sex with a prostitute • History of sexually transmitted disease • Multiple sexual partners (>5/y) • Intercourse with persons infected with hepatitis B or C Contact with persons with jaundice Changes in taste and smell Needlestick exposure Work in renal dialysis units Work in trauma units, operating rooms, or other settings in which exposure to users of IV drugs may occur Shared razors or toothbrushes Body piercing (ears, nose) Tattoos Intranasal cocaine use Special risk factors for hepatitis A: No immunization (older adults) • Travel to endemic areas • Exposure in settings where clusters of hepatitis may occur (eg, institutions) Medication use Review: All prescription medications Ask specifically about: All over-the-counter drugs Vitamins (especially vitamin A) Any foods, herbal preparations, or home remedies purchased in a health food store Alcohol use Obtain detailed quantitative history of both recent and previous alcohol use from patient and family members Ask whether patient has experienced withdrawal symptoms, or has been cited for driving-under-the-influence Miscellaneous information Ask about: Pruritus (suggests cholestasis either intrahepatic or extrahepatic) Evaluation of jaundice (dark urine, light stools) Recent changes in menstrual cycle (amenorrhea suggests chronic liver disease, often cirrhosis) Review: History of anemia, sickle cell disease, known hemoglobinopathy, artificial heart valves Symptoms suggestive of biliary colic, chronic cholecystitis Family history of liver disease, gallbladder disease |
Table 38–2 summarizes characteristic findings on physical examination in patients with jaundice. Attention should be paid to the peripheral stigmata of liver disease, including spider angioma, which characteristically occurs above the clavicles in the distribution of the superior vena cava. More than 15 spider angiomata indicate the presence of significant liver disease and likely portal hypertension. The triad of gynecomastia, Dupuytren contracture, and parotid enlargement is a clear indication that alcohol is the most likely cause of the patient’s liver disease. Splenomegaly, ascites, and prominent abdominal collateral veins indicate the presence of portal hypertension and in all likelihood the presence of esophageal or gastric varices, or both. Hepatic encephalopathy is suggested by the presence of asterixis and behavioral alterations.
General inspection Scleral icterus Pallor Wasting Needle tracts Evidence of skin excoriations Ecchymosis or petechiae Muscle tenderness and weakness Lymphadenopathy Evidence of pneumonia Evidence of congestive heart failure Peripheral stigmata of liver disease Spider angiomata Palmar erythema Gynecomastia Dupuytren contracture Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|